Table of Contents
1. Introduction
In the evolving landscape of medical treatments for chronic conditions such as type 2 diabetes and obesity, semaglutide has emerged as a beacon of hope for many. Developed through cutting-edge research, this medication belongs to a class of drugs known as GLP-1 receptor agonists, which have revolutionized the approach to managing these prevalent health issues. Semaglutide’s ability to effectively control blood sugar levels and promote significant weight loss has made it a preferred choice for patients and healthcare providers alike. However, amidst its growing popularity and widespread use, concerns regarding its impact on the gallbladder have surfaced, leading to a surge in inquiries and debates within the medical community and among those it aims to benefit.
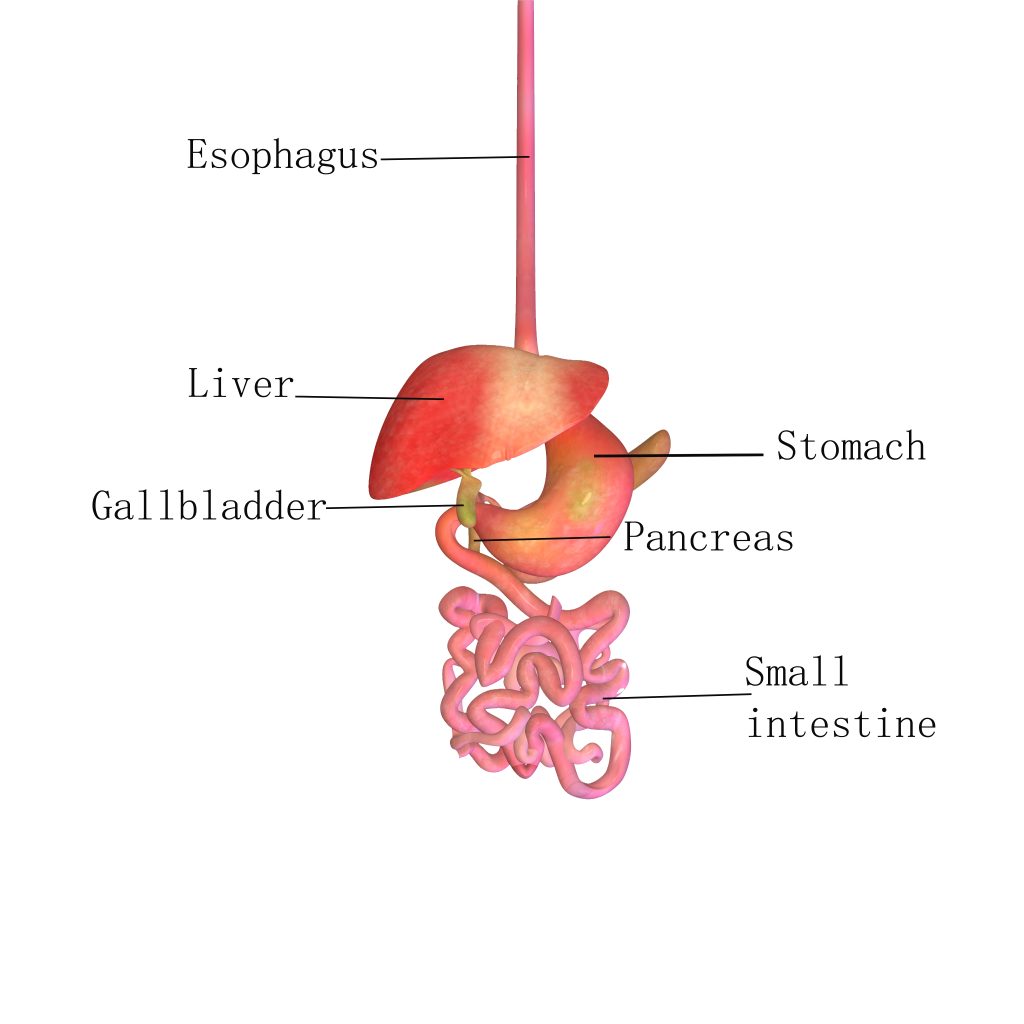
The gallbladder, a small organ tucked beneath the liver, plays a crucial role in digestion by storing and concentrating bile, a digestive fluid produced by the liver. This organ may seem inconsequential to the uninitiated, but its health is vital for the proper digestion of fats and the overall functioning of the digestive system. Issues with the gallbladder, such as gallstones or inflammation (cholecystitis), can lead to severe abdominal pain, nausea, and even more serious complications requiring medical intervention. Given the gallbladder’s role and the potential side effects associated with semaglutide, understanding the interplay between this medication and gallbladder health is of paramount importance.
The relationship between semaglutide and the gallbladder is complex and multifaceted. As semaglutide alters the way the body responds to food intake, it may inadvertently affect gallbladder function. Questions arise about whether semaglutide can lead to an increased risk of gallbladder issues, such as the formation of gallstones or the exacerbation of existing gallbladder conditions. These concerns are not unfounded, as the medication’s mechanism—slowing gastric emptying and altering hormone levels—could theoretically impact bile flow and composition, potentially leading to gallbladder complications.
This article aims to shed light on the intricate connection between semaglutide and gallbladder health. By addressing the most common inquiries, presenting current research, and exploring patient experiences, we seek to provide a comprehensive understanding of what individuals considering or currently using semaglutide need to know about its effects on the gallbladder. As we navigate through the subsequent sections, we will delve into the science behind semaglutide, the nature of gallbladder disease, symptoms to watch for, diagnostic approaches, management strategies, and the importance of preventive measures. Through this exploration, our goal is to equip readers with the knowledge they need to make informed decisions about their health and treatment options, balancing the undeniable benefits of semaglutide with a mindful consideration of its potential risks.
2. Understanding Semaglutide
Semaglutide stands at the forefront of modern pharmacotherapy for type 2 diabetes and obesity, marking a significant advancement in the treatment of these conditions. As a GLP-1 (Glucagon-Like Peptide-1) receptor agonist, it mimics the action of the naturally occurring hormone GLP-1, which plays a pivotal role in glucose metabolism and appetite regulation. This medication not only aids in lowering blood sugar levels but also contributes to weight loss, making it a dual-purpose tool in the management of diabetes and obesity. The journey of semaglutide from its development to its current status as a cornerstone in the treatment of these diseases underscores its importance in the medical field.
The mechanism of action of semaglutide is both fascinating and complex. By binding to the GLP-1 receptors in the pancreas, it enhances the release of insulin in response to elevated blood glucose levels. This insulin release is glucose-dependent, which means it occurs only when there are high levels of glucose in the blood, thereby reducing the risk of hypoglycemia—a common concern with other diabetes medications. Furthermore, semaglutide slows gastric emptying, the process by which food moves from the stomach to the small intestine. This slowing effect contributes to prolonged feelings of fullness, reduced appetite, and ultimately, weight loss. Additionally, semaglutide has been shown to decrease glucagon secretion, a hormone that raises blood glucose levels, further contributing to its glucose-lowering effects.
Semaglutide is available in two forms: a once-weekly injectable solution and an oral tablet, offering flexibility and convenience to meet the varied preferences and needs of patients. The injectable form, introduced first, has been a game-changer for patients who struggle with daily medication regimens, offering a less frequent dosing schedule that improves adherence and quality of life. The oral form, a more recent development, represents a breakthrough in peptide-based therapy, making GLP-1 treatment accessible to those who are needle-averse.
The efficacy of semaglutide in controlling blood sugar levels and promoting weight loss is well-documented in numerous clinical trials. These studies have consistently shown significant reductions in HbA1c (a marker of long-term blood glucose control) and body weight, leading to its approval and widespread use. Patients using semaglutide have reported not only improvements in their physical health but also enhancements in their overall well-being and quality of life. Despite its benefits, the journey of semaglutide is accompanied by ongoing research and dialogue about its safety profile, particularly concerning the gallbladder. As we continue to embrace semaglutide for its therapeutic benefits, understanding its full spectrum of effects, including potential impacts on the gallbladder, remains a critical area of focus for researchers, healthcare providers, and patients alike.
3. Semaglutide and the Gallbladder: An Overview
The relationship between semaglutide and the gallbladder is an area of growing interest and concern within the medical community. Semaglutide, as a GLP-1 receptor agonist, has a multifaceted mechanism of action that not only influences glucose metabolism and appetite but also may impact the function of the gallbladder. Understanding this relationship is crucial, as it can lead to a better management of potential side effects and enhance the overall treatment experience for patients using semaglutide for diabetes and obesity management.
The gallbladder’s primary function is to store and concentrate bile, a digestive fluid produced by the liver that helps in the digestion of fats. After a meal, the gallbladder contracts and releases bile into the small intestine to aid in the breakdown and absorption of dietary fats. GLP-1 receptor agonists like semaglutide can influence this process indirectly through their effects on gastric emptying and possibly bile secretion. By slowing down the rate at which the stomach empties its contents into the small intestine, semaglutide may also affect the timing and flow of bile from the gallbladder.
There is a theoretical concern that prolonged use of semaglutide could lead to an increased risk of gallbladder disorders, including gallstones (cholelithiasis), inflammation (cholecystitis), and biliary sludge. Gallstones form when there is an imbalance in the composition of bile, leading to the crystallization of substances like cholesterol or bilirubin. Since semaglutide alters digestive processes, it could potentially contribute to changes in bile composition or stasis, which are risk factors for gallstone formation.
Clinical trials and observational studies have begun to shed light on the incidence of gallbladder-related issues in patients using semaglutide. Some studies have reported a slight increase in gallbladder conditions among semaglutide users compared to those not on the medication or those on other diabetes medications. These findings have prompted further investigation into the exact nature of semaglutide’s impact on the gallbladder and the mechanisms behind it.
However, it’s important to contextualize these risks within the broader spectrum of semaglutide’s benefits. The potential for improved glycemic control, significant weight loss, and reduced risk of cardiovascular events for many patients outweighs the relatively low incidence of gallbladder complications. Nevertheless, healthcare providers should consider these factors when prescribing semaglutide, especially for patients with a history of gallbladder disease or other risk factors for gallstone formation. While semaglutide offers significant benefits in the management of type 2 diabetes and obesity, its effects on the gallbladder warrant careful consideration and monitoring. Ongoing research and clinical vigilance are essential to fully understand and manage these potential side effects, ensuring that patients can safely and effectively use semaglutide to improve their health outcomes.

4. The Risk of Gallbladder Disease with Semaglutide
The burgeoning interest in the effects of semaglutide on gallbladder health stems from its widespread use and the emerging data suggesting a potential association between GLP-1 receptor agonists and gallbladder disease. Gallbladder disease encompasses a range of conditions, including gallstones, cholecystitis, and biliary sludge, each presenting its own set of challenges and complications. Understanding the risk of gallbladder disease associated with semaglutide is imperative for clinicians and patients alike to navigate treatment decisions effectively.
Gallstones are the most common form of gallbladder disease, consisting of hard particles that form from cholesterol or bilirubin in the bile. These stones can block the flow of bile out of the gallbladder, causing pain, infection, and inflammation. The pathophysiology behind gallstone formation involves factors like supersaturation of cholesterol in bile, bile stasis, and changes in the bile acid composition, which can be influenced by diet, obesity, and, potentially, medications like semaglutide.
Clinical evidence has pointed to an increased incidence of gallbladder-related events in patients using semaglutide. For instance, in a pooled analysis of clinical trials, patients treated with semaglutide showed a slightly higher rate of gallbladder disorders compared to those on placebo or other diabetes medications. These findings have led to discussions about the need for monitoring and managing the risk of gallbladder disease in patients prescribed semaglutide.
Risk factors for developing gallbladder disease while on semaglutide include a history of gallstones, rapid weight loss, and obesity. Rapid weight loss, which can occur with the use of semaglutide, especially at higher doses for obesity treatment, has long been recognized as a risk factor for gallstone formation. The rapid mobilization of cholesterol from adipose tissue during weight loss may lead to an increased concentration of cholesterol in bile, contributing to gallstone formation.
It is essential for healthcare providers to assess individual risk factors for gallbladder disease when prescribing semaglutide and to educate patients on the potential signs and symptoms of gallbladder complications. Symptoms such as abdominal pain, particularly in the right upper quadrant, nausea, vomiting, and fever should prompt immediate medical evaluation for gallbladder disease. While semaglutide presents a valuable option for the management of type 2 diabetes and obesity, the potential risk of gallbladder disease requires attention and appropriate management. Patients should be counseled on the importance of reporting any new or worsening symptoms promptly, and healthcare providers should remain vigilant in monitoring for signs of gallbladder complications. Through careful patient selection, risk assessment, and ongoing monitoring, the benefits of semaglutide can be maximized while minimizing the risks to gallbladder health.
5. Symptoms and Signs of Gallbladder Issues in Semaglutide Users
Identifying the symptoms and signs of gallbladder issues is crucial for individuals taking semaglutide, as early detection can significantly impact the management and outcome of these conditions. Gallbladder problems, while potentially serious, often present with recognizable symptoms that should prompt individuals to seek medical evaluation. The most common gallbladder-related complications that may arise in the context of semaglutide use include gallstones, cholecystitis (inflammation of the gallbladder), and biliary sludge, each with its own set of manifestations.
Gallstones, one of the primary gallbladder issues associated with semaglutide, can cause a condition known as biliary colic. This condition is characterized by sudden, severe pain in the upper right abdomen or the center of the abdomen, just below the breastbone. The pain may also radiate to the right shoulder or back and can vary in intensity, often described as a deep, sharp, or cramping pain. Biliary colic typically occurs after eating, especially fatty meals, as the gallbladder contracts in an attempt to release bile but is obstructed by gallstones.
Cholecystitis, or inflammation of the gallbladder, presents with symptoms similar to those of biliary colic but may be accompanied by fever, chills, and a more prolonged duration of pain. The abdominal pain associated with cholecystitis is usually severe and constant, and it may be accompanied by tenderness when touching the abdomen. Nausea and vomiting are also common symptoms, reflecting the body’s response to the inflammation.
Biliary sludge, a mixture of particulate matter and bile, can lead to symptoms similar to those of gallstones, though often less severe. It can be a precursor to gallstone formation and may cause pain, nausea, and other digestive disturbances.
In addition to these specific symptoms, individuals may experience jaundice (yellowing of the skin and eyes), a result of bile duct obstruction, which prevents bile from being excreted into the intestine and leads to a buildup of bilirubin in the blood. Dark urine, pale stools, and itching can also indicate gallbladder issues, reflecting changes in bile composition or flow.
For semaglutide users, being vigilant about these symptoms is essential. The medication’s effects on gastric emptying and potential impact on bile composition necessitate awareness of the signs of gallbladder disease. Individuals experiencing any of these symptoms should consult their healthcare provider promptly for evaluation. Diagnostic tests, including ultrasound imaging of the gallbladder and liver function tests, can help determine the cause of the symptoms and guide appropriate treatment. While semaglutide offers significant benefits for individuals with type 2 diabetes and obesity, awareness of the potential signs and symptoms of gallbladder issues is critical. Early detection and treatment can mitigate the severity of these conditions, ensuring that patients can continue to benefit from semaglutide with minimal risk to their gallbladder health.
6. Diagnosing Gallbladder Problems in Patients Using Semaglutide
The diagnosis of gallbladder problems in patients using semaglutide involves a combination of clinical evaluation, symptom assessment, and diagnostic imaging. Given the potential for semaglutide to influence gallbladder function, healthcare providers must employ a thorough diagnostic approach to identify and address gallbladder issues promptly. This process is critical for ensuring patient safety and optimizing treatment outcomes.
The initial step in diagnosing gallbladder problems involves a detailed patient history and physical examination. Healthcare providers will inquire about the onset, duration, and nature of symptoms, such as abdominal pain, nausea, and changes in bowel habits. Particular attention is paid to symptoms suggestive of biliary colic or cholecystitis, including the location and character of abdominal pain, its association with meals, and any accompanying symptoms like fever or jaundice.
Following the clinical assessment, diagnostic imaging plays a pivotal role in identifying gallbladder pathology. The ultrasound is the imaging modality of choice for evaluating the gallbladder, owing to its non-invasive nature, high sensitivity, and specificity for detecting gallstones and signs of inflammation. Ultrasound can visualize gallstones, gallbladder wall thickening, and pericholecystic fluid, all indicative of gallbladder disease. In some cases, where the ultrasound findings are inconclusive or further evaluation of the biliary tree is necessary, additional imaging studies such as a hepatobiliary iminodiacetic acid (HIDA) scan or magnetic resonance cholangiopancreatography (MRCP) may be employed.
Liver function tests (LFTs) are another critical component of the diagnostic process, providing information on the liver and biliary system’s functional status. Abnormalities in LFTs, such as elevated bilirubin levels, alkaline phosphatase, or liver enzymes, can suggest biliary obstruction or liver involvement secondary to gallbladder disease.
For patients on semaglutide presenting with symptoms of gallbladder issues, healthcare providers may also consider the role of medication in their diagnostic and management strategy. While not all gallbladder problems in semaglutide users are directly related to the medication, the possibility of a drug-induced effect on gallbladder function warrants consideration, particularly in individuals with no prior history of gallbladder disease.
The management of diagnosed gallbladder problems in semaglutide users involves a multidisciplinary approach, balancing the need to address the gallbladder issue with the benefits of continuing semaglutide for diabetes or obesity management. In some cases, temporary discontinuation of semaglutide may be necessary, especially if gallbladder surgery is indicated. However, decisions regarding the continuation or cessation of semaglutide therapy should be made on a case-by-case basis, considering the individual patient’s health status and treatment goals. Diagnosing gallbladder problems in patients using semaglutide requires a comprehensive approach that integrates clinical evaluation, diagnostic imaging, and laboratory tests. By accurately identifying gallbladder issues, healthcare providers can implement appropriate management strategies to address these complications while considering the ongoing treatment of the patient’s underlying conditions.

7. Management and Treatment of Gallbladder Issues
The management and treatment of gallbladder issues in patients using semaglutide require a nuanced approach that balances the therapeutic benefits of the medication with the need to address the gallbladder condition effectively. When gallbladder problems are diagnosed, the treatment plan may vary based on the severity and type of the issue, ranging from conservative management for mild cases to surgical intervention for more severe conditions.
Conservative Management: For patients with mild symptoms of gallbladder issues, such as biliary colic without evidence of cholecystitis or choledocholithiasis (stones in the bile ducts), conservative management may be the first line of treatment. This approach includes dietary modifications to reduce gallbladder stress, such as a low-fat diet that minimizes the gallbladder’s need to contract and release bile. Hydration and pain management with non-opioid analgesics can also be part of the conservative treatment regimen. In some cases, healthcare providers may recommend a temporary pause or adjustment in the dosage of semaglutide to see if symptoms improve, especially if the medication is suspected to contribute to gallbladder issues.
Medications: Ursodeoxycholic acid, a bile acid, may be prescribed to dissolve small cholesterol gallstones. This medication works by decreasing the concentration of cholesterol in bile, which can help dissolve the stones over time. However, it is generally reserved for patients who are not candidates for surgery or in specific circumstances where surgery needs to be delayed.
Surgical Intervention: For patients with acute cholecystitis, choledocholithiasis, or symptomatic gallstones that do not respond to conservative management, cholecystectomy (surgical removal of the gallbladder) may be indicated. Cholecystectomy can be performed laparoscopically, a minimally invasive procedure that typically allows for a quicker recovery and less pain than open surgery. This surgery is highly effective in relieving symptoms and preventing future complications related to gallstones or gallbladder inflammation.
Post-Treatment Considerations: After addressing the gallbladder issue, the decision to continue semaglutide therapy should be carefully considered. For many patients, the benefits of semaglutide in managing diabetes or obesity will outweigh the potential risks associated with gallbladder problems. However, ongoing monitoring for gallbladder symptoms is essential, and lifestyle modifications should be maintained to support overall digestive health.
The management and treatment of gallbladder issues in patients using semaglutide involve a combination of conservative measures, medication, and possibly surgery, depending on the severity of the condition. Close collaboration between patients and healthcare providers is crucial to develop an individualized treatment plan that addresses the gallbladder issue while considering the patient’s broader health needs and treatment goals.
8. Preventative Measures
Preventing gallbladder issues, particularly in patients using semaglutide, involves a proactive approach centered around lifestyle modifications and regular monitoring. While it may not be possible to prevent all cases of gallbladder disease, certain measures can significantly reduce the risk and mitigate the severity of potential problems. Here are key strategies for minimizing the risk of gallbladder complications in semaglutide users:
Dietary Adjustments: Adopting a balanced diet that is low in saturated fats and refined sugars but high in fiber can help maintain healthy gallbladder function. Foods rich in healthy fats, such as omega-3 fatty acids found in fish and nuts, and plenty of fruits, vegetables, and whole grains, support digestive health and may reduce the risk of gallstone formation. Additionally, maintaining a steady, moderate weight loss pace (if weight reduction is a goal) can prevent the rapid changes in bile chemistry that contribute to gallstone formation.
Hydration: Adequate hydration is essential for maintaining the fluidity of bile and preventing the concentration of substances that can lead to gallstone formation. Patients should be encouraged to drink sufficient water throughout the day to support overall health and reduce the risk of gallstones.
Regular Physical Activity: Regular exercise helps in maintaining a healthy weight and supports overall digestive health. Moderate-intensity activities, such as walking, cycling, or swimming, can have positive effects on gallbladder function and help prevent gallstones by improving gastrointestinal motility and reducing cholesterol levels in bile.
Monitoring for Symptoms: Patients using semaglutide should be educated about the signs and symptoms of gallbladder issues and advised to report any new or worsening symptoms to their healthcare provider promptly. Early detection of gallbladder problems can lead to more effective management and treatment, potentially avoiding more serious complications.
Regular Medical Check-ups: Regular follow-ups with a healthcare provider can help monitor the effects of semaglutide on overall health, including the gallbladder. These check-ups provide an opportunity to adjust treatment plans as needed and conduct diagnostic tests if gallbladder issues are suspected.
By incorporating these preventative measures, patients using semaglutide can reduce their risk of developing gallbladder problems and maintain better overall health. Healthcare providers play a crucial role in educating patients about these strategies and supporting them in implementing lifestyle changes that promote healthy gallbladder function.
9. Patient Testimonials and Case Studies
The integration of patient testimonials and case studies offers invaluable insights into the real-world experiences of individuals using semaglutide, particularly concerning gallbladder issues. These narratives not only shed light on the challenges faced by patients but also highlight the strategies and treatments that have proven effective in managing these complications. Through a collection of diverse experiences, we gain a comprehensive understanding of the impact of semaglutide on gallbladder health and the importance of proactive management.
Case Study 1: The Case of Emily
Emily, a 45-year-old female with type 2 diabetes and obesity, began treatment with semaglutide to improve her glycemic control and support weight loss. After several months of therapy, Emily experienced significant benefits, including a noticeable reduction in her HbA1c levels and a 15-pound weight loss. However, she soon started experiencing intermittent, severe pain in the upper right quadrant of her abdomen, particularly after meals. An ultrasound confirmed the presence of gallstones, with no signs of cholecystitis.
Management: Emily’s healthcare team decided to adopt a conservative management approach initially, adjusting her diet to reduce fat intake and increasing her hydration. They also monitored her symptoms closely, opting to continue semaglutide due to its benefits. Over time, Emily’s gallbladder symptoms improved with these dietary changes, and she remained on semaglutide without requiring surgical intervention.
Case Study 2: The Case of John
John, a 52-year-old male with a history of obesity, started on semaglutide as part of a comprehensive weight management program. While John experienced significant weight loss, he developed acute abdominal pain and was diagnosed with acute cholecystitis after an evaluation that included an ultrasound and elevated liver enzymes.
Management: Given the acute nature of John’s condition, he underwent a laparoscopic cholecystectomy, which resolved his symptoms. Post-surgery, John and his healthcare provider discussed the risks and benefits of continuing semaglutide. Considering the absence of his gallbladder and the ongoing benefits of semaglutide for his diabetes and weight management, they decided to resume the medication, with regular follow-ups to monitor his health.
Patient Testimonial: The Story of Alex
Alex, a 38-year-old with type 2 diabetes, shared their journey on an online forum, detailing their experience with semaglutide and subsequent gallbladder issues. Alex emphasized the importance of being attuned to their body’s signals, noting that early recognition of gallbladder-related symptoms led to prompt medical intervention and management. Despite the setback, Alex expressed gratitude for the support received from healthcare providers and the diabetes community, highlighting the significance of a supportive network in navigating the challenges of managing chronic conditions.
These case studies and testimonials underscore the variability in patient experiences with semaglutide and gallbladder issues. They highlight the importance of individualized care, the potential need for adjustments in treatment plans, and the value of patient education and support networks. Through these narratives, healthcare providers and patients alike can better understand the complexities of managing gallbladder health in the context of semaglutide therapy, leading to improved outcomes and enhanced patient satisfaction.
10. Future Research Directions
The exploration of semaglutide’s effects on the gallbladder represents a dynamic area of clinical research, with ongoing studies aiming to elucidate the mechanisms behind these associations and to identify strategies for prevention and management. The future research directions in this field are guided by the need to address the gaps in current knowledge, improve patient care, and optimize the therapeutic benefits of semaglutide while minimizing adverse effects. Here are key areas where future research is needed:
Mechanistic Studies: Understanding the precise mechanisms by which semaglutide may influence gallbladder function and contribute to gallstone formation or gallbladder disease is crucial. Research focusing on the drug’s impact on bile composition, gallbladder motility, and gastrointestinal hormones could provide valuable insights into how to mitigate these risks.
Long-term Safety Data: Longitudinal studies tracking patients on semaglutide over extended periods are essential to gather comprehensive safety data, including the incidence of gallbladder issues. These studies will help clarify the long-term risk profile of semaglutide and inform clinical guidelines for monitoring and management.
Comparative Effectiveness Research: Studies comparing semaglutide with other GLP-1 receptor agonists and diabetes medications can help determine if the risk of gallbladder issues is unique to semaglutide or a class effect. This research would aid in personalized medication selection based on patient-specific risk factors for gallbladder disease.
Preventive Strategies: Investigating preventive measures, including dietary interventions, lifestyle modifications, and possibly adjunctive medications, could offer approaches to reduce the incidence of gallbladder issues in patients using semaglutide. Randomized controlled trials focusing on prevention could significantly impact clinical practice by providing evidence-based recommendations for patients at risk.
Patient-Centered Outcomes: Research exploring the quality of life, patient satisfaction, and treatment adherence among semaglutide users with gallbladder issues will contribute to a more patient-centered approach to care. Understanding patients’ perspectives and experiences can guide the development of supportive interventions and educational resources.
Genetic and Biomarker Studies: Identifying genetic predispositions or biomarkers associated with an increased risk of gallbladder issues in semaglutide users could lead to personalized treatment plans and targeted monitoring strategies. This precision medicine approach would optimize the benefits of semaglutide while reducing adverse outcomes.
As the use of semaglutide continues to grow, so does the importance of advancing our understanding of its effects on gallbladder health. Future research in these areas promises to enhance our knowledge, improve patient care, and refine the therapeutic use of semaglutide in the management of type 2 diabetes and obesity. Through continued investigation and collaboration among researchers, clinicians, and patients, the goal of maximizing the benefits of semaglutide while safeguarding patient health remains within reach.
11. Conclusion
The journey through understanding the relationship between semaglutide and gallbladder health has been comprehensive, traversing the mechanisms of semaglutide’s action, its benefits in managing type 2 diabetes and obesity, the potential risks it poses to the gallbladder, and the strategies for diagnosis, management, and prevention of gallbladder issues. This exploration underscores the importance of a balanced perspective when considering semaglutide therapy, recognizing both its substantial advantages and the need to be vigilant about potential side effects.
Semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity, offering patients a powerful tool to control their blood sugar levels and reduce body weight. Its mechanism, mimicking the action of the GLP-1 hormone, taps into the body’s natural regulatory systems, promoting insulin production and decreasing appetite. However, the impact of semaglutide on the gallbladder has emerged as an area of concern, with evidence suggesting a possible increase in gallbladder-related issues among users. This highlights the complexity of managing chronic conditions, where treatment benefits must be weighed against potential risks.
The management of gallbladder issues in patients using semaglutide requires a multidisciplinary approach, integrating dietary adjustments, lifestyle modifications, and, in some cases, surgical intervention. Healthcare providers play a crucial role in this process, guiding patients through informed decision-making, closely monitoring for symptoms of gallbladder disease, and adjusting treatment plans as necessary to ensure patient safety and optimize outcomes.
Preventative measures, including maintaining a healthy diet, staying hydrated, and engaging in regular physical activity, are essential strategies for minimizing the risk of gallbladder problems. Additionally, patient education on the potential signs and symptoms of gallbladder issues can facilitate early detection and treatment, enhancing the overall success of semaglutide therapy.
As we look to the future, ongoing research is critical to deepening our understanding of semaglutide’s effects on the gallbladder. Studies focusing on the mechanisms behind these effects, long-term safety data, preventive strategies, and patient-centered outcomes will continue to inform clinical practice, ensuring that patients receive the most effective and safe care possible.
In conclusion, semaglutide offers significant benefits for individuals with type 2 diabetes and obesity, but its use requires careful consideration of gallbladder health. Through vigilant monitoring, individualized treatment approaches, and a commitment to patient education, healthcare providers can navigate the challenges associated with semaglutide therapy, maximizing its benefits while minimizing risks. As research advances, the medical community’s ability to manage these challenges will improve, enhancing the quality of care for patients relying on semaglutide to manage their chronic conditions. Click to learn more about the cost of semaglutide in our program.
12. Research Citations
In the exploration of semaglutide’s impact on gallbladder health, several key studies and reviews have provided valuable insights, informing the discussions and recommendations presented throughout this article. Below is a selection of pivotal research citations that have contributed to our understanding of the relationship between semaglutide and the gallbladder:
- Clinical Trials on Semaglutide’s Efficacy and Safety: The SUSTAIN and PIONEER clinical trial series have been instrumental in demonstrating semaglutide’s benefits in glycemic control and weight reduction, while also noting the incidence of gallbladder-related adverse events. These trials offer a comprehensive overview of semaglutide’s profile, highlighting its therapeutic potential and safety considerations.
- SUSTAIN clinical trials series: References to specific trials within this series can be found in leading medical journals, providing detailed data on semaglutide’s efficacy and safety across diverse patient populations.
- PIONEER clinical trials series: Similar to the SUSTAIN series, the PIONEER trials focus on the oral formulation of semaglutide, contributing to the body of evidence supporting its use in clinical practice.
- Review Articles on GLP-1 Receptor Agonists and Gallbladder Function: Scholarly review articles that synthesize findings from multiple studies have offered insights into the mechanisms by which GLP-1 receptor agonists, including semaglutide, might influence gallbladder function and the risk of gallstones.
- Example: A comprehensive review published in the “Journal of Endocrinological Investigation” discusses the physiological effects of GLP-1 receptor agonists on the gallbladder, summarizing current knowledge and identifying areas for future research.
- Case Reports and Observational Studies: Individual case reports and larger observational studies have documented instances of gallbladder disease in patients using semaglutide, providing real-world evidence of this potential side effect and suggesting factors that may contribute to an increased risk.
- Case reports in medical journals often detail specific instances of gallbladder issues arising after the initiation of semaglutide therapy, offering insights into clinical presentations and management strategies.
- Guidelines and Recommendations: Professional organizations, such as the American Diabetes Association (ADA) and the Endocrine Society, periodically release guidelines that include considerations for the use of GLP-1 receptor agonists like semaglutide, taking into account their impact on gallbladder health among other safety and efficacy factors.
- ADA’s Standards of Medical Care in Diabetes: This document provides evidence-based recommendations for the management of diabetes, including the use of medications like semaglutide and considerations related to gallbladder health.
The research citations listed above serve as a foundation for understanding semaglutide’s role in diabetes and obesity management, its potential effects on the gallbladder, and the strategies for mitigating these risks. As the scientific community continues to investigate this topic, further studies will undoubtedly contribute to our knowledge, guiding clinical practice and patient care in the years to come.
Questions and Answers: Semaglutide and gallbladder
Semaglutide, like other GLP-1 receptor agonists, can influence gallbladder function indirectly through its effects on digestion and bile dynamics. By slowing gastric emptying, semaglutide may alter the timing and flow of bile, potentially leading to bile stasis—a condition that can contribute to the formation of gallstones. Furthermore, changes in weight, particularly rapid weight loss, can affect bile composition, increasing the risk of gallstones.
Patients using semaglutide should be vigilant for symptoms such as acute or intermittent pain in the upper right abdomen, nausea, vomiting, and fever, which may indicate gallbladder issues like gallstones or cholecystitis. Additionally, jaundice (yellowing of the skin and eyes) and changes in stool or urine color could signify a bile duct obstruction. Reporting these symptoms to a healthcare provider promptly is crucial for early detection and management.
Yes, individuals with a history of gallbladder disease, rapid weight loss, obesity, and those consuming a diet high in fats and low in fiber may be at an increased risk of developing gallbladder problems while on semaglutide. Genetic predispositions and certain medical conditions, such as diabetes, also elevate the risk. Healthcare providers often assess these risk factors before prescribing semaglutide and recommend regular monitoring.
Adopting a healthy lifestyle can significantly mitigate the risk of gallbladder problems. This includes maintaining a balanced diet rich in fiber, avoiding rapid weight loss, staying hydrated, and engaging in regular physical activity. These measures support overall digestive health and may prevent bile stasis and the formation of gallstones.
The management strategy depends on the severity of the gallbladder issue. Mild cases may be managed conservatively with dietary adjustments and pain management, while more severe conditions like acute cholecystitis might require surgical intervention, such as cholecystectomy. In some instances, healthcare providers may also consider adjusting the semaglutide dosage or temporarily discontinuing the medication.
Not necessarily. Patients with a history of gallbladder disease can still be considered for semaglutide therapy but may require closer monitoring for symptoms of gallbladder issues. The decision to use semaglutide should be made on a case-by-case basis, weighing the benefits of the medication against the potential risks, and in close consultation with a healthcare provider.
Regular monitoring may be advised for individuals at higher risk of gallbladder disease or those who develop symptoms suggestive of gallbladder issues while on semaglutide. Monitoring might include clinical evaluations and, if necessary, diagnostic imaging such as ultrasound to assess gallbladder health.
The onset of gallbladder issues after starting semaglutide can vary significantly among individuals. Some patients might experience symptoms within a few months of treatment initiation, while others may not encounter issues until after a year or more of continuous use. The variability depends on several factors, including the individual’s underlying risk factors for gallbladder disease, such as personal or family history of gallstones, rapid weight loss, dietary habits, and overall health status. Continuous monitoring and communication with healthcare providers are essential to catch any issues early.
Not always. The decision to stop semaglutide due to gallbladder issues is highly individualized and depends on the severity of the symptoms, the specific gallbladder condition diagnosed, and the patient’s overall health and treatment goals. In cases of mild gallbladder symptoms, healthcare providers might opt for conservative management while continuing semaglutide, closely monitoring the patient’s condition. For more severe gallbladder issues, such as acute cholecystitis or symptomatic gallstones requiring surgical intervention, pausing semaglutide might be necessary. Ultimately, the course of action should be determined through a detailed discussion between the patient and their healthcare provider, considering the benefits of semaglutide therapy against the risks associated with gallbladder disease.
Yes, semaglutide can often be resumed after resolving gallbladder issues, especially if the medication was effective and well-tolerated for managing diabetes or obesity prior to the onset of gallbladder problems. The decision to restart semaglutide should be made in consultation with a healthcare provider, who will consider the nature of the gallbladder issue, the treatment undertaken (such as cholecystectomy), and the patient’s current health status. For patients who have undergone gallbladder removal, semaglutide can typically be resumed without the same level of risk for gallstone formation, although monitoring for other potential side effects remains important. Resuming semaglutide after addressing gallbladder issues underscores the importance of a personalized approach to treatment, balancing the benefits of the medication with the individual patient’s health considerations.

Dr. Kevin Kargman
Dr. Kevin J. Kargman is a pediatrician in Sewell, New Jersey and is affiliated with multiple hospitals in the area, including Cooper University Health Care-Camden and Jefferson Health-Stratford, Cherry Hill and Washington Township. (Learn More)
