Table of Contents
1. Introduction
In the evolving landscape of medical treatment for metabolic disorders and hormonal imbalances, semaglutide emerges as a beacon of hope for those battling the dual challenges of obesity and type 2 diabetes. This groundbreaking medication, a GLP-1 receptor agonist, not only revolutionizes the approach to managing these conditions but also piques interest for its potential implications on another crucial aspect of health: testosterone levels. The interplay between semaglutide and testosterone levels embodies a complex, yet fascinating area of study that could redefine treatment paradigms for patients worldwide.
Semaglutide’s journey from a diabetes management tool to a weight loss aid highlights its versatility and effectiveness. Originally approved for the treatment of type 2 diabetes, semaglutide works by mimicking the action of GLP-1, a hormone involved in blood sugar regulation and appetite control. Its ability to lower blood sugar levels and promote weight loss has garnered attention not only from the medical community but also from those struggling with obesity—a condition intricately linked with diminished testosterone levels in men.
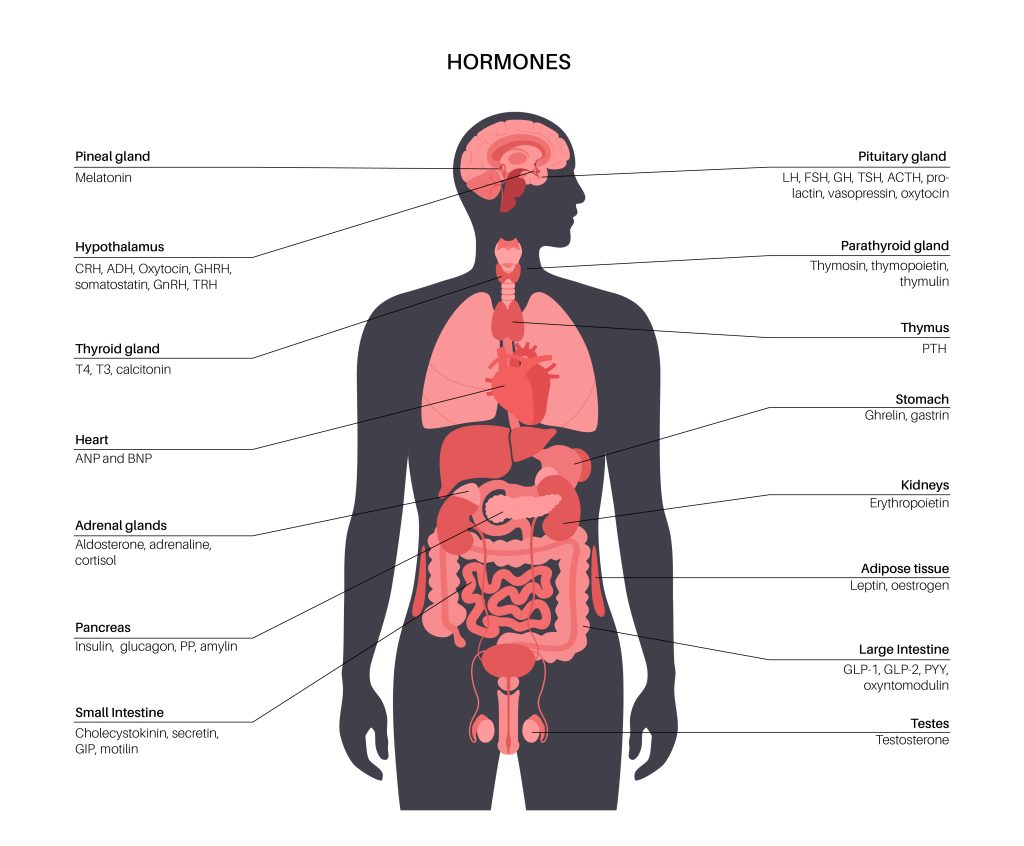
Testosterone, the primary male sex hormone, plays a pivotal role in muscle mass, fat distribution, bone density, and the overall health of men. Low levels of testosterone, a condition often seen in conjunction with obesity and type 2 diabetes, are associated with a myriad of health issues including decreased libido, fatigue, depression, and increased risk of cardiovascular diseases. The quest to elevate testosterone levels naturally has led researchers and patients alike to explore the potential benefits of weight loss medications like semaglutide in achieving this goal.
The significance of understanding the relationship between semaglutide and testosterone cannot be overstated. For men facing the dual challenges of managing their weight and maintaining healthy testosterone levels, semaglutide offers a glimmer of hope. It symbolizes not just a medical solution to their metabolic disorders but also a path to restoring hormonal balance and enhancing their quality of life. As we delve deeper into this topic, this article aims to shed light on the top questions asked by those eager to understand the potential of semaglutide in impacting testosterone levels. From its mechanism of action, side effects, and long-term safety to its comparative effectiveness and potential in combination therapies, we explore the myriad facets of semaglutide. With a focus on evidence-based insights and expert opinions, we endeavor to provide a comprehensive overview that empowers individuals with the knowledge to navigate their treatment options confidently.
2. What is Semaglutide?
Semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity, marking a pivotal shift in how these conditions are managed. As a GLP-1 receptor agonist, semaglutide mimics the action of the incretin hormone GLP-1, which is naturally secreted in response to food intake. This hormone plays a crucial role in regulating blood sugar levels by enhancing insulin secretion, inhibiting glucagon release, and delaying gastric emptying. The introduction of semaglutide into the pharmacological arsenal has provided patients and healthcare providers with a powerful tool to combat the escalating global epidemic of diabetes and obesity.
Developed through sophisticated biotechnological processes, semaglutide is structurally similar to human GLP-1 but with modifications that extend its half-life, allowing for less frequent dosing while maintaining its efficacy. This unique attribute distinguishes it from earlier GLP-1 receptor agonists and enhances patient adherence to treatment regimens. Available in both injectable and oral forms, semaglutide offers flexibility and convenience to meet the diverse needs and preferences of patients. The injectable form, marketed under the name Ozempic, is administered once weekly, whereas the oral form, known as Rybelsus, is taken daily.
The clinical trials leading to the approval of semaglutide have consistently demonstrated its effectiveness in lowering blood glucose levels and promoting significant weight loss. These outcomes are particularly beneficial for patients with type 2 diabetes, who often struggle with managing their weight—a key factor in the progression and control of their condition. The weight loss effect of semaglutide is attributed to its action on the brain’s appetite centers, reducing hunger and caloric intake. This dual action addresses two of the most challenging aspects of managing diabetes and obesity, offering a holistic approach to treatment.
Beyond its metabolic benefits, semaglutide’s impact on cardiovascular health has also been a focal point of research. Studies have shown a reduction in major cardiovascular events among patients with type 2 diabetes, positioning semaglutide as a medication that transcends glucose control, offering a multifaceted approach to improving patient outcomes.
However, the journey of semaglutide from development to widespread clinical use has not been without challenges. Its cost, potential side effects, and the need for ongoing monitoring have prompted discussions among healthcare providers and patients. Despite these challenges, the consensus remains that semaglutide’s benefits in managing type 2 diabetes and obesity—conditions at the forefront of global health concerns—far outweigh its limitations. As research continues to unravel the full potential of semaglutide, its role in the treatment of metabolic disorders is undeniably transformative. It not only offers hope to millions of patients seeking to manage their condition more effectively but also opens new avenues for exploring how this medication can impact other aspects of health, including testosterone levels and hormonal balance. The story of semaglutide is a testament to the power of innovation in addressing some of the most pressing health challenges of our time.
3. How Does Semaglutide Affect Weight Loss?
Semaglutide’s role in weight loss represents a paradigm shift in the management of obesity, a condition that has reached epidemic proportions globally. As obesity is linked with a multitude of health issues, including type 2 diabetes, cardiovascular diseases, and hormonal imbalances, the search for effective weight loss solutions has been relentless. Semaglutide, primarily known for its use in type 2 diabetes management, has emerged as a potent weapon in this battle, offering not just hope but tangible results to those struggling with obesity.
The weight loss mechanism of semaglutide is intricately linked to its action on the GLP-1 receptors in the brain, which are pivotal in regulating appetite and food intake. By mimicking the action of the naturally occurring incretin hormones, semaglutide enhances the feeling of satiety and fullness, leading to a reduction in calorie intake. This effect on appetite control is a cornerstone of semaglutide’s ability to induce weight loss. Patients report a natural decrease in hunger, which facilitates adherence to lower-calorie diets without the constant battle against cravings that often derails weight loss efforts.
Clinical trials have underscored the effectiveness of semaglutide in achieving significant weight loss. In studies comparing semaglutide with placebo and other weight loss medications, semaglutide consistently demonstrated superior efficacy in reducing body weight. Participants receiving semaglutide experienced an average weight loss of 10-15% of their body weight, a figure that marks a substantial improvement over existing medications and approaches to obesity treatment. This level of weight reduction is not only clinically significant but also translates into tangible improvements in health outcomes, including glycemic control, cardiovascular risk factors, and overall quality of life.
The impact of semaglutide on weight loss extends beyond the numbers on a scale. By aiding in weight reduction, semaglutide addresses the root causes of obesity-related comorbidities, offering a holistic approach to improving health. The reduction in body weight has been associated with improvements in insulin sensitivity, blood pressure, lipid profiles, and inflammatory markers, highlighting the broad spectrum of benefits conferred by weight loss.
Moreover, the success of semaglutide in weight management has led to its approval for use specifically in the treatment of obesity, underlining its role as a cornerstone therapy. However, the journey towards managing obesity with semaglutide is accompanied by the necessity for lifestyle modifications. Diet and exercise remain integral components of a comprehensive weight loss strategy, with semaglutide serving as a powerful adjunct to enhance outcomes.
Semaglutide offers a promising avenue for individuals seeking to overcome obesity. Its ability to induce weight loss through appetite suppression and calorie intake reduction, combined with its favorable impact on various health parameters, positions it as a transformative option in the obesity treatment landscape. As we continue to explore and understand the full potential of semaglutide, its role in reshaping the approach to weight loss and metabolic health becomes increasingly evident.

4. Can Semaglutide Influence Testosterone Levels?
The exploration of semaglutide’s influence on testosterone levels is at the frontier of endocrinological research, delving into the intricate relationship between metabolic health and hormonal balance. Testosterone, a hormone pivotal to male health, affecting muscle mass, bone density, libido, and overall well-being, has been shown to decrease in men with obesity and type 2 diabetes. This intersection of metabolic disorders and hormonal imbalances has spurred interest in the potential of semaglutide not only as a treatment for diabetes and obesity but also as a means to positively impact testosterone levels.
Emerging evidence suggests that the weight loss achieved through semaglutide therapy may play a crucial role in modulating testosterone levels. Obesity is a known risk factor for reduced testosterone in men, primarily due to the increased conversion of testosterone to estrogen in adipose tissue and the insulin resistance associated with obesity, which can impair hormonal regulation. By facilitating significant weight loss, semaglutide indirectly contributes to the amelioration of these conditions, potentially leading to an increase in testosterone levels.
Research into the direct effects of semaglutide on testosterone is still in the nascent stages, with most data pointing towards an indirect mechanism through weight loss and improved insulin sensitivity. However, the outcomes are promising. Studies have documented increases in testosterone levels among men who have experienced substantial weight loss, with semaglutide being a contributing factor. These findings are crucial, considering the broad implications of low testosterone levels on men’s health, including risks of cardiovascular disease, diabetes, and diminished quality of life.
The potential for semaglutide to influence testosterone levels also extends to its impact on insulin sensitivity and glycemic control. Insulin resistance—a hallmark of type 2 diabetes and obesity—has been linked to reduced testosterone levels. By improving insulin sensitivity and reducing blood glucose levels, semaglutide not only addresses the metabolic components of these conditions but also creates an environment conducive to hormonal balance.
However, it’s important to approach the relationship between semaglutide and testosterone with caution. While the indirect effects through weight loss and metabolic improvement are supported by current research, direct effects on the hormonal axis require further investigation. The complexity of hormonal regulation, influenced by factors ranging from genetic predispositions to lifestyle choices, underscores the need for comprehensive studies to fully understand how semaglutide may affect testosterone levels.
Semaglutide represents a beacon of hope for men suffering from the dual burdens of metabolic disorders and low testosterone. Its role in facilitating weight loss and improving metabolic health holds the promise of not only transforming physical health but also restoring hormonal balance. As research continues to unfold, the potential of semaglutide to influence testosterone levels offers a compelling narrative in the quest for holistic treatment approaches, merging metabolic and hormonal health into a unified strategy for well-being.
5. What are the Side Effects of Semaglutide?
While semaglutide has emerged as a revolutionary treatment for obesity and type 2 diabetes, offering significant benefits in weight loss and glycemic control, it is not without its side effects. Like any medication, the potential for adverse reactions must be carefully weighed against the benefits it offers. Understanding the side effects associated with semaglutide is crucial for patients and healthcare providers to navigate its use effectively.
The most commonly reported side effects of semaglutide are gastrointestinal in nature. These include nausea, vomiting, diarrhea, abdominal pain, and constipation. Such symptoms are typically most pronounced at the beginning of treatment and tend to decrease over time as the body adjusts to the medication. The mechanism behind these gastrointestinal effects is linked to semaglutide’s action on gastric emptying, which it slows down to help reduce appetite. While these side effects are generally manageable and often temporary, they can be uncomfortable and, in some cases, lead to discontinuation of the medication.
Beyond gastrointestinal issues, semaglutide has been associated with more serious, albeit less common, side effects. These include pancreatitis, an inflammation of the pancreas that can be severe and life-threatening. Symptoms of pancreatitis may include severe abdominal pain that can radiate to the back, nausea, vomiting, and a rapid heartbeat. Given this risk, patients are advised to report any significant abdominal pain immediately to their healthcare provider.
Another concern is the potential risk of thyroid C-cell tumors. Studies in rodents have shown semaglutide and other GLP-1 receptor agonists can induce thyroid C-cell tumors. However, it’s important to note that it’s unclear if this risk directly translates to humans. As a precaution, semaglutide is not recommended for individuals with a personal or family history of medullary thyroid carcinoma or patients with Multiple Endocrine Neoplasia syndrome type 2.
Changes in vision, kidney function, and gallbladder problems, including gallstones, have also been reported in patients using semaglutide. These side effects underscore the importance of regular monitoring and communication with healthcare providers throughout the treatment process. In the context of its benefits, these side effects represent the balance that must be struck in the management of chronic conditions like obesity and type 2 diabetes. Patient education and a personalized approach to treatment are key in minimizing risks while maximizing the therapeutic potential of semaglutide. As with any medication, the decision to use semaglutide should be made on an individual basis, considering the specific health profile and needs of each patient.
6. Is Semaglutide Safe for Long-Term Use?
The long-term safety of semaglutide is a critical consideration for both patients and healthcare providers, given that obesity and type 2 diabetes are chronic conditions requiring ongoing management. Since its introduction, semaglutide has undergone rigorous clinical trials and post-marketing surveillance to monitor its safety profile over extended periods. The evidence gathered thus far provides valuable insights into the long-term use of semaglutide, though with the understanding that ongoing research is essential to fully ascertain its long-term safety.
One of the key concerns with long-term use is the potential for cardiovascular effects. Given that patients with type 2 diabetes and obesity are already at an elevated risk for cardiovascular disease, the impact of semaglutide on heart health is of paramount importance. Encouragingly, large-scale cardiovascular outcome trials (CVOTs) have demonstrated that semaglutide not only does not increase cardiovascular risk but may actually confer cardiovascular benefits. These trials, including the SUSTAIN-6 trial, have shown a reduction in major adverse cardiovascular events (MACE) among participants treated with semaglutide, suggesting a protective effect on heart health.
Another area of focus has been the potential for an increased risk of certain types of cancers, particularly medullary thyroid carcinoma (MTC). As mentioned, studies in rodents have indicated a potential risk; however, long-term data in humans have yet to show a significant increase in thyroid cancer risk associated with semaglutide use. Nonetheless, vigilance and ongoing research are essential, and semaglutide is contraindicated in individuals with a personal or family history of MTC or those with Multiple Endocrine Neoplasia syndrome type 2.
The risk of pancreatitis and gallbladder disease, both of which have been associated with GLP-1 receptor agonists, including semaglutide, continues to be monitored. While these conditions are relatively rare, they are serious and require immediate medical attention if symptoms develop. Patients are advised to be aware of the symptoms of pancreatitis and gallbladder problems and to seek medical care promptly if they suspect these conditions.
Finally, the impact of semaglutide on renal function is an area of ongoing study. While semaglutide has been associated with improvements in markers of kidney function in some patients, there have been reports of acute kidney injury, usually related to dehydration from gastrointestinal side effects. As such, adequate hydration and monitoring of kidney function are recommended for patients on semaglutide.
The current body of evidence supports the safety of semaglutide for long-term use in the management of type 2 diabetes and obesity, with several potential health benefits beyond weight loss and glycemic control. However, as with all medications, the balance of risks and benefits must be carefully considered, and patients on semaglutide should be monitored regularly for any adverse effects. Continued research and post-marketing surveillance are crucial to further define the long-term safety profile of semaglutide and to ensure that its use remains in the best interest of patients managing chronic metabolic conditions.
7. How is Semaglutide Administered?
Semaglutide represents a significant advancement in the pharmacological treatment of type 2 diabetes and obesity, not only due to its efficacy but also because of its versatile administration routes. Available in both injectable and oral formulations, semaglutide offers patients and healthcare providers flexibility in tailoring treatment to individual needs and preferences, an important factor in long-term adherence and management of these chronic conditions.
The injectable form of semaglutide, marketed under the brand name Ozempic, is administered once weekly via subcutaneous injection. This once-weekly dosing schedule is seen as a considerable advantage over daily injection therapies, improving convenience and reducing the burden of treatment for patients. The injection can be self-administered after proper training from healthcare professionals, offering patients a sense of autonomy in managing their condition. Ozempic is available in pre-filled pens with different dose strengths, allowing for dose adjustments based on the patient’s response and tolerability.
In addition to the injectable form, semaglutide is available as an oral tablet, known as Rybelsus, marking a breakthrough in GLP-1 receptor agonist therapy. The development of an oral formulation of semaglutide was a significant scientific achievement, overcoming the challenges associated with the oral delivery of peptide-based medications, which are typically degraded in the stomach before they can be absorbed. Rybelsus is taken once daily on an empty stomach with a glass of water, at least 30 minutes before the first meal of the day. This unique administration route is particularly appealing to patients who are averse to injections or those looking for the simplest integration into their daily routine.
The choice between injectable and oral semaglutide depends on several factors, including patient preference, lifestyle, medical history, and specific treatment goals. While both forms have been shown to be effective in lowering blood glucose levels and aiding in weight loss, individual responses can vary. Healthcare providers play a crucial role in discussing the pros and cons of each formulation with their patients, considering factors such as ease of use, adherence potential, and side effect profiles.
Regardless of the administration route, the initiation and titration of semaglutide should be carefully managed to minimize side effects and optimize therapeutic outcomes. Starting with a lower dose and gradually increasing it allows the body to adjust to the medication, reducing the risk of gastrointestinal side effects, which are the most common adverse reactions. The availability of semaglutide in both injectable and oral forms provides valuable options for the treatment of type 2 diabetes and obesity. This flexibility in administration routes can enhance patient adherence, a critical component of effective long-term management. As with any medication, ongoing communication between patients and healthcare providers is essential to tailor the treatment plan to the individual’s needs, monitor efficacy, and adjust dosing as necessary.
8. Can Women Use Semaglutide?
The use of semaglutide in women, particularly for the treatment of type 2 diabetes and obesity, is an area of significant interest and importance. Given the global prevalence of these conditions and their impact on women’s health, understanding the gender-specific considerations, efficacy, and safety of semaglutide is crucial. Women face unique health challenges and considerations, including hormonal fluctuations, pregnancy, and breastfeeding, which can influence the management of chronic conditions and the choice of therapeutic interventions.
Clinical trials and post-marketing studies have included women and have analyzed the efficacy and safety of semaglutide across genders. These studies have consistently demonstrated that semaglutide is effective in lowering blood glucose levels and promoting weight loss in women, with a safety profile similar to that observed in men. The common side effects, including gastrointestinal issues such as nausea, vomiting, and diarrhea, are also similar across genders.
However, when considering semaglutide for women, reproductive health is a paramount consideration. Women of childbearing age who are planning to conceive or are pregnant require careful management, as the effects of semaglutide on fertility, pregnancy, and fetal development are not fully understood. Current guidelines recommend discontinuing semaglutide at least two months before attempting to conceive and avoiding its use during pregnancy and breastfeeding. This recommendation is based on the principle of caution, given the limited data on semaglutide in these populations.
Moreover, women with polycystic ovary syndrome (PCOS), a common endocrine disorder affecting women of reproductive age and often associated with obesity and insulin resistance, may be particularly interested in the potential benefits of semaglutide. While the primary use of semaglutide is for the treatment of type 2 diabetes and obesity, its impact on weight loss and metabolic health may offer indirect benefits for women with PCOS, such as the improvement of insulin sensitivity and potential amelioration of PCOS symptoms. However, specific studies targeting women with PCOS and the use of semaglutide are needed to fully understand its efficacy and safety in this population.
Semaglutide can be used by women for the treatment of type 2 diabetes and obesity, offering significant health benefits. However, considerations around pregnancy, breastfeeding, and reproductive health must be carefully navigated. Women considering semaglutide should engage in thorough discussions with their healthcare providers to weigh the benefits and risks, considering their specific health status, treatment goals, and reproductive plans. As with all patients, individualized treatment decisions, careful monitoring, and ongoing communication with healthcare professionals are key to optimizing outcomes and ensuring safety.
9. How Does Semaglutide Compare to Other Diabetes Medications?
The treatment landscape for type 2 diabetes is diverse, with a wide array of pharmacological options available to manage the condition. Semaglutide, a GLP-1 receptor agonist, stands out among these treatments due to its unique mechanism of action, efficacy, and benefits beyond glycemic control. Understanding how semaglutide compares to other diabetes medications is essential for healthcare providers and patients to make informed decisions about their treatment strategy.
Efficacy in Lowering Blood Glucose: Semaglutide has demonstrated superior efficacy in lowering HbA1c levels compared to many other classes of diabetes medications, including sulfonylureas, thiazolidinediones, and DPP-4 inhibitors. Its potent glucose-lowering effect is attributed to its action on the GLP-1 receptor, which enhances insulin secretion, suppresses glucagon release, and slows gastric emptying. This multifaceted approach not only improves glycemic control but also supports weight loss, an important consideration for many patients with type 2 diabetes.
Weight Loss Benefits: One of the most distinguishing features of semaglutide is its ability to promote significant weight loss, a benefit not commonly associated with other diabetes medications. While most other antidiabetic drugs are weight-neutral or may even cause weight gain, semaglutide’s effect on weight reduction is a valuable adjunct for patients struggling with obesity. This attribute can lead to improvements in overall metabolic health, reducing the risk of cardiovascular diseases and enhancing the quality of life.
Cardiovascular Outcomes: Recent studies have highlighted the cardiovascular benefits of semaglutide, demonstrating a reduction in major adverse cardiovascular events among patients with type 2 diabetes. This contrasts with some older diabetes medications that have been associated with neutral or potentially negative impacts on cardiovascular health. The cardiovascular protective effects of semaglutide make it an attractive option for patients with type 2 diabetes who are at an increased risk of heart disease.
Administration and Convenience: The availability of semaglutide in both injectable and oral formulations offers flexibility in administration, catering to patient preferences and lifestyles. This is a significant advantage over medications that require multiple daily doses or those only available in injectable form, potentially improving adherence and treatment outcomes.
Side Effect Profile: While semaglutide’s side effect profile is generally well-tolerated, its gastrointestinal side effects are more pronounced compared to some other diabetes medications. However, these are often transient and manageable with dose adjustments. The risk of hypoglycemia with semaglutide is lower compared to insulin and sulfonylureas, making it a safer option for many patients.
Semaglutide offers a compelling combination of efficacy, weight loss benefits, cardiovascular protection, and flexible administration options, setting it apart from other diabetes medications. Its role in the management of type 2 diabetes represents a significant advancement, providing patients with a powerful tool to control their diabetes and improve their overall health. However, individual patient characteristics, health status, and treatment goals should guide the choice of therapy, with semaglutide being one of the many options in a comprehensive diabetes care plan.
10. Can Semaglutide be Used in Combination with Other Weight Loss Medications?
The management of obesity, particularly in patients with type 2 diabetes, often requires a multifaceted approach to achieve significant and sustained weight loss. Semaglutide has emerged as a powerful monotherapy for weight management; however, the question arises whether it can be effectively combined with other weight loss medications to enhance outcomes. The potential for synergistic effects between semaglutide and other agents could offer new avenues for individuals who struggle to lose weight through diet, exercise, and monotherapy alone.
Combination Therapy Considerations: When considering the combination of semaglutide with other weight loss medications, it is crucial to evaluate the mechanisms of action, potential for additive effects, and the risk of adverse reactions. Semaglutide works primarily by mimicking GLP-1, reducing appetite, and slowing gastric emptying. Combining it with medications that act through different pathways, such as orlistat (which reduces fat absorption) or phentermine (an appetite suppressant with a different mechanism), could theoretically enhance weight loss outcomes by attacking obesity from multiple angles.
Clinical Evidence and Guidelines: To date, clinical trials specifically investigating the combination of semaglutide with other weight loss drugs are limited. However, anecdotal evidence and small-scale studies suggest that combining semaglutide with other agents can be beneficial for some patients, particularly those with significant obesity-related comorbidities. Healthcare providers must rely on clinical judgment, current guidelines, and available evidence when prescribing combination therapy, ensuring that the benefits outweigh the risks.
Safety and Monitoring: Safety is a paramount concern when considering combination therapy for weight loss. The potential for additive side effects, especially gastrointestinal issues, requires careful patient selection and monitoring. Patients on combination therapy should be closely followed to manage side effects, adjust dosages, and monitor for signs of nutrient deficiencies or other adverse effects.
Individualized Treatment Plans: Ultimately, the decision to use semaglutide in combination with other weight loss medications should be personalized, taking into account the patient’s health status, weight loss goals, and response to previous treatments. A comprehensive approach that includes dietary changes, physical activity, behavioral therapy, and pharmacotherapy, tailored to the individual’s needs, is likely to yield the best outcomes.
While semaglutide can potentially be used in combination with other weight loss medications, this approach should be navigated with caution. The absence of extensive clinical trials necessitates a cautious and evidence-based approach, with ongoing monitoring and adjustments to ensure efficacy and safety. As obesity and its related complications continue to challenge public health, exploring innovative combinations of treatments, including semaglutide, could pave the way for more effective obesity management strategies.
11. What is the Impact of Semaglutide on Cardiovascular Health?
The impact of semaglutide on cardiovascular health has become a focal point of interest for clinicians and researchers alike, given the high prevalence of cardiovascular disease (CVD) among patients with type 2 diabetes and obesity. Cardiovascular disease remains the leading cause of morbidity and mortality in these populations, underscoring the necessity for treatments that not only manage blood glucose and body weight but also confer cardiovascular benefits. Semaglutide, through extensive clinical research, has shown promising results in this regard, signaling a potential paradigm shift in the holistic management of type 2 diabetes and obesity.
Cardiovascular Outcome Trials (CVOTs): The landmark SUSTAIN-6 trial, a cardiovascular outcome trial of semaglutide, was pivotal in demonstrating the cardiovascular benefits of this medication. The trial enrolled participants with type 2 diabetes at high risk of cardiovascular events and investigated the impact of semaglutide on major adverse cardiovascular events (MACE), including heart attack, stroke, and cardiovascular death. The results were compelling, showing a significant reduction in MACE among participants treated with semaglutide compared to those receiving placebo. This outcome was particularly noteworthy as it highlighted the potential of semaglutide to go beyond glycemic control and weight management, offering protective benefits against serious cardiovascular outcomes.
Mechanisms Behind Cardiovascular Benefits: The exact mechanisms through which semaglutide exerts its cardiovascular protective effects are multifaceted and still under investigation. Possible explanations include its impact on weight loss, improvements in glycemic control, blood pressure reduction, and lipid profile improvements. Additionally, semaglutide’s anti-inflammatory and anti-atherosclerotic effects may play a role in reducing cardiovascular risk. The comprehensive nature of these effects underscores the potential of semaglutide to address multiple cardiovascular risk factors simultaneously.
Clinical Implications and Guidelines: The findings from cardiovascular outcome trials have led to a reassessment of clinical guidelines, with an increasing emphasis on selecting diabetes medications that provide cardiovascular benefits for patients at high risk of CVD. Semaglutide’s ability to reduce the risk of major cardiovascular events positions it as a preferred option for managing type 2 diabetes in patients with existing cardiovascular disease or those at high cardiovascular risk. This shift underscores a more integrated approach to treating type 2 diabetes, where the choice of medication is informed not only by its efficacy in controlling blood glucose but also by its impact on overall cardiovascular health.
Future Directions: Ongoing studies aim to further elucidate the long-term cardiovascular benefits of semaglutide and to understand the specific patient populations that may derive the most significant benefit. Additionally, research continues to explore the mechanisms behind semaglutide’s cardiovascular effects, which may lead to broader applications of GLP-1 receptor agonists in cardiovascular disease management beyond the context of diabetes and obesity.
Semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity, with notable benefits for cardiovascular health. Its ability to reduce the risk of major adverse cardiovascular events offers hope for improved outcomes in patients burdened by the high risk of cardiovascular disease, marking a step forward in the comprehensive management of these interconnected conditions.
12. Patients Taking Semaglutide and Testosterone Replacement Therapy
The intersection of metabolic health and hormonal balance, particularly in the context of semaglutide use and testosterone replacement therapy (TRT), presents a unique clinical scenario. For men experiencing obesity or type 2 diabetes alongside low testosterone levels, the combination of semaglutide and TRT could offer a dual approach to addressing these interlinked health issues. This section delves into the considerations, potential benefits, and monitoring strategies for patients embarking on this combined treatment pathway.
Clinical Considerations: The decision to initiate both semaglutide and TRT concurrently hinges on a comprehensive evaluation of the patient’s health status. Obesity and type 2 diabetes can exacerbate low testosterone levels, contributing to a cycle of metabolic dysfunction and hormonal imbalance. Semaglutide addresses the metabolic component by aiding in weight loss and improving glycemic control, potentially creating a more favorable environment for hormonal balance. TRT directly addresses the hormonal deficiency, potentially alleviating symptoms associated with low testosterone, such as fatigue, decreased libido, and loss of muscle mass. However, clinicians must navigate these treatments carefully, considering the potential for side effects and the need for tailored dosing strategies.
Potential Benefits: The synergistic use of semaglutide and TRT may offer several benefits. For individuals with obesity, the weight loss facilitated by semaglutide can improve the efficacy of TRT by reducing the conversion of testosterone to estrogen in adipose tissue and enhancing the overall hormonal profile. Improved metabolic control with semaglutide may also mitigate some of the cardiovascular risks associated with low testosterone levels. On the other hand, TRT can support the gains in muscle mass and reductions in fat mass, potentially enhancing the metabolic benefits of semaglutide.
Monitoring and Management: Close monitoring is crucial when combining semaglutide with TRT. Healthcare providers should regularly assess cardiovascular health, liver function, hematocrit levels, and prostate health, among other parameters, to ensure the safety and efficacy of the treatment. Adjustments to the dosage of either medication may be necessary based on the patient’s response, side effects, and laboratory findings. Patient education on the signs and symptoms of potential adverse effects is also essential to enable timely reporting and management.
Future Directions and Research: While the combination of semaglutide and TRT holds promise, more research is needed to fully understand the long-term benefits and risks. Clinical trials focusing on this combined approach could provide valuable insights into optimizing treatment for men with obesity or type 2 diabetes and low testosterone levels.
The concurrent use of semaglutide and testosterone replacement therapy represents a novel approach to addressing the intertwined issues of metabolic health and hormonal imbalance. With careful patient selection, monitoring, and individualized treatment plans, this combination therapy could enhance the quality of life and health outcomes for men affected by these conditions, signaling a new frontier in integrated care.
13. Conclusion
The exploration of semaglutide and its multifaceted impact on health, particularly in the realms of diabetes management, weight loss, cardiovascular health, and its potential interplay with testosterone levels, highlights a significant advancement in the treatment of chronic metabolic conditions. Semaglutide has emerged not just as a medication but as a beacon of hope for those struggling with obesity, type 2 diabetes, and the associated complications that often accompany these conditions, including compromised cardiovascular health and hormonal imbalances.
The efficacy of semaglutide in reducing blood glucose levels and promoting substantial weight loss is well-documented, offering patients a powerful tool to combat two of the most prevalent health issues of our time. Its impact extends beyond mere numbers on a scale or glycemic readings, translating into real-world benefits such as improved cardiovascular outcomes and a potential normalization of testosterone levels in men affected by obesity-induced hypogonadism. These effects underscore semaglutide’s role in addressing not only the symptoms of metabolic disorders but also their underlying causes, fostering a holistic approach to patient care.
However, the journey with semaglutide is not without its challenges. The consideration of its side effects, the importance of careful patient selection, and the ongoing monitoring required to ensure safety and efficacy highlight the complexities of managing chronic diseases. The potential for semaglutide to be used in combination with other medications, including testosterone replacement therapy, opens new avenues for personalized treatment strategies but also calls for a cautious and informed approach.
As we look to the future, the importance of continued research cannot be overstated. While the current body of evidence provides a strong foundation for the use of semaglutide in clinical practice, ongoing studies are essential to fully understand its long-term effects, optimize dosing strategies, and explore its full potential in managing not just diabetes and obesity but also their associated health conditions. The role of healthcare providers in navigating this evolving landscape, armed with the latest evidence and a commitment to patient-centered care, is crucial in maximizing the benefits of semaglutide for those in need.
In conclusion, semaglutide represents a significant leap forward in the management of diabetes and obesity, offering hope for improved health outcomes and quality of life for millions of individuals around the globe. Its development and application reflect the progress in our understanding of these complex diseases and our ability to combat them effectively, marking a milestone in the journey towards a healthier future for all.
14. Research Citations
The development and application of semaglutide as a therapeutic agent for type 2 diabetes, obesity, and potentially for the improvement of cardiovascular health and hormonal balance, is grounded in a robust body of research. The following citations provide a glimpse into the extensive scientific work that supports the use of semaglutide, offering insights into its efficacy, safety, and the potential for broader health impacts:
- Efficacy of Semaglutide in Type 2 Diabetes and Obesity: A landmark study published in the New England Journal of Medicine (Marso et al., 2016) demonstrated the efficacy of semaglutide in reducing HbA1c levels and body weight in patients with type 2 diabetes, setting the stage for its widespread use.
- Cardiovascular Outcomes with Semaglutide: The SUSTAIN-6 trial (Marso et al., 2016, New England Journal of Medicine) revealed that semaglutide significantly reduced the risk of major adverse cardiovascular events, highlighting its benefits beyond glucose control.
- Impact on Weight Loss: A pivotal trial published in The Lancet (Wilding et al., 2021) showed that semaglutide led to substantial weight loss in individuals with obesity, confirming its efficacy as a weight management solution.
- Comparison with Other Diabetes Medications: A comprehensive review in Diabetes, Obesity and Metabolism (Nauck et al., 2017) compared the efficacy and safety of semaglutide against other GLP-1 receptor agonists and diabetes medications, providing a framework for its clinical use.
- Semaglutide and Testosterone Levels: Research exploring the indirect effects of weight loss induced by semaglutide on testosterone levels in men is ongoing, with preliminary findings suggesting a positive correlation between weight reduction and hormonal balance.
- Long-Term Safety Profile: The ongoing post-marketing surveillance and studies aim to further elucidate the long-term safety profile of semaglutide, ensuring that its benefits continue to outweigh any potential risks.
These citations represent just a fraction of the extensive research that underpins the use of semaglutide in clinical practice. They serve as a foundation for healthcare providers to make informed decisions and for patients to understand the potential benefits and risks associated with its use. As the scientific community continues to investigate semaglutide, it is expected that additional findings will further refine its role in managing diabetes, obesity, and related health concerns, ensuring that treatment approaches remain evidence-based and patient-centered.
Questions and Answers: Semaglutide and Testosterone
Semaglutide promotes weight loss primarily through its action on GLP-1 receptors, which are involved in regulating appetite and food intake. By mimicking the action of GLP-1, it reduces appetite, leading to a decrease in caloric intake and subsequent weight loss. Clinical trials have shown that patients can expect significant weight reduction, with an average loss of 10-15% of body weight over 68 weeks when used in conjunction with lifestyle modifications. The degree of weight loss varies among individuals, depending on factors such as baseline weight, adherence to a healthy diet, and physical activity levels.
Semaglutide has been rigorously evaluated in clinical trials for its safety and efficacy. While it is generally well-tolerated, long-term surveillance continues to monitor for potential risks. Concerns such as the risk of thyroid C-cell tumors in rodents, pancreatitis, and retinopathy have been noted, but the overall benefit-risk profile remains favorable. Ongoing research and post-marketing surveillance are crucial to fully understand the long-term safety of semaglutide.
Yes, semaglutide has demonstrated significant cardiovascular benefits in major clinical trials. It has been shown to reduce the risk of major adverse cardiovascular events, such as heart attack, stroke, and cardiovascular death, in patients with type 2 diabetes. These effects are attributed to its impact on weight loss, improved glycemic control, and possibly direct beneficial effects on the cardiovascular system.
For patients with pre-existing cardiovascular conditions, semaglutide offers dual benefits by managing blood glucose levels and providing cardiovascular protection. It is particularly beneficial for patients at high risk of cardiovascular events, as it can lead to a significant reduction in such events. However, individual assessment and monitoring are essential to ensure its appropriateness for each patient’s specific condition.
While semaglutide is not directly used to treat hormonal imbalances, its effectiveness in promoting weight loss may indirectly improve testosterone levels in men with obesity-related low testosterone. Weight loss has been associated with an increase in testosterone levels, potentially alleviating symptoms of low testosterone. However, further research is needed to fully understand the impact of semaglutide on hormonal balance.
Combining semaglutide with other medications, including testosterone replacement therapy, requires a personalized approach, considering the patient’s overall health status, goals, and potential interactions. Close monitoring for efficacy and adverse effects is crucial, with adjustments made as necessary to optimize patient outcomes. Collaboration among specialists, such as endocrinologists and cardiologists, may enhance the management of complex cases.
Semaglutide is primarily approved for use in type 2 diabetes due to its mechanism of action, which relies on the presence of endogenous insulin production. In patients with type 1 diabetes, where there is an absolute deficiency of insulin, the primary treatment remains insulin therapy. While semaglutide may offer potential benefits such as weight loss, its use in type 1 diabetes is not widely recommended and should only be considered under specific circumstances and close medical supervision. Ongoing research is evaluating its safety and efficacy in this population, but insulin therapy remains the cornerstone of type 1 diabetes management.
Semaglutide has a relatively low potential for direct drug-drug interactions because it does not directly interfere with the cytochrome P450 system, which is responsible for the metabolism of many drugs. However, due to its effects on gastric emptying, semaglutide can affect the absorption of orally administered medications. Patients are advised to take oral medications at least 30 minutes before taking semaglutide to minimize this interaction. Specific concerns or potential interactions should be discussed with a healthcare provider, as individual factors may influence the risk of interactions.
Semaglutide, like other GLP-1 receptor agonists, has a low inherent risk of causing hypoglycemia when used alone because its glucose-lowering effect is glucose-dependent; it stimulates insulin secretion only when blood glucose levels are elevated. However, when semaglutide is used in combination with other antidiabetic agents that can cause hypoglycemia, such as sulfonylureas or insulin, the risk of hypoglycemia may increase. Patients on combination therapy should be closely monitored, and adjustments to the dosing of these medications may be necessary to minimize the risk of hypoglycemia.
The guidelines for stopping semaglutide before surgery or medical procedures primarily concern its effects on gastric emptying and potential interactions with perioperative medications or anesthesia. Generally, it is recommended to temporarily discontinue semaglutide at least 72 hours before planned surgery or any procedure requiring anesthesia. This precaution is to ensure that the effects of semaglutide on gastric emptying do not interfere with the management of perioperative nutrition or medication absorption. The decision to stop semaglutide should be made in consultation with the healthcare provider overseeing the patient’s diabetes management and the surgical or procedural team to ensure a coordinated approach to care.

Dr. Kevin Kargman
Dr. Kevin J. Kargman is a pediatrician in Sewell, New Jersey and is affiliated with multiple hospitals in the area, including Cooper University Health Care-Camden and Jefferson Health-Stratford, Cherry Hill and Washington Township. (Learn More)
