Table of Contents
Introduction
The gut-brain axis is a fascinating and rapidly evolving area of scientific research, revealing the intricate communication network between our digestive system and brain. This axis not only ensures basic digestive functions but also profoundly impacts our mental health, emotions, and overall well-being.
This bidirectional communication system involves the brain influencing gut functions and the gut affecting brain activity. Various pathways, including the nervous system (especially the vagus nerve), the endocrine (hormone) system, and the immune system, mediate this relationship. Signals such as neurotransmitters, hormones, and cytokines facilitate constant dialogue between the gut and the brain.
Understanding the gut-brain axis starts with its components. The gastrointestinal tract, lined with millions of neurons, is often called the “second brain.” These neurons, along with the vast array of gut microbes (the microbiota), are crucial for this communication network. The gut microbiota, comprising trillions of bacteria, viruses, and fungi, has a symbiotic relationship with the host, essential for digestion, immune response, and vitamin production.
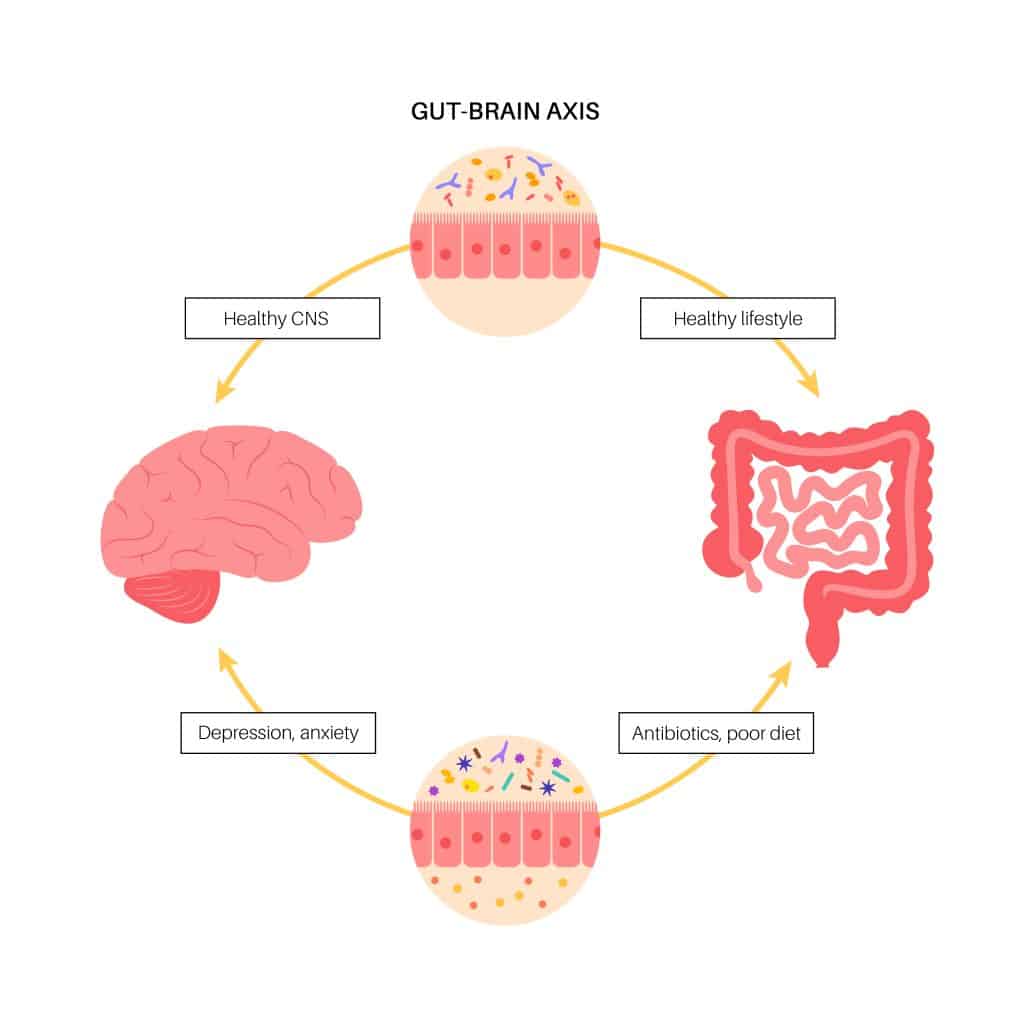
Emerging research shows the gut microbiota also influences brain function and behavior. Changes in gut microbiota composition can affect mood, cognitive abilities, and susceptibility to mental health disorders. For example, studies link specific gut bacteria patterns to conditions like depression, anxiety, and autism spectrum disorder.
The gut-brain axis is influenced by factors such as genetics, diet, stress, and environment. Dietary choices can dramatically impact gut microbiota, affecting mental health. Similarly, stress can alter gut function and microbiota, leading to changes in brain function and emotional state.
Understanding the gut-brain axis is crucial for developing new therapeutic strategies. Interventions targeting the gut microbiota, such as probiotics, prebiotics, and dietary modifications, show potential for improving mental health outcomes. This axis is also pivotal in personalized medicine, where treatments could be tailored based on an individual’s gut microbiota profile.
The gut-brain axis exemplifies the complexity and interconnectedness of our body systems. Its study promises new frontiers in understanding human health and disease, challenging traditional views of the brain and mental health. As research continues to unravel this axis’s mysteries, we approach a paradigm shift in healthcare, aiming for more holistic and effective treatments for various physical and mental health conditions.
Defining the Gut-Brain Axis
The gut-brain axis, a pivotal concept in modern science and wellness, signifies the dynamic communication network between the gut’s enteric nervous system (ENS) and the brain’s central nervous system (CNS). This intricate system involves neural, hormonal, and immune signaling, connecting brain functions with gut activities.
At the core of this axis is the ENS, often called the “second brain,” which controls digestion from the esophagus to the colon with over 100 million neurons. While capable of autonomous function, the ENS maintains constant communication with the CNS, primarily through the vagus nerve. This nerve serves as a direct channel, relaying information between the gut and brain.
The hormonal aspect of the gut-brain axis includes hormones like ghrelin, leptin, and peptide YY, released in response to food intake and gut microbiota state. These hormones regulate appetite, energy balance, and mood, significantly affecting emotional well-being. Notably, the gut produces most of the body’s serotonin, crucial for mood regulation, highlighting the gut’s impact on mental health.
Immune signaling is another vital element. The gut’s extensive immune system interacts with the microbiota, sending signals that can influence brain inflammation and degeneration. This interaction is key to understanding the link between gut health and neurological or psychiatric disorders.
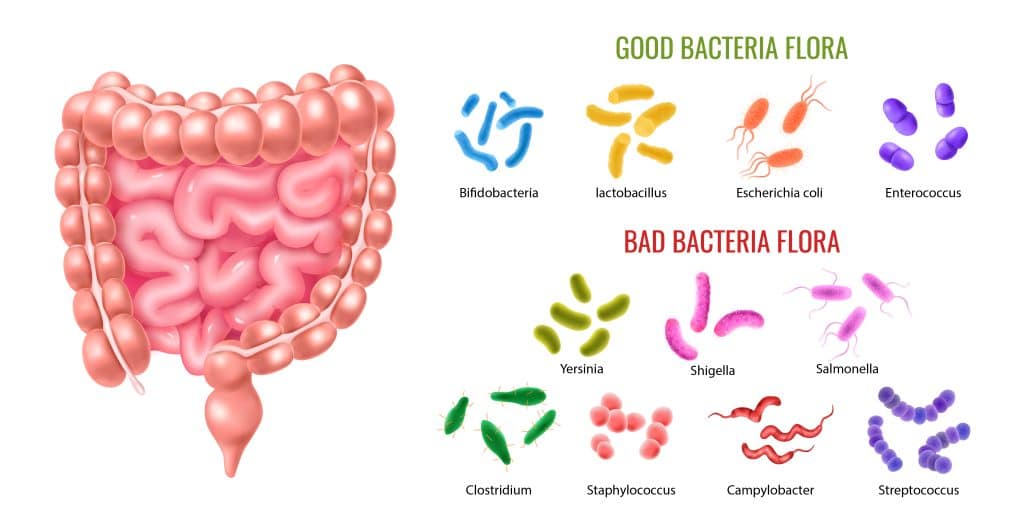
The gut microbiota itself, consisting of trillions of microorganisms, plays a crucial role. These microbes aid digestion, protect against pathogens, and produce neuroactive compounds like short-chain fatty acids (e.g., butyrate) that benefit brain health. Imbalances in this microbiota, known as dysbiosis, can lead to conditions like anxiety, depression, and autism.
Understanding the gut-brain axis has progressed from recognizing a physical connection to appreciating its profound impact on mental health and metabolic disorders. This system’s complexity underscores the interdependence of bodily functions, shedding light on human health’s multifaceted nature. Ongoing research into the gut-brain axis promises to revolutionize therapeutic approaches for various diseases, transforming health and wellness paradigms.
Take Action:
- Improve Your Gut Health: Incorporate a balanced diet rich in fiber, probiotics, and prebiotics.
- Stay Physically Active: Regular exercise supports a healthy gut-brain connection.
- Manage Stress: Practices like mindfulness and meditation can positively impact gut and brain health.
- Consult Healthcare Providers: Seek advice on maintaining a healthy gut-brain axis to enhance overall well-being.
The Role of Microbiota
In the complex landscape of human health, the gut microbiota stands out as a crucial player, especially in the context of the gut-brain axis. This diverse community of microorganisms—including bacteria, fungi, viruses, and protozoa—resides in the gastrointestinal tract and significantly influences gut health and brain function. Our growing understanding of these trillions of organisms has revolutionized our grasp of gut-brain communication.
The gut microbiota is essential for numerous vital processes, such as digestion, vitamin synthesis, and immune system modulation. These microorganisms break down complex carbohydrates, fibers, and proteins, producing essential nutrients and metabolites. They also synthesize important vitamins like vitamin K and some B vitamins, which are crucial for bodily functions.
Beyond these physical roles, the gut microbiota significantly shapes the body’s immune response. Through interactions with gut immune cells, the microbiota helps distinguish between harmful pathogens and benign molecules, training the immune system and enhancing overall immune response.
One of the most intriguing roles of the gut microbiota is its communication with the brain, a key component of the gut-brain axis. This occurs through neural, endocrine, and immune pathways. For instance, gut bacteria produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which regulate mood and anxiety. These neurotransmitters can directly or indirectly influence brain function through interactions with the immune system and the vagus nerve.
The composition of the gut microbiota is influenced by genetics, diet, lifestyle, and environmental factors. Diet plays a pivotal role—fiber-rich diets with fruits and vegetables promote a diverse, healthy microbiota, while diets high in processed foods and sugars can cause an imbalance, or dysbiosis. Dysbiosis has been linked to various health issues, including inflammatory bowel diseases, obesity, diabetes, and mental health disorders like depression and anxiety.
Research indicates that changes in gut microbiota composition can significantly impact brain function and behavior. Studies in humans and animals show that alterations in the gut microbiota affect stress responses, emotional behavior, and cognitive functions. This has led to exploring therapeutic interventions targeting the gut microbiota for treating neurological and psychiatric conditions.
The gut microbiota is a dynamic and complex entity crucial for human health. Its interaction with the brain via the gut-brain axis opens new avenues for understanding disease pathophysiology and developing novel therapies. As research continues, it becomes clear that the health of our gut microbiota is intrinsically linked to our overall physical and mental well-being.
Gut-Brain Axis and Mental Health
The gut-brain axis has revealed a profound connection between gut health and mental well-being, influencing mood, stress response, and susceptibility to psychiatric disorders. Understanding this link is crucial for developing innovative mental health treatments and preventive strategies.
At the heart of this connection is the gut microbiota, whose health and diversity directly affect brain function. The microbiota communicates with the brain through neural (vagus nerve), endocrine, and immune pathways, impacting emotional and cognitive processes.
One direct influence of the gut on mental health is through neurotransmitter production. A significant portion of serotonin, crucial for mood regulation, is produced in the gut. Imbalances in serotonin levels are linked to depression and anxiety disorders.
The gut microbiota also modulates the body’s stress response via the hypothalamic-pituitary-adrenal (HPA) axis. Changes in gut microbiota composition can affect HPA axis development and function, influencing stress responses, particularly following early-life stress.
Emerging research indicates a connection between gut microbiota and neurodevelopmental disorders like autism spectrum disorder (ASD). Individuals with ASD often have distinct microbiota profiles and gastrointestinal issues, suggesting the gut-brain axis may play a role in ASD symptom development or exacerbation.
Inflammation is another critical factor, with gut health influencing mental health through inflammatory processes. Gut inflammation can produce cytokines that cross the blood-brain barrier, potentially contributing to mood and anxiety disorders.
The concept of “psychobiotics”—probiotics that positively impact mental health—highlights the potential of modulating gut microbiota to enhance brain function. This offers a promising path for new mental health treatments.
The gut-brain axis is fundamental to mental health, affecting everything from mood and stress response to psychiatric disorder development. This knowledge advocates for a holistic approach to mental health care, integrating gut health as essential to mental wellness. As research progresses, it promises to transform mental health treatment with more comprehensive and effective strategies.
Nutrition and the Gut-Brain Axis
The profound connection between diet, gut microbiota, and brain health is a burgeoning field in both nutrition and mental health sciences. The foods we consume significantly shape our gut microbiota, impacting brain health and overall well-being.
Diet and Gut Microbiota:
Our gut microbiota thrives on the nutrients we ingest, and its composition can be rapidly influenced by dietary changes. Diets rich in diverse plant-based foods provide fibers, vitamins, and minerals that support a healthy microbial community. These fibers are fermented by gut bacteria, producing short-chain fatty acids (SCFAs) like butyrate, propionate, and acetate. SCFAs are essential for colon cells, immune function, inflammation regulation, and maintaining blood-brain barrier integrity.
In contrast, diets high in processed foods, sugars, and saturated fats promote a less diverse and more inflammatory gut environment. This dysbiosis can increase intestinal permeability (leaky gut) and systemic inflammation, which are linked to mental health issues such as depression and anxiety.
Mediterranean Diet Benefits:
The Mediterranean diet, rich in fruits, vegetables, whole grains, olive oil, and fish, supports a beneficial gut microbiota. This diet is not only heart-healthy but also promotes mental health, potentially reducing the risk of depression and cognitive decline due to its positive impact on the gut-brain axis.
Polyphenols and Mental Health:
Polyphenols, found in berries, nuts, and tea, have antioxidant properties and can modulate the gut microbiota to benefit brain health. Emerging research highlights their potential role in supporting mental well-being.
Probiotics and Prebiotics:
Probiotics (live microorganisms) and prebiotics (dietary fibers) improve gut health by selectively feeding beneficial bacteria. Both have shown promise in enhancing mental health outcomes, such as reducing symptoms of depression and anxiety, through their effects on the gut-brain axis.
Action Steps:
- Adopt a Mediterranean Diet: Incorporate more fruits, vegetables, whole grains, olive oil, and fish into your diet.
- Increase Fiber Intake: Choose a variety of plant-based foods to support a diverse gut microbiota.
- Limit Processed Foods: Reduce consumption of processed foods, sugars, and saturated fats to prevent dysbiosis.
- Consider Polyphenol-Rich Foods: Include berries, nuts, and tea in your diet for their potential brain health benefits.
- Explore Probiotics and Prebiotics: Consider adding probiotic and prebiotic-rich foods or supplements to your routine.
A balanced, nutrient-rich diet is crucial for physical and mental health. Understanding and improving our dietary habits can significantly influence gut microbiota and, consequently, brain function and mental well-being. This underscores the importance of nutrition in managing and preventing mental health disorders, highlighting the interconnectedness of diet, gut health, and brain function.
The Gut-Brain Axis and Neurological Disorders
The gut-brain axis is revolutionizing our understanding of neurological disorders. The health of the gastrointestinal system, particularly the gut microbiota, plays a critical role in the development and progression of conditions like Parkinson’s disease (PD), Alzheimer’s disease (AD), and multiple sclerosis (MS).
Parkinson’s Disease
PD is a neurodegenerative disorder marked by tremors, rigidity, and slowed movement. Recent research links gut health to PD, suggesting that gut microbiota changes may precede and contribute to PD pathology. Early gastrointestinal symptoms, such as constipation, often appear before motor symptoms. The presence of alpha-synuclein, a protein linked to PD, in the gut’s nervous system supports the idea that PD might originate in the gut and spread to the brain via the gut-brain axis.
Alzheimer’s Disease
AD, the leading cause of dementia, is characterized by amyloid-beta plaques and tau tangles in the brain, leading to cognitive decline. Emerging evidence suggests that gut microbiota dysbiosis can influence these brain changes. Gut-originated inflammation can worsen neuroinflammation, a key factor in AD progression. Certain gut bacteria produce amyloid and other neurotoxic substances, potentially contributing to AD.
Multiple Sclerosis
MS is a chronic autoimmune disease that damages the myelin sheath of neurons, causing various neurological symptoms. Research shows that MS patients often have altered gut microbiota, which may impact disease severity and progression. The gut microbiota affects MS through its role in modulating the immune system and potentially influencing the autoimmune response.
Therapeutic Potential
Targeting the gut microbiota offers promising therapeutic strategies for neurological disorders. Interventions like probiotics, prebiotics, dietary changes, and fecal microbiota transplantation are being investigated for their potential to alter disease progression.
The gut-brain axis is crucial in the development and progression of neurological disorders. Understanding the interplay between gut microbiota and brain health can shift our approach to these conditions. Ongoing research in this field promises new interventions targeting the gut to mitigate neurological diseases, offering hope for improved treatments and preventive strategies.
Probiotics, Prebiotics, and Brain Health
In the intricate world of the gut-brain axis, probiotics and prebiotics emerge as key players influencing brain health. Their ability to modulate gut microbiota offers a pathway to treating mental health and neurological disorders.
Probiotics: Beneficial Microorganisms
Probiotics are live microorganisms that, when taken in sufficient amounts, confer health benefits. These beneficial bacteria help maintain a healthy gut microbiota balance, crucial for both gut and brain health. Probiotics influence brain health by:
- Modulating gut microbiota composition
- Enhancing intestinal barrier function
- Reducing inflammation
- Producing neurotransmitters and bioactive compounds
Certain strains, known as “psychobiotics,” alleviate symptoms of depression and anxiety by reducing inflammation, modulating the stress response, and producing neurotransmitter precursors like tryptophan, a serotonin precursor.
Prebiotics: Fuel for Healthy Bacteria
Prebiotics are non-digestible food components that promote the growth of beneficial gut microorganisms. Found in dietary fibers and complex carbohydrates such as inulin, FOS, and GOS, prebiotics improve gut microbiota composition and health. This positively affects brain function and mental health by influencing the gut-brain axis.
Synbiotics: A Powerful Combination
Combining probiotics and prebiotics, known as synbiotics, enhances gut microbiota diversity and functionality. This synergy improves gut barrier integrity and reduces inflammation, benefiting brain health. Research indicates synbiotics may:
- Aid in neurodevelopmental disorders
- Support cognitive function in neurodegenerative diseases
- Enhance cognitive function in healthy individuals
The Potential of Probiotics and Prebiotics
Emerging research suggests probiotics and prebiotics may play roles in neurodevelopmental and neurodegenerative diseases and improve cognitive function. For instance, probiotics have shown cognitive benefits in Alzheimer’s patients, while prebiotics can enhance sleep and stress resilience.
The exploration of probiotics and prebiotics in the gut-brain axis offers promising potential for mental health and neurology. By modulating gut microbiota, these substances present novel therapeutic approaches for brain-related conditions. As research evolves, the connection between gut microbiota health and mental well-being becomes increasingly clear. Prioritize gut health for both physical and cognitive benefits.
The Impact of Stress on the Gut-Brain Axis
Stress profoundly impacts the gut-brain axis, a critical mediator of the relationship between psychological factors and physical health, especially gastrointestinal function and overall well-being.
Stress Response and Gut Impact
Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, releasing cortisol and other stress hormones to prepare the body for perceived threats. Chronic stress can lead to a host of health problems, particularly affecting the gut-brain axis.
The gut is highly sensitive to stress, which can disrupt gut motility, increase gut permeability (commonly known as “leaky gut”), and alter the balance of gut microbiota. These changes often result in gastrointestinal issues like indigestion, heartburn, and irritable bowel syndrome (IBS). Moreover, an imbalanced gut microbiota and increased intestinal permeability can trigger systemic inflammation, further impacting brain function and contributing to anxiety and depression.
Gut’s Role in Stress Response
The gut’s health significantly influences the body’s stress response. A balanced gut microbiota is essential for the proper functioning of the HPA axis. Certain beneficial gut bacteria, like Lactobacillus and Bifidobacterium, produce neurotransmitters such as gamma-aminobutyric acid (GABA), which help reduce anxiety and regulate the stress response.
Interventions and Holistic Approaches
The bi-directional relationship between stress and the gut-brain axis suggests that interventions targeting either can benefit the other. Stress reduction techniques such as mindfulness, meditation, and yoga have been shown to positively affect gut health by modulating the gut microbiota and reducing inflammation. Similarly, dietary strategies that promote a healthy gut microbiota, including the use of probiotics and prebiotics, can mitigate the physiological impacts of stress.
Understanding the complex, bidirectional relationship between stress and the gut-brain axis is crucial for developing holistic approaches to managing stress and its effects on the body. As research in this field expands, it offers new avenues for preventing and treating stress-related conditions by targeting the gut-brain axis. Prioritize stress management and gut health to improve overall well-being and mental health.
GLP-1 Medications and Their Impact on the Gut-Brain Axis
The interplay between GLP-1 (Glucagon-Like Peptide-1) medications, particularly Semaglutide, and the gut-brain axis is a burgeoning field of interest. Originally designed to treat type 2 diabetes, these medications are now recognized for their potential in weight management and neurological health.
GLP-1 is a hormone produced in the gut in response to food intake, crucial for glucose metabolism, insulin secretion, and glucagon inhibition. By slowing gastric emptying and promoting satiety, GLP-1 plays a vital role in weight management. Medications like Semaglutide mimic this hormone, aiding in blood sugar control and weight loss.
These medications significantly impact the gut-brain axis. By slowing gastric emptying, they enhance the feeling of fullness and reduce appetite, aiding in weight loss without restrictive diets. Additionally, GLP-1 receptors in the brain’s appetite-regulating areas, such as the hypothalamus, are directly influenced by these medications, further promoting weight loss.
Emerging research highlights the neuroprotective effects of GLP-1 medications. Studies suggest that GLP-1 receptor agonists like Semaglutide improve neuronal insulin signaling, reduce oxidative stress, and lower brain inflammation. This has potential implications for treating neurodegenerative diseases like Alzheimer’s and Parkinson’s.
Moreover, GLP-1 medications may play a role in mood regulation and mental health. The gut-brain axis is crucial in mood disorders, and influencing this axis with GLP-1 medications could open new treatment avenues for depression and anxiety.
The impact of GLP-1 medications, especially Semaglutide, on the gut-brain axis marks a significant advancement in metabolic and neurological health. These medications not only aid in diabetes management and weight loss but also offer promising neuroprotective and mental health benefits. As research progresses, the full scope of their impact will become clearer, potentially revolutionizing treatment across various medical fields.
Future Directions in Gut-Brain Axis Research
The exploration of the gut-brain axis marks a new era in biomedical research, with the potential to revolutionize our understanding of health and disease. This intricate interplay between gut microbiota and the brain opens doors to innovative therapies for a wide range of conditions.
Mental Health Disorders:
The gut-brain axis offers new insights into depression, anxiety, and schizophrenia. Research is now focusing on how gut microbiota influence these conditions, paving the way for treatments like probiotics, prebiotics, and dietary changes. These strategies aim to modify gut microbiota to enhance mental health, providing an alternative to conventional medications.
Neurological Diseases:
Emerging evidence links gut microbiota to neurological diseases such as Parkinson’s and Alzheimer’s. Future studies aim to decode these mechanisms, potentially leading to early diagnosis and novel treatments. Using gut microbiota profiles as biomarkers could provide critical insights into disease progression and response to therapy.
Autoimmune Diseases:
Research is intensifying on the gut-brain axis’s role in autoimmune diseases like multiple sclerosis. Understanding how gut microbiota impact the immune system may lead to new treatments that modulate gut microbiota, offering alternatives or supplements to current immune therapies.
Aging and Cognitive Decline:
As the population ages, maintaining cognitive health is crucial. Studies on how aging affects gut microbiota and, in turn, brain health could result in preventive strategies and treatments for cognitive decline.
Personalized Medicine:
The unique nature of each individual’s microbiota presents a significant opportunity for personalized medicine. Tailoring probiotics and prebiotics to an individual’s specific gut microbiota profile could prove more effective than generic treatments, enhancing the efficacy of dietary and therapeutic interventions.
The future of gut-brain axis research is bright and full of promise. From mental health and neurology to autoimmune diseases and aging, the potential for groundbreaking discoveries is immense. As we unravel the complexities of this communication network, we inch closer to novel treatments, early diagnoses, and effective preventive strategies, underscoring the holistic interconnectedness of our body systems.
Conclusion
The exploration of the gut-brain axis has revolutionized our understanding of health and disease, breaking traditional boundaries in neuroscience, microbiology, and gastroenterology. This complex communication network between the gut and brain significantly impacts mental health, neurological function, immune response, and overall well-being.
Recent research confirms that the gut-brain axis is fundamental to human physiology, with profound clinical implications. Discovering that our gut microbiota can affect brain function and behavior represents a paradigm shift in understanding mental health and neurological disorders. This connection promotes a holistic approach to treatment, incorporating diet, probiotics, and prebiotics as potential non-pharmacological interventions for mental health care.
In neurology, the gut-brain axis offers valuable insights into diseases like Parkinson’s, Alzheimer’s, and multiple sclerosis. Understanding how gut microbiota changes influence these conditions opens up innovative diagnostic and therapeutic strategies. Using gut microbiota composition as a biomarker for neurological diseases holds promise for non-invasive early detection and personalized treatment plans.
The gut-brain axis underscores the importance of a holistic approach to health, highlighting the interconnectedness of body systems and the need for comprehensive treatment strategies. This perspective is crucial in managing chronic conditions and preventive health care, where maintaining a healthy gut microbiota can have widespread benefits.
Interdisciplinary collaboration has been pivotal in unraveling the complexities of the gut-brain axis. As we delve deeper into this field, cross-disciplinary partnerships will be essential for advancing our understanding and translating research into effective clinical practices.
The study of the gut-brain axis challenges us to rethink health and disease, advocating for integrative strategies that consider both the gut and the brain. As research progresses, it promises to enhance our ability to prevent and treat various conditions, ultimately improving the quality of life worldwide.
Learn more about the cost of semaglutide with BMI Doctors.
Research Citations
The gut-brain axis represents a bidirectional communication network between the gastrointestinal tract and the central nervous system, encompassing neural, endocrine, and immune pathways. Understanding the intricate mechanisms underlying this axis has profound implications for various aspects of health and disease, including metabolism, mood regulation, immune function, and neurological disorders. This article reviews current research on the gut-brain axis, highlighting its significance in maintaining homeostasis and potential therapeutic targets for a range of conditions.
- Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 2012;13(10):701-712. doi:10.1038/nrn3346
- Mayer EA, Knight R, Mazmanian SK, Cryan JF, Tillisch K. Gut microbes and the brain: paradigm shift in neuroscience. J Neurosci. 2014;34(46):15490-15496. doi:10.1523/JNEUROSCI.3299-14.2014
- Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305-312. doi:10.1016/j.tins.2013.01.005
- Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203-209.
- Sharon G, Sampson TR, Geschwind DH, Mazmanian SK. The central nervous system and the gut microbiome. Cell. 2016;167(4):915-932. doi:10.1016/j.cell.2016.10.027
- Cryan JF, O’Riordan KJ, Cowan CSM, et al. The microbiota-gut-brain axis. Physiol Rev. 2019;99(4):1877-2013. doi:10.1152/physrev.00018.2018
- Grenham S, Clarke G, Cryan JF, Dinan TG. Brain-gut-microbe communication in health and disease. Front Physiol. 2011;2:94. doi:10.3389/fphys.2011.00094
- Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125(3):926-938. doi:10.1172/JCI76304
- Rhee SH, Pothoulakis C, Mayer EA. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6(5):306-314. doi:10.1038/nrgastro.2009.35
- Burokas A, Moloney RD, Dinan TG, Cryan JF. Microbiota regulation of the mammalian gut-brain axis. Adv Appl Microbiol. 2015;91:1-62. doi:10.1016/bs.aambs.2015.02.001
These references offer a comprehensive overview of the gut-brain axis, highlighting its multifaceted mechanisms and implications for various aspects of health and disease.
Questions and Answers: Gut-Brain Axis
The gut-brain axis refers to the bidirectional communication network that links the central nervous system (including the brain) with the enteric nervous system of the gastrointestinal tract. This communication occurs through various channels, including neural pathways (like the vagus nerve), hormonal signals, and immune system interactions. The gut-brain axis plays a crucial role in regulating digestive processes, mood, mental health, and overall well-being.
The gut microbiota, composed of trillions of microorganisms, influences mental health through several mechanisms. These microbes can produce neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), which play a role in mood regulation. They also interact with the immune system, influencing inflammation levels, which can impact the brain. Additionally, the gut microbiota affects the body’s stress response, which can have mental health implications.
Yes, diet plays a significant role in the health of the gut-brain axis. A diet rich in diverse fruits, vegetables, whole grains, and fermented foods can promote a healthy and diverse gut microbiota, which is beneficial for brain health. On the other hand, diets high in processed foods and sugars can negatively affect gut microbiota diversity and lead to increased inflammation, potentially impacting mental health.
Research suggests that imbalances in the gut microbiota may contribute to the development of neurological disorders such as Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis. These imbalances may lead to increased inflammation and changes in neural communication, which could play a role in the pathology of these diseases.
There is growing evidence that certain probiotics, sometimes referred to as “psychobiotics,” may have beneficial effects on mental health. These probiotics can influence the gut microbiota and, consequently, the gut-brain axis, potentially alleviating symptoms of depression, anxiety, and other mood disorders. However, more research is needed to fully understand their efficacy and to identify specific strains that are most effective.
Stress can significantly impact the gut-brain axis. It can alter gut motility, affect the integrity of the gut lining, and change the composition of the gut microbiota. These changes can lead to gastrointestinal issues and can also impact mental health, as the altered gut microbiota can affect mood and stress responses.
GLP-1 medications, such as Semaglutide, primarily used for diabetes and weight management, also affect the gut-brain axis. They act on GLP-1 receptors in the brain and gut, influencing appetite regulation and insulin sensitivity. There is emerging research into their potential neuroprotective effects and their impact on conditions like Alzheimer’s and Parkinson’s diseases.
Future research on the gut-brain axis is vast and varied, encompassing the development of new treatments for mental and neurological disorders, understanding the role of diet and microbiota in brain health, and exploring the potential of personalized medicine based on individual gut microbiota profiles. There is also ongoing research into how early-life gut microbiota influences long-term brain health and behavior.
While altering the gut microbiota presents a promising avenue for treating certain mental health issues, it is not a standalone solution. Mental health disorders are complex and multifactorial. However, strategies that include modifying the gut microbiota through diet, probiotics, and prebiotics can be valuable components of a more comprehensive mental health treatment plan.
Absolutely, the gut-brain axis is relevant for everyone. Maintaining a healthy gut microbiota can benefit brain health, mood, cognitive function, and overall well-being. A balanced diet, regular exercise, stress management, and possibly the use of probiotics and prebiotics can all contribute to a healthy gut-brain axis.

Dr. Melissa VanSickle
Dr. Melissa Vansickle, MD is a family medicine specialist in Onsted, MI and has over 24 years of experience in the medical field. She graduated from University of Michigan Medical School in 1998. She is affiliated with medical facilities Henry Ford Allegiance Health and Promedica Charles And Virginia Hickman Hospital. Her subspecialties include General Family Medicine, Urgent Care, Complementary and Integrative Medicine in Rural Health.
