Table of Contents
Introduction
Semaglutide is a medication that many people use to help manage their blood sugar levels, particularly those with type 2 diabetes. It has also gained popularity for its role in weight management. This medication, part of a class of drugs known as GLP-1 receptor agonists, helps to regulate insulin and lower blood sugar levels by mimicking a hormone called glucagon-like peptide-1 (GLP-1). While semaglutide offers significant benefits, it also comes with potential side effects, one of which is stomach paralysis, also known as gastroparesis.
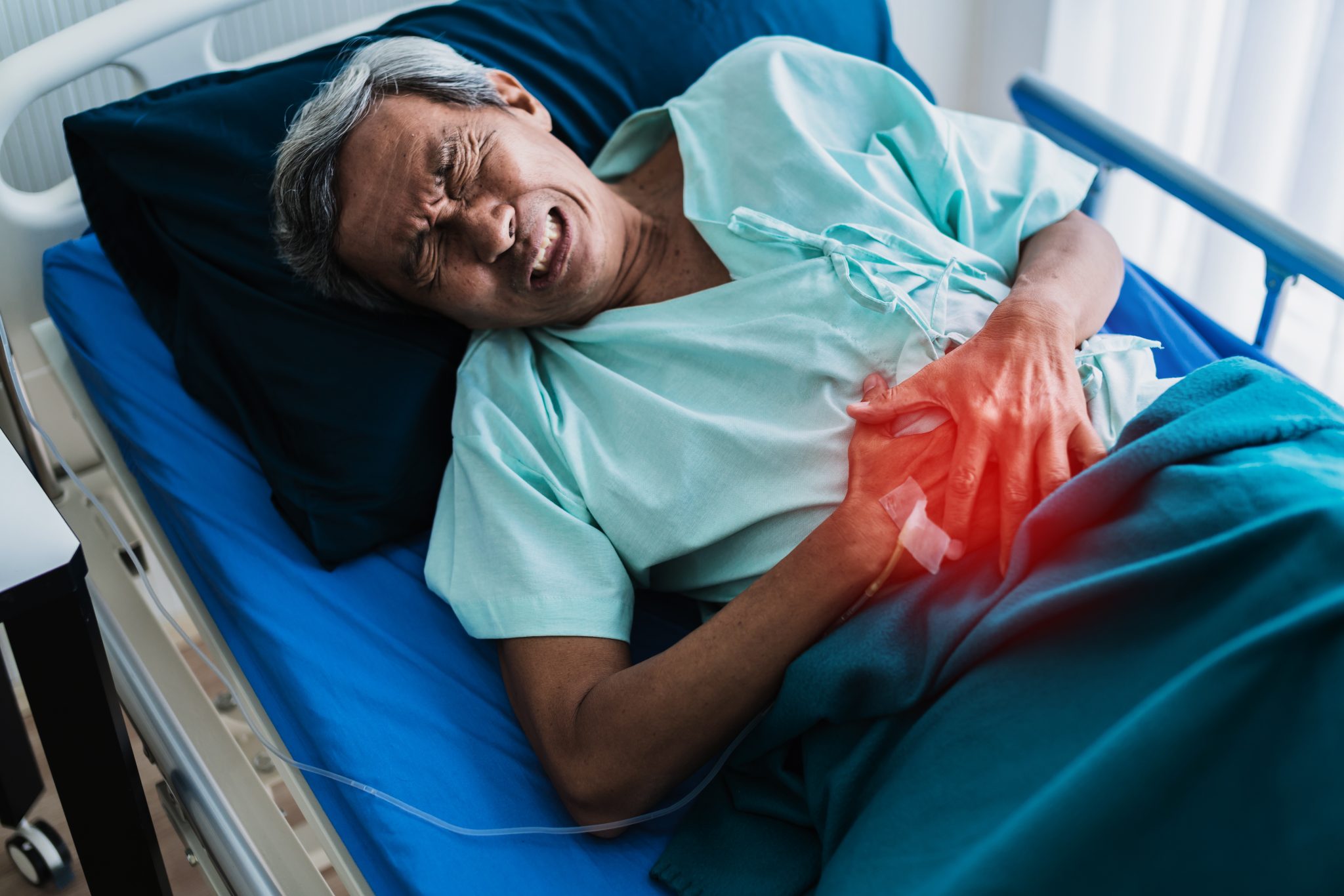
Stomach paralysis is a condition where the stomach muscles are unable to move food effectively through the digestive system. This leads to delayed emptying of the stomach contents into the small intestine. Symptoms of stomach paralysis can include nausea, vomiting, bloating, and a feeling of fullness after eating only a small amount of food. This condition can significantly impact a person’s quality of life and nutritional status.
The purpose of this article is to explore the relationship between semaglutide and stomach paralysis. We will delve into how semaglutide works in the body, examine whether it can cause stomach paralysis, and discuss the symptoms, risk factors, and management of this condition. By understanding these aspects, readers can make informed decisions about their health and treatment options.
Understanding the potential link between semaglutide and stomach paralysis is crucial because it helps patients and healthcare providers monitor and manage this possible side effect. While semaglutide has proven to be effective in controlling blood sugar levels and aiding weight loss, being aware of its possible impacts on stomach function allows for better treatment plans and patient outcomes.
Stomach paralysis, or gastroparesis, can occur for various reasons, including diabetes, infections, and certain medications. When the stomach muscles do not function properly, food remains in the stomach longer than it should, leading to discomfort and other digestive issues. This can cause a range of symptoms that vary in severity from mild to debilitating.
Semaglutide’s role in potentially causing stomach paralysis involves its action on the gut. Since GLP-1 receptor agonists like semaglutide slow gastric emptying as part of their mechanism to promote satiety and reduce blood sugar spikes, there is a concern that this effect might contribute to or worsen gastroparesis in some individuals. Understanding this connection is essential for patients who use semaglutide, especially those who might already be at risk for digestive complications.
This article will also address common questions and concerns about semaglutide and stomach paralysis. For instance, readers often want to know if everyone who takes semaglutide is at risk, what symptoms to look out for, and how to manage any digestive issues that arise while using this medication. By providing comprehensive answers, we aim to equip readers with the knowledge they need to recognize potential side effects early and seek appropriate medical advice.
In the following sections, we will discuss what semaglutide is, how it works in the body, and the specifics of stomach paralysis. We will then examine the evidence linking semaglutide to stomach paralysis and provide guidance on recognizing symptoms, managing the condition, and taking preventive measures. This holistic approach will help readers understand both the benefits and risks of semaglutide, ensuring they are well-informed about their treatment options.
In summary, semaglutide is a valuable medication for managing diabetes and aiding in weight loss, but it is important to be aware of its potential side effects, including stomach paralysis. By exploring this issue in detail, we aim to provide clear, understandable information that can help patients and healthcare providers navigate the complexities of treatment with semaglutide. The goal is to support informed decision-making and promote better health outcomes for those using this medication.
What is Semaglutide?
Semaglutide is a medication that has gained significant attention in recent years, primarily for its use in treating type 2 diabetes and assisting with weight management. It belongs to a class of drugs known as GLP-1 receptor agonists. Understanding what semaglutide is, how it works, and its common uses can help you grasp why it’s important to discuss its potential side effects, like stomach paralysis.
Definition and Classification
Semaglutide is a synthetic version of a naturally occurring hormone called GLP-1 (glucagon-like peptide-1). GLP-1 is produced in the intestines and plays a crucial role in regulating blood sugar levels and appetite. Semaglutide mimics the action of GLP-1, which helps control blood sugar levels in people with type 2 diabetes.
Semaglutide is available under several brand names, including Ozempic® and Rybelsus®, and it can be administered either through injections or as an oral tablet. It is classified as a GLP-1 receptor agonist, meaning it activates the GLP-1 receptors in the body to exert its effects.
Mechanism of Action
The primary way semaglutide works is by stimulating the GLP-1 receptors in the body. When these receptors are activated, several beneficial effects occur:
- Increased Insulin Secretion: Semaglutide helps the pancreas release more insulin in response to meals. Insulin is a hormone that lowers blood sugar levels by helping cells take in glucose from the blood.
- Reduced Glucagon Secretion: Glucagon is a hormone that raises blood sugar levels by stimulating the liver to produce glucose. Semaglutide decreases the secretion of glucagon, helping to keep blood sugar levels in check.
- Slowed Gastric Emptying: Semaglutide slows down the rate at which food leaves the stomach and enters the intestines. This helps prevent spikes in blood sugar levels after meals and also contributes to a feeling of fullness, which can aid in weight loss.
- Appetite Suppression: By acting on the brain, semaglutide reduces hunger and cravings, making it easier for people to stick to a healthy diet and lose weight.
Common Uses in Diabetes and Weight Management
Type 2 Diabetes
Semaglutide is primarily prescribed for people with type 2 diabetes, a condition where the body either resists the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels. Managing blood sugar is crucial for preventing the complications of diabetes, which can include heart disease, nerve damage, kidney failure, and vision problems.
By enhancing insulin secretion, reducing glucagon levels, and slowing gastric emptying, semaglutide helps maintain steady blood sugar levels throughout the day. This can lead to better overall control of diabetes and a lower risk of long-term complications.
Weight Management
In addition to its role in managing diabetes, semaglutide has also been approved for use in weight management. For individuals who are overweight or obese, losing weight can significantly reduce the risk of developing type 2 diabetes and other health issues like heart disease and stroke.
Semaglutide helps with weight loss by suppressing appetite and slowing the emptying of the stomach. These effects make individuals feel fuller for longer periods, reducing the overall amount of food consumed. Clinical trials have shown that semaglutide can lead to substantial weight loss when combined with lifestyle changes such as diet and exercise.
Semaglutide is a powerful medication that offers significant benefits for managing type 2 diabetes and aiding in weight loss. By mimicking the natural hormone GLP-1, it helps regulate blood sugar levels, reduce appetite, and promote weight loss. Understanding these aspects of semaglutide provides a foundation for exploring its potential side effects, including its impact on stomach health. As we delve deeper into the relationship between semaglutide and stomach paralysis, it’s important to keep in mind how this medication functions and why it is widely used in medical practice.
Understanding Stomach Paralysis (Gastroparesis)
Stomach paralysis, also known as gastroparesis, is a condition where the stomach cannot empty food properly. This happens because the muscles in the stomach are either weak or do not work as they should. When the stomach muscles do not function correctly, it causes delays in moving food into the small intestine. Understanding this condition is important, especially for people taking medications like semaglutide, which may affect how the stomach works.
Definition and Symptoms
Gastroparesis means that the stomach is paralyzed or partially paralyzed. This condition can cause a range of symptoms. Some common symptoms of gastroparesis include:
- Nausea: Feeling like you need to vomit
- Vomiting: Throwing up food that has not been digested
- Bloating: Feeling full and tight in your stomach
- Abdominal Pain: Stomach pain that can be sharp or dull
- Early Satiety: Feeling full quickly after starting to eat
- Weight Loss: Losing weight without trying
- Poor Appetite: Not feeling hungry or wanting to eat
These symptoms can vary in intensity from mild to severe and may come and go.
Causes and Risk Factors
Several factors can cause or contribute to gastroparesis. Understanding these can help identify who is at risk. Here are some common causes and risk factors:
- Diabetes: High blood sugar levels can damage the nerves that control the stomach muscles.
- Surgery: Operations on the stomach or other parts of the digestive system can affect how the stomach works.
- Infections: Some viral infections can lead to gastroparesis.
- Medications: Certain medications, including some for pain, depression, and diabetes, can slow stomach emptying.
- Nervous System Diseases: Conditions like Parkinson’s disease or multiple sclerosis can affect stomach muscles.
- Hypothyroidism: Low levels of thyroid hormones can slow down bodily functions, including digestion.
- Autoimmune Diseases: Conditions where the immune system attacks the body, like lupus, can cause gastroparesis.
Diagnosis and Impact on Health
Diagnosing gastroparesis involves several steps. A doctor will start by reviewing the patient’s symptoms and medical history. Then, they may order tests to see how well the stomach is emptying food. Some common tests include:
- Gastric Emptying Study: This test measures how long it takes for food to leave the stomach.
- Upper Endoscopy: A flexible tube with a camera is used to look inside the stomach and small intestine.
- Ultrasound: Sound waves are used to create images of the stomach and surrounding organs.
- SmartPill: A small, swallowable device that sends information about how the stomach and intestines are working.
Gastroparesis can have a significant impact on a person’s health and quality of life. Because food is not moving through the digestive system as it should, people with gastroparesis may not get all the nutrients they need. This can lead to malnutrition and weight loss. Persistent vomiting can also cause dehydration and electrolyte imbalances. Additionally, gastroparesis can make controlling blood sugar levels more difficult for people with diabetes, leading to further complications.
Managing Gastroparesis
While there is no cure for gastroparesis, there are ways to manage the symptoms and improve quality of life. Here are some management strategies:
- Dietary Changes: Eating smaller, more frequent meals that are easier to digest can help. Pureed or liquid foods are often recommended.
- Medications: There are medications that can help stimulate stomach muscles or manage symptoms like nausea and vomiting.
- Lifestyle Changes: Regular exercise, avoiding lying down after eating, and quitting smoking can also help manage symptoms.
Understanding gastroparesis is important, especially for people taking medications that might affect their stomach, like semaglutide. Recognizing the symptoms and knowing the causes and risk factors can help in seeking timely medical advice and managing the condition effectively. If you suspect you have gastroparesis, it is important to talk to your doctor for proper diagnosis and treatment options.

How Does Semaglutide Work in the Body?
Semaglutide is a medication commonly used to treat type 2 diabetes and help with weight loss. It works by mimicking a hormone in the body called glucagon-like peptide-1 (GLP-1). This hormone plays a key role in regulating blood sugar levels and appetite. Understanding how semaglutide works in the body can help us see why it might cause stomach problems like stomach paralysis.
Detailed Mechanism of Action
When you eat, your body releases GLP-1. This hormone helps your pancreas release insulin, which lowers your blood sugar levels. It also slows down the movement of food from your stomach into your small intestine, helping you feel full longer. Semaglutide, being similar to GLP-1, does the same things. It helps your body manage blood sugar levels by boosting insulin release when your blood sugar is high and by reducing the amount of sugar your liver makes.
Effects on Gastrointestinal Motility
Gastrointestinal motility refers to the movement of food through your digestive system. One of the effects of semaglutide is to slow down this movement. Normally, food moves from your stomach into your small intestine, where nutrients are absorbed. By slowing down this process, semaglutide helps you feel full longer, which can be very helpful for weight loss. However, this same action can sometimes lead to problems.
When the movement of food is slowed too much, it can cause a condition called gastroparesis, or stomach paralysis. In gastroparesis, the stomach takes too long to empty its contents. This can cause a range of symptoms, including nausea, vomiting, and a feeling of fullness after eating only a small amount of food.
Interaction with Other Bodily Systems
Semaglutide doesn’t just affect the stomach. It interacts with several other systems in the body. For example, it helps control blood sugar levels, which is crucial for people with diabetes. It also affects appetite control, helping people eat less and lose weight. But these beneficial effects can sometimes come with side effects.
The hormone GLP-1, which semaglutide mimics, is part of a complex system that includes the brain, stomach, pancreas, and liver. By interacting with this system, semaglutide can have wide-ranging effects. For instance, in the brain, it helps reduce appetite. In the pancreas, it helps release insulin. In the stomach, it slows down digestion.
Potential Side Effects
While semaglutide can be very effective, it is important to be aware of its potential side effects. The most common side effects are related to the gastrointestinal system. These include nausea, diarrhea, vomiting, and constipation. These side effects are usually mild and go away after a few weeks as your body adjusts to the medication.
However, in some cases, the effect on the stomach’s motility can be more severe, leading to stomach paralysis. When this happens, the symptoms can be more serious and persistent. If you experience severe nausea, vomiting, or a feeling of fullness that doesn’t go away, it’s important to talk to your doctor.
Balancing Benefits and Risks
For many people, the benefits of semaglutide outweigh the risks. It can help manage blood sugar levels, reduce the risk of heart disease, and promote weight loss. But like all medications, it’s important to use it under the guidance of a healthcare professional who can monitor for side effects and adjust the treatment if necessary.
Semaglutide works by mimicking the GLP-1 hormone, helping to regulate blood sugar levels and control appetite. While it is very effective for these purposes, its effects on gastrointestinal motility can sometimes lead to side effects like stomach paralysis. Understanding how semaglutide works in the body helps explain why these side effects can occur and highlights the importance of using this medication under the supervision of a healthcare provider. If you experience any severe or persistent symptoms while taking semaglutide, it’s important to seek medical advice.
Can Semaglutide Cause Stomach Paralysis?
Semaglutide is a medication often prescribed for managing diabetes and helping with weight loss. However, like many medications, it can have side effects. One of the more serious potential side effects is stomach paralysis, also known as gastroparesis. In this section, we will explore whether semaglutide can cause stomach paralysis by looking at clinical studies, reported cases, and possible mechanisms.
Review of Clinical Studies and Research
Clinical studies are essential for understanding the side effects of any medication. Semaglutide has been extensively studied, but information about its link to stomach paralysis is still emerging. Some studies have reported that semaglutide can slow down stomach emptying. This means that food stays in the stomach longer than it should.
For example, a study published in the Journal of Clinical Endocrinology & Metabolism found that patients taking semaglutide had a slower gastric emptying rate. While this effect can help people feel full longer, aiding in weight loss, it can also lead to symptoms similar to those of gastroparesis in some individuals.
Analysis of Reported Cases
In addition to clinical studies, there are individual case reports where patients taking semaglutide experienced symptoms of stomach paralysis. These symptoms can include nausea, vomiting, feeling full after eating only a small amount of food, and abdominal pain.
For instance, one case reported in a medical journal described a patient who developed severe gastroparesis symptoms after starting semaglutide. The patient experienced significant nausea and vomiting, which improved after discontinuing the medication. Such cases highlight the need for healthcare providers to monitor patients closely for signs of stomach paralysis.
Possible Mechanisms Linking Semaglutide to Stomach Paralysis
Understanding how semaglutide might cause stomach paralysis involves looking at its mechanism of action. Semaglutide works by mimicking a hormone called GLP-1 (glucagon-like peptide-1). This hormone helps regulate blood sugar levels by stimulating insulin secretion and slowing down gastric emptying.
The slowing of gastric emptying is beneficial for blood sugar control and weight management, as it helps prevent spikes in blood sugar levels after meals and keeps people feeling full longer. However, in some people, this effect can be too strong, leading to symptoms of gastroparesis.
GLP-1 receptors are found in the stomach, and when these receptors are activated by semaglutide, they can reduce the movement of the stomach muscles. This reduction in movement slows the passage of food through the stomach, which can cause the symptoms of stomach paralysis.
Identifying Symptoms of Stomach Paralysis
It’s important to recognize the symptoms of stomach paralysis, especially if you are taking semaglutide. Common symptoms include:
- Nausea: Feeling like you are going to vomit
- Vomiting: Actually throwing up, especially undigested food
- Bloating: Feeling full and swollen in the abdomen
- Early satiety: Feeling full after eating only a small amount of food
- Abdominal pain: Pain or discomfort in the stomach area
These symptoms can vary in severity and may come and go. If you experience any of these symptoms while taking semaglutide, it’s crucial to talk to your healthcare provider.
Differentiating Symptoms from Other Side Effects
Not all digestive symptoms mean you have stomach paralysis. Semaglutide can cause other side effects, such as mild nausea and diarrhea, which are common when starting the medication. These symptoms often improve over time as your body adjusts to the medication.
However, if your symptoms are severe or persist for a long time, they could indicate a more serious problem like stomach paralysis. Keeping a symptom diary can help you and your healthcare provider determine whether your symptoms are due to normal side effects or something more serious.
While there is evidence that semaglutide can slow down gastric emptying and potentially lead to symptoms of stomach paralysis, more research is needed to fully understand this relationship. If you are taking semaglutide and experience severe or persistent digestive symptoms, it’s essential to seek medical advice to ensure proper management and care.
Symptoms of Stomach Paralysis Associated with Semaglutide
Stomach paralysis, also known as gastroparesis, can be a concerning side effect for people taking semaglutide. Understanding the symptoms is crucial for early detection and management. In this section, we will explore the common symptoms of stomach paralysis, their severity and duration, and how to differentiate these symptoms from other side effects.
Common Symptoms to Watch For
- Nausea and Vomiting:
- Nausea is a feeling of sickness with an urge to vomit. Vomiting is the act of throwing up food and liquids from the stomach.
- People with stomach paralysis often feel nauseated because the stomach cannot move food through the digestive tract efficiently. This leads to a feeling of fullness and discomfort.
- Vomiting occurs when food remains in the stomach for too long, causing a build-up of pressure that eventually forces the contents back up through the esophagus.
- Bloating and Abdominal Pain:
- Bloating is a feeling of fullness or swelling in the abdomen. This can be uncomfortable and make the abdomen appear larger.
- Abdominal pain can range from mild to severe and is usually felt in the upper part of the stomach.
- These symptoms occur because the stomach is not emptying properly, causing food and gas to accumulate.
- Feeling Full Quickly:
- This symptom, also known as early satiety, is when a person feels full after eating only a small amount of food.
- It happens because the stomach’s inability to move food along means that even small meals can make you feel overly full.
- Weight Loss and Malnutrition:
- Because eating can be difficult and uncomfortable, people with stomach paralysis may eat less, leading to weight loss.
- If the body is not getting enough nutrients from food, it can lead to malnutrition, which can cause further health problems.
- Changes in Blood Sugar Levels:
- For people with diabetes, stomach paralysis can make it harder to manage blood sugar levels.
- When food stays in the stomach for a long time, it can lead to unpredictable spikes and drops in blood sugar levels.
Severity and Duration of Symptoms
The severity and duration of symptoms can vary widely among individuals. Some people might experience mild symptoms that are manageable, while others might have severe symptoms that significantly impact their daily lives.
- Mild Symptoms: These might include occasional nausea, slight bloating, or feeling full quickly. These symptoms can often be managed with dietary changes and over-the-counter medications.
- Moderate Symptoms: These might include frequent nausea and vomiting, persistent bloating, and regular abdominal pain. These symptoms may require prescription medications and more significant lifestyle changes.
- Severe Symptoms: These might include constant nausea and vomiting, severe abdominal pain, significant weight loss, and malnutrition. These symptoms often require intensive medical treatment and possibly hospitalization.
The duration of symptoms can also vary. Some people might experience symptoms only occasionally, while others might have chronic symptoms that persist over time.
Differentiating Symptoms from Other Side Effects
It’s important to distinguish symptoms of stomach paralysis from other common side effects of semaglutide. Semaglutide can cause a range of side effects, including gastrointestinal issues, but not all of these are related to stomach paralysis.
- Common Side Effects of Semaglutide:
- Nausea, vomiting, diarrhea, and constipation are common side effects of semaglutide. While these symptoms can overlap with those of stomach paralysis, they are usually temporary and less severe.
- Headache and fatigue are also common side effects but are not related to stomach paralysis.
To determine if symptoms are due to stomach paralysis, consider the following:
- Frequency and Persistence: Symptoms of stomach paralysis tend to be more persistent and frequent than common side effects.
- Response to Treatment: If common gastrointestinal treatments do not alleviate the symptoms, it might indicate stomach paralysis.
- Consulting a Doctor: Always consult with a healthcare provider to accurately diagnose and differentiate between side effects.
Recognizing the symptoms of stomach paralysis is essential for managing this condition effectively. By understanding the common symptoms, their severity and duration, and how to differentiate them from other side effects, individuals taking semaglutide can seek timely medical advice and treatment.

Risk Factors for Developing Stomach Paralysis on Semaglutide
Stomach paralysis, also known as gastroparesis, can be a serious condition. When someone takes semaglutide, certain factors might increase their risk of developing this condition. In this section, we will explore these risk factors in detail. Understanding these can help patients and healthcare providers make informed decisions about semaglutide use.
Pre-existing Conditions
Certain health conditions can make a person more likely to develop stomach paralysis when using semaglutide. These conditions include:
- Diabetes: People with diabetes are already at a higher risk for gastroparesis. Semaglutide is often prescribed to manage diabetes, so it is important to monitor for signs of stomach paralysis in diabetic patients.
- Neurological Disorders: Conditions like Parkinson’s disease or multiple sclerosis can affect the nerves that control stomach muscles, increasing the risk of gastroparesis.
- Previous Gastrointestinal Surgery: Surgeries on the stomach or intestines can disrupt normal motility, making it more likely for a person to develop gastroparesis.
If you have any of these conditions, it is crucial to discuss the potential risks with your healthcare provider before starting semaglutide.
Dosage and Duration of Treatment
The dosage of semaglutide and how long a person takes it can also influence the risk of developing stomach paralysis.
- High Dosages: Higher doses of semaglutide might have a greater impact on the digestive system. If you are prescribed a high dose, your doctor may monitor you more closely for any signs of gastroparesis.
- Long-Term Use: The longer you take semaglutide, the greater the chance of experiencing side effects, including stomach paralysis. Long-term users should have regular check-ups to ensure their digestive system is functioning properly.
Lifestyle and Dietary Factors
Certain lifestyle and dietary habits can also increase the risk of developing stomach paralysis while using semaglutide. These include:
- Poor Diet: A diet high in fatty and fiber-rich foods can slow down stomach emptying. When combined with semaglutide, this can exacerbate the risk of gastroparesis.
- Lack of Exercise: Regular physical activity helps keep the digestive system moving. Sedentary lifestyles can contribute to slower digestion, increasing the risk of stomach paralysis.
- Dehydration: Not drinking enough water can slow down the digestive process, leading to symptoms of gastroparesis.
Recognizing the Risk
Knowing the risk factors is the first step in preventing stomach paralysis. If you fall into any of these categories, it is important to be vigilant about monitoring your health while on semaglutide. Here are some steps you can take:
- Communicate with Your Doctor: Always inform your healthcare provider about any pre-existing conditions or concerns. Regular communication can help manage and mitigate risks.
- Regular Monitoring: Schedule regular check-ups with your doctor to monitor your digestive health. This is especially important if you have diabetes or other risk factors for gastroparesis.
- Healthy Lifestyle Choices: Adopt a healthy diet and regular exercise routine. This can help keep your digestive system functioning well and reduce the risk of stomach paralysis.
Managing Risk Factors
Even if you have risk factors for stomach paralysis, there are ways to manage these risks effectively:
- Adjusting Dosage: Your doctor might adjust your semaglutide dosage based on your response and any side effects you experience. This can help minimize the risk of developing stomach paralysis.
- Symptom Awareness: Be aware of the symptoms of gastroparesis, such as nausea, vomiting, bloating, and feeling full quickly. If you experience any of these symptoms, contact your healthcare provider promptly.
- Supportive Treatments: In some cases, your doctor might recommend additional treatments or medications to help manage your symptoms and support your digestive health.
Understanding the risk factors for developing stomach paralysis while on semaglutide is essential for safe and effective treatment. By being aware of pre-existing conditions, dosage considerations, and lifestyle factors, patients and healthcare providers can work together to minimize risks. Regular monitoring and healthy lifestyle choices play a crucial role in managing these risks, ensuring that the benefits of semaglutide are maximized while minimizing potential side effects. Always communicate openly with your healthcare provider and stay informed about your health to manage your treatment effectively.
Diagnosis and Monitoring of Stomach Paralysis in Semaglutide Users
If you’re using semaglutide and start experiencing stomach problems, it’s crucial to know how doctors diagnose and monitor stomach paralysis. This condition, also known as gastroparesis, can significantly affect your health and quality of life. Understanding the diagnostic process and the importance of regular monitoring can help you manage the condition more effectively.
Diagnostic Procedures and Tests
Medical History and Physical Examination
The first step in diagnosing stomach paralysis is a thorough medical history and physical examination. Your doctor will ask about your symptoms, including how long you’ve had them and their severity. They will also inquire about your diet, medications, and any other health conditions. During the physical examination, your doctor will check for signs of bloating, tenderness, and other abdominal issues.
Gastric Emptying Study
One of the most common tests for diagnosing gastroparesis is the gastric emptying study. This test measures how quickly food leaves your stomach. You will eat a meal that contains a small amount of radioactive material. A scanner will then track the movement of this material through your stomach and intestines. If food stays in your stomach longer than normal, it could indicate stomach paralysis.
Upper Endoscopy
An upper endoscopy is another essential test. During this procedure, a thin, flexible tube with a camera (endoscope) is inserted through your mouth and down into your stomach. This allows your doctor to visually inspect your stomach lining and check for any blockages or abnormalities. This test can help rule out other conditions that might cause similar symptoms.
Breath Tests
Breath tests can also be used to diagnose stomach paralysis. In these tests, you will drink a liquid containing a specific substance. Your breath is then analyzed at regular intervals to measure how quickly your stomach empties. This test is less invasive than an endoscopy and can provide valuable information about stomach function.
Regular Monitoring and Follow-Up
Importance of Regular Monitoring
Once diagnosed with stomach paralysis, regular monitoring is essential. Gastroparesis is a chronic condition, meaning it can persist for a long time and require ongoing management. Regular check-ups with your healthcare provider can help track the progression of the condition and adjust treatment plans as needed.
Symptom Tracking
Keeping a detailed symptom diary can be very helpful. Record when symptoms occur, their severity, and any potential triggers. This information can help your doctor understand how the condition is affecting you and identify any patterns that might be addressed through treatment adjustments.
Dietary and Lifestyle Monitoring
Your diet and lifestyle play a significant role in managing stomach paralysis. Regularly reviewing your eating habits with a dietitian or nutritionist can ensure you’re getting the necessary nutrients without exacerbating symptoms. Lifestyle changes, such as eating smaller, more frequent meals and avoiding high-fat and high-fiber foods, can also be beneficial.
Medication and Treatment Adjustments
Your doctor may need to adjust your medications over time. Some medications used to treat other conditions can slow stomach emptying and worsen gastroparesis symptoms. Regular follow-ups allow your doctor to review all your medications and make necessary changes to avoid complications.
Importance of Early Detection
Preventing Complications
Early detection and treatment of stomach paralysis can prevent complications. If left untreated, gastroparesis can lead to severe dehydration, malnutrition, and difficulties in managing blood sugar levels. Regular monitoring helps catch these issues early, making them easier to address.
Improving Quality of Life
By diagnosing and managing stomach paralysis early, you can significantly improve your quality of life. Effective treatment can reduce symptoms like nausea, vomiting, and bloating, allowing you to maintain a more normal lifestyle. Regular doctor visits and proactive symptom management are key to living well with this condition.
Diagnosing and monitoring stomach paralysis in semaglutide users involves several steps, including taking a medical history, conducting tests like gastric emptying studies and upper endoscopies, and maintaining regular follow-ups. Keeping track of symptoms, adjusting diet and medications, and early detection are crucial in managing the condition effectively. By working closely with your healthcare provider, you can manage stomach paralysis and improve your overall well-being.
Managing Stomach Paralysis While on Semaglutide
Stomach paralysis, also known as gastroparesis, can be a challenging condition to manage, especially when it is caused or worsened by medications like semaglutide. However, there are several ways to manage this condition effectively. This section will cover dietary modifications, medications and treatment options, and lifestyle changes to help alleviate symptoms.
Dietary Modifications
Dietary changes are one of the first steps in managing stomach paralysis. Since gastroparesis affects how quickly food leaves the stomach, eating the right kinds of food can make a big difference.
- Eat Smaller, More Frequent Meals: Instead of three large meals a day, try eating smaller meals more often. This can help reduce the amount of food your stomach has to process at one time, making it easier for your stomach to empty.
- Chew Food Thoroughly: Make sure to chew your food well. Smaller food particles are easier for your stomach to digest and pass through.
- Choose Easy-to-Digest Foods: Foods that are low in fat and fiber are generally easier to digest. Fat slows down stomach emptying, and high-fiber foods can be hard for your stomach to process.
- Blend or Puree Foods: If solid foods are difficult to digest, try blending or pureeing them. Soups, smoothies, and well-cooked vegetables are good options.
- Stay Hydrated: Drink plenty of fluids, but try to avoid drinking a lot of liquids during meals. Instead, drink fluids between meals to help stay hydrated without making your stomach feel too full.
Medications and Treatment Options
In addition to dietary changes, there are medications and treatments that can help manage stomach paralysis.
- Prokinetic Agents: These medications help stimulate the muscles of the stomach to improve motility. Examples include metoclopramide and erythromycin. However, these medications should be used under the guidance of a healthcare provider due to potential side effects.
- Antiemetic Medications: These drugs can help control nausea and vomiting, which are common symptoms of gastroparesis. Medications like ondansetron or promethazine can be prescribed to alleviate these symptoms.
- Pain Management: Sometimes, stomach paralysis can cause abdominal pain. Pain management options may include medications like acetaminophen or, in some cases, medications specifically designed for neuropathic pain.
- Gastric Electrical Stimulation: In severe cases of gastroparesis, a device called a gastric stimulator may be surgically implanted. This device sends mild electrical pulses to the stomach muscles to help improve stomach emptying.
- Nutritional Supplements: If dietary modifications alone are not sufficient to meet nutritional needs, nutritional supplements in liquid form can be helpful. Your healthcare provider can recommend appropriate supplements.
Lifestyle Changes to Alleviate Symptoms
Beyond diet and medications, certain lifestyle changes can also help manage symptoms of stomach paralysis.
- Exercise Regularly: Light to moderate exercise, such as walking, can help stimulate digestion and promote overall health. Try to take a walk after meals to help your stomach empty more effectively.
- Elevate the Head While Sleeping: Raising the head of your bed or using extra pillows to elevate your head while sleeping can help prevent stomach contents from backing up into the esophagus, which can be particularly helpful for those experiencing reflux symptoms.
- Avoid Lying Down After Meals: Try to stay upright for at least two to three hours after eating. This can help gravity assist in moving food through the digestive tract.
- Manage Stress: Stress can worsen the symptoms of gastroparesis. Techniques such as deep breathing exercises, meditation, or yoga can help reduce stress levels.
- Monitor Blood Sugar Levels: For people with diabetes, keeping blood sugar levels well-controlled is important, as high blood sugar can worsen gastroparesis. Work with your healthcare provider to manage your diabetes effectively.
Consulting with Healthcare Providers
Managing stomach paralysis while on semaglutide requires a comprehensive approach that includes dietary modifications, medications, and lifestyle changes. It is crucial to work closely with healthcare providers to develop a personalized management plan. Regular follow-ups and open communication with your healthcare team will help ensure that your condition is managed effectively and that any necessary adjustments to your treatment plan are made promptly.

Preventive Measures for Stomach Paralysis with Semaglutide Use
Preventing stomach paralysis, or gastroparesis, while using semaglutide is important for your overall health and well-being. Here are some detailed preventive measures to help you use semaglutide safely and effectively.
Guidelines for Safe Usage
Start with a Low Dose: When beginning semaglutide, it’s often best to start with a low dose. This allows your body to adjust to the medication gradually. Your doctor will usually start you on a lower dose and then slowly increase it. This can help minimize side effects, including potential impacts on your stomach.
Follow Your Doctor’s Instructions: Always take semaglutide exactly as prescribed by your doctor. Do not adjust your dose without consulting your healthcare provider. Skipping doses or taking more than prescribed can increase the risk of side effects.
Report Symptoms Early: If you experience any symptoms of stomach paralysis, such as nausea, vomiting, or feeling full quickly, report them to your doctor right away. Early detection can help manage symptoms more effectively and prevent complications.
Patient Education and Awareness
Understand the Medication: Educate yourself about semaglutide and how it works. Knowing the potential side effects, including stomach paralysis, can help you recognize symptoms early and seek help when needed. Ask your healthcare provider to explain anything you don’t understand about your treatment.
Know the Symptoms of Gastroparesis: Familiarize yourself with the symptoms of stomach paralysis. Common symptoms include nausea, vomiting, bloating, and feeling full quickly after starting a meal. Being aware of these symptoms can help you detect issues early.
Stay Informed: Keep up with the latest information about semaglutide and its effects. New research and guidelines can provide valuable insights into how to use the medication safely. Your healthcare provider can be a good source of updated information.
Regular Check-Ups and Symptom Monitoring
Schedule Regular Visits: Make sure to have regular check-ups with your healthcare provider. During these visits, your doctor can monitor your overall health and check for any signs of stomach paralysis. Regular monitoring helps catch problems early, making them easier to manage.
Track Your Symptoms: Keep a symptom diary to track any changes in your digestive health. Note when you experience symptoms like nausea, vomiting, or bloating. This record can help your doctor understand your condition better and adjust your treatment if needed.
Regular Blood Tests: Regular blood tests can help monitor your overall health and how your body is responding to semaglutide. These tests can detect any abnormalities early, allowing for timely intervention.
Lifestyle and Dietary Adjustments
Eat Small, Frequent Meals: Eating smaller meals more frequently can help manage symptoms of stomach paralysis. Large meals can be hard for your stomach to process, leading to discomfort. Smaller, more frequent meals can ease digestion.
Choose Easy-to-Digest Foods: Focus on foods that are easy to digest, such as lean proteins, cooked vegetables, and low-fiber foods. Avoid high-fat and high-fiber foods, as they can slow down digestion and worsen symptoms.
Stay Hydrated: Drink plenty of water throughout the day. Staying hydrated can help with digestion and prevent constipation, a common issue for people with stomach paralysis. Avoid sugary and carbonated drinks, as they can cause bloating.
Avoid Lying Down After Eating: Try not to lie down immediately after eating. This can slow digestion and make symptoms worse. Instead, wait at least two hours after a meal before lying down.
Exercise Regularly: Regular physical activity can help improve digestion and overall health. Simple activities like walking after meals can aid in digestion and prevent symptoms of stomach paralysis.
Working with Your Healthcare Team
Open Communication: Maintain open communication with your healthcare team. Share any concerns or symptoms you experience, no matter how minor they may seem. Your doctor can provide valuable advice and adjust your treatment plan to better suit your needs.
Follow-Up Appointments: Attend all follow-up appointments to monitor your progress. These visits allow your doctor to make any necessary adjustments to your treatment and ensure that semaglutide is working well for you without causing severe side effects.
Specialist Consultation: If needed, ask for a referral to a gastroenterologist, a doctor who specializes in digestive health. They can provide more specialized care if you experience symptoms of stomach paralysis.
By following these preventive measures, you can reduce the risk of developing stomach paralysis while using semaglutide. Staying informed, monitoring your symptoms, and maintaining a healthy lifestyle can help you use this medication safely and effectively. Always consult your healthcare provider for personalized advice and support.
Conclusion
In summary, semaglutide is a medication that helps people manage their blood sugar levels and weight. It works by mimicking a hormone in the body that helps control appetite and blood sugar. However, like all medications, semaglutide can have side effects. One of the more serious but less common side effects is stomach paralysis, also known as gastroparesis. This condition affects how the stomach muscles work, leading to slow digestion and various uncomfortable symptoms.
Stomach paralysis can cause a range of symptoms such as nausea, vomiting, bloating, and abdominal pain. It happens when the stomach muscles do not move food through the digestive tract as they should. Instead, food stays in the stomach longer than normal, which can lead to these symptoms. While stomach paralysis is not very common, it is important for anyone taking semaglutide to be aware of this potential side effect.
Research has shown that there is a possible link between semaglutide and stomach paralysis. Some studies and reports have highlighted cases where patients on semaglutide experienced symptoms of gastroparesis. It is believed that the way semaglutide works might slow down the stomach’s movements. This can lead to the symptoms of stomach paralysis in some individuals. However, more research is needed to fully understand this link.
Certain people might be at a higher risk of developing stomach paralysis while taking semaglutide. People who already have digestive issues, diabetes, or other health conditions that affect the stomach may be more prone to experiencing this side effect. The dosage of semaglutide and how long a person has been taking it can also influence the risk. Additionally, lifestyle and dietary habits can play a role in how the body responds to the medication.
Diagnosing stomach paralysis involves several steps. If you are taking semaglutide and notice symptoms like nausea, vomiting, or bloating, it is important to talk to your doctor. They might perform tests to see how well your stomach is working. These tests can include gastric emptying studies, which measure how quickly food leaves your stomach. Early diagnosis and regular monitoring are key to managing the condition effectively.
Managing stomach paralysis while on semaglutide involves a combination of dietary changes, medications, and lifestyle adjustments. Eating smaller, more frequent meals can help ease symptoms. Avoiding high-fat and high-fiber foods, which take longer to digest, can also be beneficial. Medications that help move food through the stomach more quickly can be prescribed by a doctor. In some cases, other treatments might be necessary to help manage the symptoms and improve the quality of life.
Preventing stomach paralysis when using semaglutide is possible by following certain guidelines. It is important to use the medication as prescribed and to follow up regularly with your healthcare provider. They can monitor your progress and adjust your treatment plan if necessary. Being aware of the symptoms of stomach paralysis and seeking medical advice early can help prevent the condition from becoming severe. Patient education is crucial, as understanding the potential risks and how to manage them can lead to better outcomes.
In conclusion, while semaglutide is effective for managing blood sugar and weight, it is important to be aware of its potential side effects, including stomach paralysis. Understanding how semaglutide works, recognizing the symptoms of stomach paralysis, and knowing the risk factors can help you stay informed about your health. If you experience any symptoms, it is important to talk to your doctor right away. They can help diagnose the condition and provide the appropriate treatment. By staying informed and proactive, you can manage your health effectively while using semaglutide. Always consult your healthcare provider for personalized advice and follow their recommendations to ensure safe and effective treatment.
Research Citations
Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2016 Nov 10;375(19):1834-1844. doi: 10.1056/NEJMoa1607141. PMID: 27633186.
Aroda VR, Bain SC, Cariou B, et al. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol. 2017 May;5(5):355-366. doi: 10.1016/S2213-8587(17)30092-4. Epub 2017 Mar 1. PMID: 28259609.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2016 Jul 28;375(4):311-22. doi: 10.1056/NEJMoa1603827. Epub 2016 Jun 13. PMID: 27295427.
Trujillo JM, Nuffer W, Ellis SL. GLP-1 receptor agonists: a review of head-to-head clinical studies. Ther Adv Endocrinol Metab. 2015 Aug;6(4):19-28. doi: 10.1177/2042018815595641. PMID: 26288724; PMCID: PMC4539847.
Pozzilli P, Norwood P, Jódar E, et al. Placebo-controlled, randomized trial of the addition of once-weekly glucagon-like peptide-1 receptor agonist dulaglutide to titrated daily insulin glargine in patients with type 2 diabetes (AWARD-9). Diabetes Obes Metab. 2017 Mar;19(3):1024-1031. doi: 10.1111/dom.12894. Epub 2017 Jan 4. PMID: 27981616; PMCID: PMC5341920.
Marso SP, Poulter NR, Nissen SE, et al. Design of the liraglutide effect and action in diabetes: evaluation of cardiovascular outcome results (LEADER) trial. Am Heart J. 2013 Nov;166(5):823-30.e5. doi: 10.1016/j.ahj.2013.07.012. Epub 2013 Sep 1. PMID: 24176460.
Sorli C, Harashima SI, Tsoukas GM, et al. Efficacy and Safety of Once-Weekly Semaglutide Monotherapy Versus Placebo in Patients with Type 2 Diabetes (SUSTAIN 1): A Double-Blind, Randomised, Placebo-Controlled, Parallel-Group, Multinational, Multicentre Phase 3a Trial. Lancet Diabetes Endocrinol. 2017 Feb;5(4):251-260. doi: 10.1016/S2213-8587(17)30035-3. Epub 2017 Jan 10. PMID: 28082169.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2016 Nov 10;375(19):1834-1844. doi: 10.1056/NEJMoa1607141. PMID: 27633186.
Pratley RE, Aroda VR, Lingvay I, et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 2018 Jan;6(4):275-286. doi: 10.1016/S2213-8587(18)30024-X. Epub 2018 Feb 6. PMID: 29426642.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2016 Nov 10;375(19):1834-1844. doi: 10.1056/NEJMoa1607141. PMID: 27633186.
Questions and Answers: Semaglutide Stomach Paralysis
Semaglutide is a medication used to treat type 2 diabetes and obesity. It works by mimicking a hormone called GLP-1, which helps regulate blood sugar levels and appetite.
Stomach paralysis, also known as gastroparesis, is a condition where the stomach muscles do not function properly, causing delayed stomach emptying. This can lead to symptoms like nausea, vomiting, bloating, and feeling full quickly.
Semaglutide may slow gastric emptying as part of its mechanism of action, which could potentially lead to symptoms similar to gastroparesis in some individuals. However, true gastroparesis is a rare side effect.
Semaglutide slows gastric emptying by enhancing the effects of the hormone GLP-1, which reduces the rate at which food leaves the stomach, helping to control blood sugar levels and promote satiety.
Symptoms may include nausea, vomiting, bloating, abdominal pain, and feeling full quickly after eating small amounts of food.
The risk of developing gastroparesis with semaglutide is relatively low. Most patients do not experience significant issues with gastric emptying, but some may have mild symptoms.
If you experience symptoms of gastroparesis, contact your healthcare provider. They may adjust your dosage, recommend dietary changes, or consider alternative treatments.
Preventive measures include eating smaller, more frequent meals, avoiding high-fat and high-fiber foods, and staying hydrated. Your healthcare provider can provide personalized advice.
Yes, gastroparesis symptoms can be managed with dietary changes, medications to enhance gastric motility, and in some cases, adjusting or discontinuing semaglutide under medical supervision.
Do not stop taking semaglutide without consulting your healthcare provider. They will evaluate your symptoms and determine the best course of action, which may include adjusting your treatment plan.

Dr. Melissa VanSickle
Dr. Melissa Vansickle, MD is a family medicine specialist in Onsted, MI and has over 24 years of experience in the medical field. She graduated from University of Michigan Medical School in 1998. She is affiliated with medical facilities Henry Ford Allegiance Health and Promedica Charles And Virginia Hickman Hospital. Her subspecialties include General Family Medicine, Urgent Care, Complementary and Integrative Medicine in Rural Health.