Table of Contents
Introduction
Semaglutide is a medication that has gained attention for its effectiveness in treating type 2 diabetes and aiding in weight loss. As more people use semaglutide, it is crucial to understand its potential side effects, especially serious ones like blood clots. This article aims to provide a comprehensive overview of the relationship between semaglutide and blood clots, answering the most common questions people have about this topic.
Semaglutide works by mimicking a hormone in the body called GLP-1, which helps to control blood sugar levels and reduce appetite. It is often prescribed to people with type 2 diabetes to help manage their blood sugar levels, and it has also been approved for weight loss in people who are overweight or obese. While semaglutide can be very effective, like all medications, it comes with potential side effects. One of the more serious side effects that has raised concerns is the risk of blood clots.
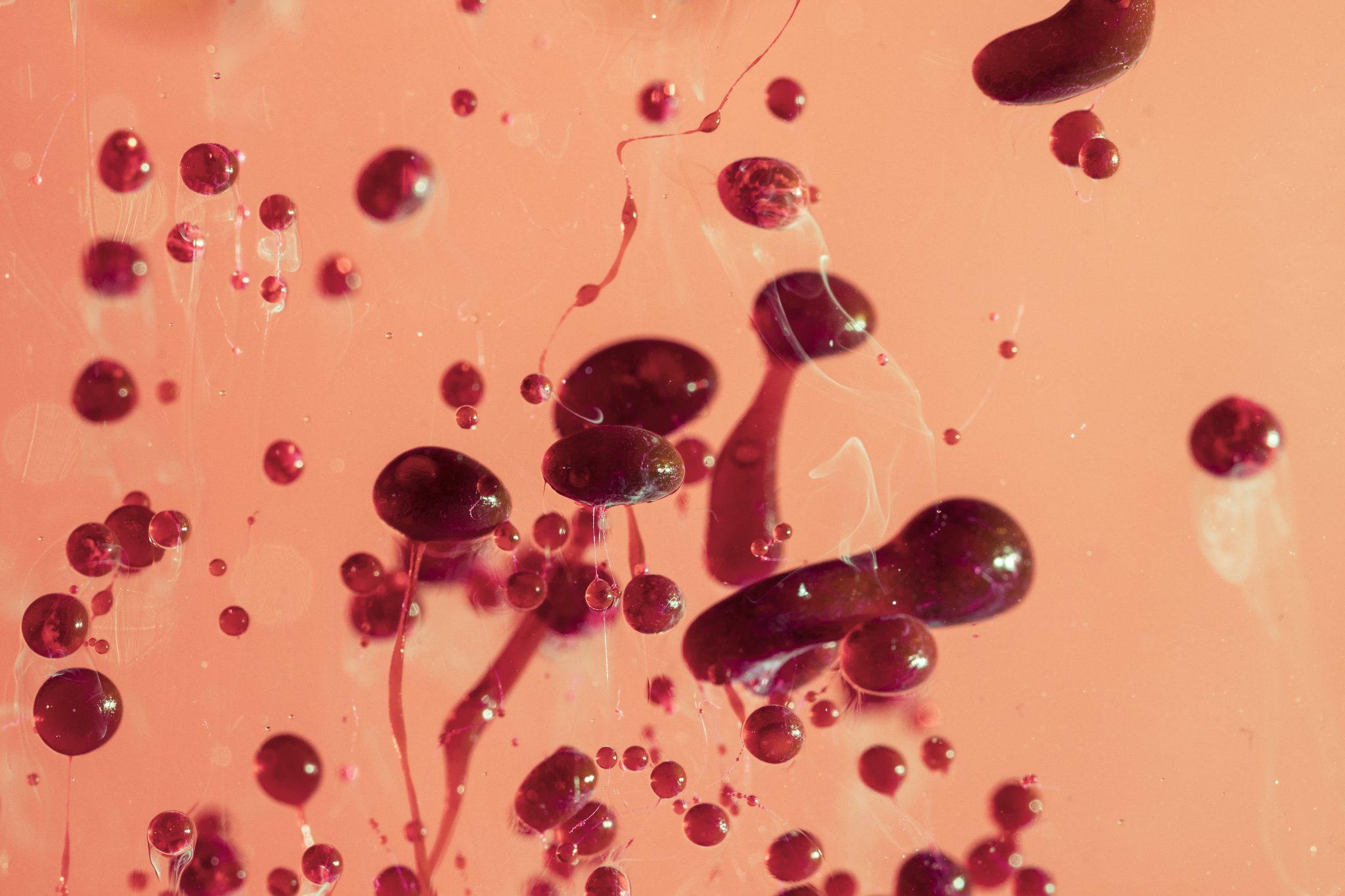
Blood clots are clumps of blood that form when blood changes from a liquid to a gel-like state. They can form in veins or arteries and can lead to serious health problems if they travel to critical areas such as the lungs (causing a pulmonary embolism) or the brain (leading to a stroke). Understanding the potential for semaglutide to cause or contribute to blood clots is important for anyone considering or currently using this medication.
The purpose of this article is to answer the top 10 questions people have about semaglutide and blood clots. By addressing these questions, we aim to provide clear and useful information that can help people make informed decisions about their health. We will explore what semaglutide is and how it works, what blood clots are and why they are dangerous, and whether there is a link between semaglutide and blood clots. We will also look at who might be at risk, how to recognize the symptoms of blood clots, and what steps can be taken to prevent them.
This article will also discuss what to do if you suspect you have a blood clot while taking semaglutide, including when to seek medical help and what treatments might be necessary. We will cover how patients and healthcare providers can work together to manage the risk of blood clots and ensure the safe use of semaglutide. Our goal is to provide detailed, understandable information to help you stay informed and healthy.
In recent years, semaglutide has been widely studied and used, leading to increased awareness of both its benefits and potential risks. While the benefits of semaglutide in managing blood sugar levels and promoting weight loss are well-documented, it is equally important to understand the potential risks, including the risk of blood clots. Blood clots can be life-threatening, and being aware of this risk can help users of semaglutide take necessary precautions.
The information provided in this article is based on current research and expert recommendations. It is intended to help you understand the potential side effects of semaglutide and what steps you can take to reduce your risk of blood clots. Always consult with your healthcare provider before making any changes to your medication or treatment plan. They can provide personalized advice based on your specific health needs and risks.
In conclusion, understanding the relationship between semaglutide and blood clots is crucial for anyone using or considering this medication. This article will answer the most common questions about this topic, providing you with the information you need to stay safe and make informed decisions about your health. Stay tuned as we dive deeper into each aspect of semaglutide and blood clots, starting with what semaglutide is and how it works.
What is Semaglutide?
Semaglutide is a type of medication known as a GLP-1 receptor agonist. GLP-1 stands for glucagon-like peptide-1. This is a hormone that your body naturally produces in the gut. When you eat, GLP-1 helps regulate your blood sugar levels by stimulating insulin release and inhibiting glucagon secretion. Insulin lowers blood sugar levels, while glucagon raises them. By balancing these hormones, semaglutide helps keep your blood sugar levels in check.
How Does Semaglutide Work?
Semaglutide mimics the action of natural GLP-1 in your body. When you take semaglutide, it binds to GLP-1 receptors in your pancreas. This triggers your pancreas to release more insulin when your blood sugar levels are high. At the same time, semaglutide reduces the amount of glucagon your liver releases. This dual action helps lower your blood sugar levels effectively.
But semaglutide does more than just control blood sugar. It also slows down the emptying of your stomach. This means food stays in your stomach longer, making you feel full for a longer time. This can help reduce your appetite and lead to weight loss.
Common Uses of Semaglutide
Semaglutide is primarily used to treat type 2 diabetes. In type 2 diabetes, your body either doesn’t produce enough insulin or your cells don’t respond well to insulin. This leads to high blood sugar levels, which can cause various health problems over time. By helping control blood sugar levels, semaglutide can reduce the risk of complications from diabetes, such as heart disease, kidney damage, and nerve damage.
In addition to treating diabetes, semaglutide is also approved for weight management in people with obesity or overweight who have at least one weight-related condition, such as high blood pressure or high cholesterol. Clinical studies have shown that semaglutide can help people lose significant amounts of weight when combined with a reduced-calorie diet and increased physical activity.
Forms of Semaglutide
Semaglutide is available in two main forms: an injection and an oral tablet. The injectable form is usually taken once a week. It comes in a pre-filled pen, making it easy to use. You inject it under the skin, usually in the abdomen, thigh, or upper arm. The oral tablet is taken once daily, with or without food.
Benefits of Semaglutide
One of the major benefits of semaglutide is its ability to effectively control blood sugar levels. For many people with type 2 diabetes, maintaining stable blood sugar levels can be challenging. Semaglutide helps by providing consistent glucose control, reducing the risk of both high and low blood sugar episodes.
Another benefit is weight loss. For individuals with type 2 diabetes who are overweight, losing weight can improve insulin sensitivity and overall health. Semaglutide supports weight loss by reducing appetite and increasing feelings of fullness.
Possible Side Effects
Like all medications, semaglutide can cause side effects. The most common side effects include nausea, vomiting, diarrhea, and constipation. These symptoms are usually mild and tend to decrease over time as your body adjusts to the medication. Some people may also experience abdominal pain or decreased appetite.
More serious side effects are rare but can occur. These include pancreatitis (inflammation of the pancreas), kidney problems, and allergic reactions. It’s important to talk to your doctor about any side effects you experience while taking semaglutide.
Semaglutide is a powerful medication that offers significant benefits for people with type 2 diabetes and those struggling with obesity. By understanding how it works and its potential effects, you can better manage your health and make informed decisions about your treatment options. Always consult with your healthcare provider before starting any new medication to ensure it’s the right choice for you.
What are Blood Clots?
Blood clots are clumps of blood that have changed from a liquid to a semi-solid state. This process is known as coagulation and is a normal part of the body’s healing mechanism. When we get injured, blood clots help stop bleeding. However, blood clots that form in the veins or arteries without injury can be dangerous.
Types of Blood Clots
There are two main types of blood clots: deep vein thrombosis (DVT) and pulmonary embolism (PE).
Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, usually in the legs. The deep veins are large veins that go through muscles and carry blood back to the heart. Symptoms of DVT can include swelling, pain, and redness in the leg. Sometimes, the skin may feel warm to the touch. If a piece of the clot breaks off, it can travel through the bloodstream to other parts of the body.
Pulmonary Embolism (PE)
PE happens when a blood clot travels to the lungs and blocks a blood vessel. This can be life-threatening because it can stop blood from reaching parts of the lung. Symptoms of PE include sudden shortness of breath, chest pain (especially when breathing deeply), and coughing up blood. Other symptoms can include a rapid heart rate and feeling lightheaded or faint. PE is often caused by a clot that starts as a DVT.
Common Causes and Risk Factors
Blood clots can form for many reasons. Understanding the common causes and risk factors can help you be aware of your own risk.
Inactivity and Immobility
Long periods of inactivity, such as sitting during long flights or car trips, can slow blood flow in the veins. This makes it easier for clots to form. Being bedridden or recovering from surgery also increases the risk of blood clots.
Injury and Surgery
Injuries that damage blood vessels can trigger the body’s clotting process. This is a natural response to prevent excessive bleeding. Surgery, especially on the hips or legs, can increase the risk of blood clots. This is why doctors often recommend moving around soon after surgery.
Medical Conditions
Certain medical conditions can increase the risk of blood clots. These include cancer, heart disease, and inflammatory conditions like lupus. Blood clotting disorders, such as Factor V Leiden mutation, can make a person more prone to clots.
Medications
Some medications can raise the risk of blood clots. These include hormone replacement therapy, birth control pills, and some cancer treatments. It’s important to talk to your doctor about any medications you are taking and their potential risks.
Lifestyle Factors
Smoking, being overweight, and not getting enough exercise can all contribute to the risk of blood clots. Staying hydrated and maintaining a healthy lifestyle can help reduce these risks.
Symptoms and Complications of Blood Clots
Recognizing the symptoms of blood clots is crucial for getting timely medical help.
Symptoms of DVT
- Swelling in one or both legs
- Pain or tenderness in the leg, which might feel like cramping or soreness
- Red or discolored skin on the leg
- A feeling of warmth in the affected leg
Symptoms of PE
- Sudden shortness of breath
- Chest pain that may become worse when you breathe deeply
- Coughing up blood
- Rapid heartbeat or palpitations
- Lightheadedness or dizziness
Complications
Blood clots can lead to serious complications if not treated. For instance, a PE can be fatal if it severely restricts blood flow to the lungs. Post-thrombotic syndrome can occur after a DVT. This condition causes long-term pain and swelling in the affected limb. Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare but serious condition that can develop after a PE, leading to high blood pressure in the lungs.
Understanding blood clots, their causes, and symptoms is essential for anyone using medications like semaglutide. Being aware of your own risk factors and taking steps to reduce them can help maintain your health and safety. If you suspect you have a blood clot, seek medical attention immediately.
Can Semaglutide Cause Blood Clots?
Semaglutide is a medication often prescribed for managing type 2 diabetes and aiding weight loss. Like all medications, it’s essential to understand its potential side effects. One concern that some people have is whether semaglutide can cause blood clots. To answer this question, we need to look at what the current research and evidence say.
Semaglutide works by mimicking a hormone called GLP-1 (glucagon-like peptide-1). This hormone helps control blood sugar levels and influences appetite. The U.S. Food and Drug Administration (FDA) and other health organizations have approved Ozempic and Wegovy after thorough testing. However, new research always emerges, and it’s crucial to stay updated on potential risks.
According to clinical trials and studies, there isn’t strong evidence directly linking semaglutide to an increased risk of blood clots. These trials involve many participants and are designed to detect various side effects. While some people in these trials did develop blood clots, the number was not significantly higher than what is usually expected in the general population. This means that while blood clots did occur, they were not necessarily caused by semaglutide.
Discussion of Reported Cases and Studies
There have been a few reported cases where individuals taking semaglutide developed blood clots. However, it’s important to understand that these cases do not prove that semaglutide was the cause. Many factors can contribute to blood clots, such as underlying health conditions, lifestyle choices, and other medications.
One study published in a medical journal looked at people with type 2 diabetes taking semaglutide and compared them to those not taking the medication. The study found no significant difference in the rate of blood clots between the two groups. This suggests that semaglutide does not notably increase the risk of blood clots compared to not taking it.
Comparison with Other Medications in the Same Class
Semaglutide belongs to a class of drugs known as GLP-1 receptor agonists. Other medications in this class include exenatide and liraglutide. Comparing semaglutide to these drugs can help us understand its safety profile better.
Studies have shown that GLP-1 receptor agonists, in general, do not have a high risk of causing blood clots. For example, liraglutide, another widely used GLP-1 receptor agonist, has been studied extensively, and the evidence does not suggest a significant risk of blood clots.
In a large analysis combining data from several studies, researchers examined the safety of different GLP-1 receptor agonists. They found no substantial increase in the risk of blood clots for people taking these medications compared to those not taking them. This analysis included semaglutide, further supporting the idea that it is unlikely to cause blood clots.
Monitoring and Ongoing Research
While current evidence does not show a strong link between semaglutide and blood clots, ongoing research is essential. The medical community continues to monitor and study the long-term effects of semaglutide and other GLP-1 receptor agonists. This continuous research helps ensure that any potential risks are identified and managed appropriately.
Patients taking semaglutide should report any unusual symptoms to their healthcare provider. Symptoms of blood clots can include swelling, pain, redness in a limb, shortness of breath, and chest pain. Early detection and treatment are crucial in managing blood clots effectively.
While there have been some reports of blood clots in people taking semaglutide, current research and evidence do not indicate a direct link. The risk of blood clots does not appear to be significantly higher than in the general population or compared to other medications in the same class. Ongoing research and monitoring are important to ensure the safety of all patients using semaglutide. If you have concerns about blood clots or any other side effects, discussing them with your healthcare provider is always a good idea.
How Does Semaglutide Affect Blood Clot Risk?
Understanding how semaglutide might affect the risk of blood clots is important for anyone considering or currently using this medication. Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist used to manage diabetes and, more recently, for weight loss. Like any medication, it’s essential to understand its potential side effects, including the risk of blood clots.
Mechanism of Action
To understand how semaglutide could affect blood clot risk, we first need to understand how it works. Semaglutide mimics a natural hormone in the body called GLP-1. This hormone helps regulate blood sugar levels by increasing insulin production and decreasing the amount of sugar the liver releases into the bloodstream. Semaglutide also slows down how quickly food leaves the stomach, which helps you feel full longer and can aid in weight loss.
Potential Influence on Clotting Mechanisms
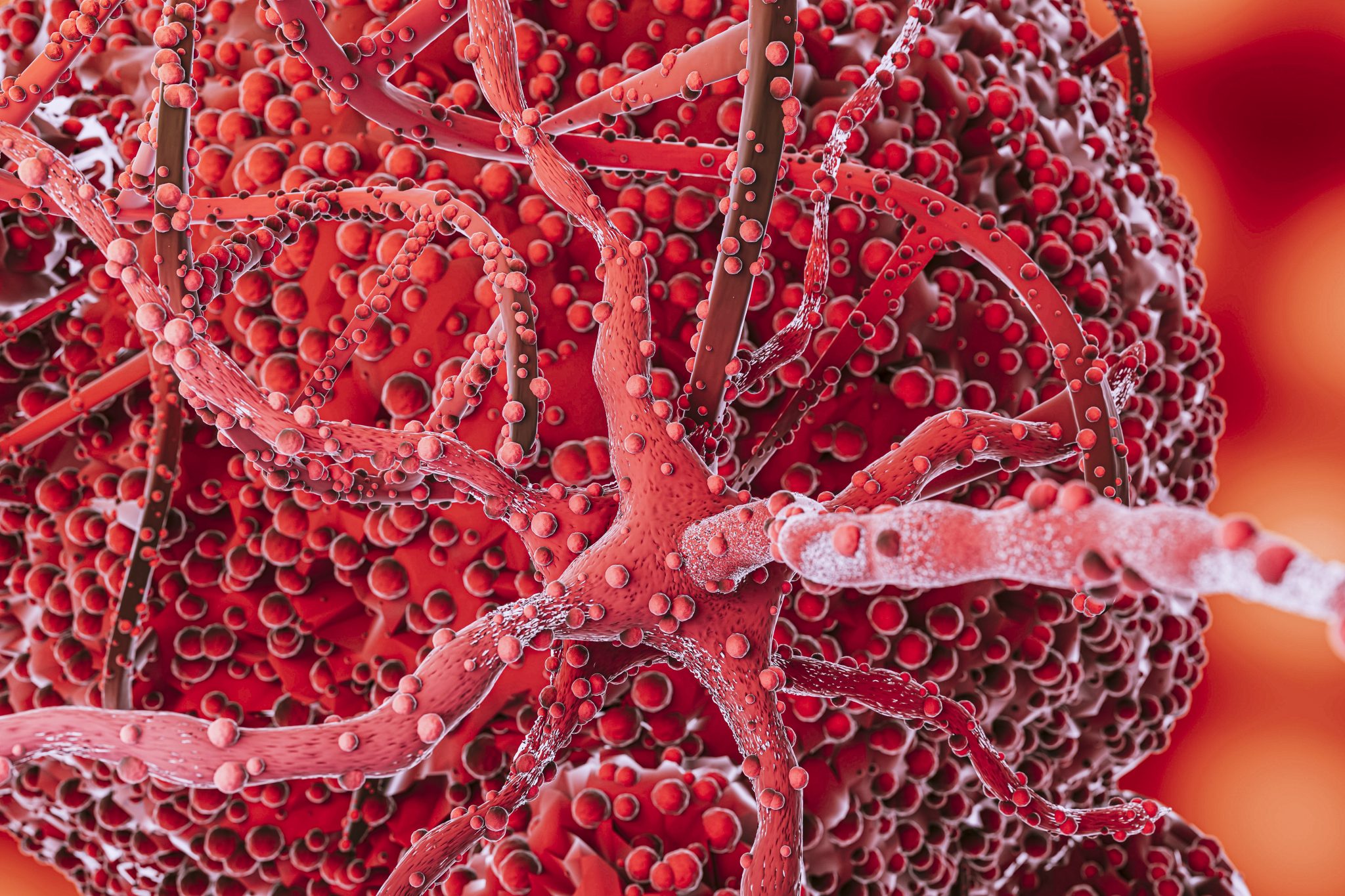
The primary concern with semaglutide and blood clots is how it might interact with the body’s natural clotting mechanisms. Blood clots form when blood cells called platelets and proteins in your blood stick together to stop bleeding. While this process is crucial for healing cuts and injuries, sometimes clots can form inside blood vessels, leading to serious health issues like deep vein thrombosis (DVT) or pulmonary embolism (PE).
Some studies suggest that medications affecting blood sugar and weight might also impact clotting factors. However, it’s important to note that the exact mechanisms through which semaglutide could influence clotting are not fully understood. Current research has not conclusively shown that semaglutide directly increases the risk of blood clots, but ongoing studies continue to explore this possibility.
Correlation vs. Causation
One of the biggest challenges in understanding the relationship between semaglutide and blood clots is distinguishing correlation from causation. Just because two things happen together doesn’t mean one causes the other. For example, people with diabetes or obesity, who are often prescribed semaglutide, already have a higher risk of blood clots. This makes it difficult to determine if semaglutide itself increases clot risk or if the higher risk is due to the underlying health conditions.
Research and Evidence
So far, research on semaglutide and blood clot risk is limited but growing. A few clinical trials have reported cases of blood clots in patients taking semaglutide, but these cases are relatively rare. For instance, a large clinical trial called the SUSTAIN-6 trial, which investigated the cardiovascular effects of semaglutide, found no significant increase in the risk of blood clots compared to other diabetes treatments. This suggests that while blood clots are a potential side effect, they are not common.
Biological Pathways
Understanding the biological pathways through which semaglutide could affect blood clot risk requires more research. Some scientists hypothesize that by reducing inflammation and improving blood vessel function, semaglutide might actually lower the risk of clots. On the other hand, because semaglutide can affect the balance of certain hormones and proteins in the blood, it could theoretically influence clot formation in ways not yet fully understood.
Monitoring and Ongoing Studies
Given the complexity of blood clot formation and the relatively new use of semaglutide, healthcare providers are encouraged to monitor patients closely for signs of clotting. Ongoing studies are also essential to provide more definitive answers. These studies aim to better understand the long-term effects of semaglutide on blood clot risk and identify any specific patient populations who might be at higher risk.
While there is no strong evidence to suggest that semaglutide significantly increases the risk of blood clots, understanding its potential effects on clotting mechanisms is crucial. Patients should discuss any concerns with their healthcare provider and stay informed about new research findings. By doing so, they can make the best decisions for their health and safety while using semaglutide.
Who is at Risk for Blood Clots While Using Semaglutide?
When taking semaglutide, it’s essential to understand who might be at higher risk for developing blood clots. While the medication has proven benefits for managing diabetes and aiding weight loss, it’s crucial to be aware of the potential risks, including the formation of blood clots. This section will delve into identifying high-risk groups, factors that may increase the risk, and recommendations for risk assessment before starting semaglutide.
Identifying High-Risk Groups
Certain individuals are more likely to develop blood clots when using semaglutide. Understanding who these high-risk groups are can help in taking preventive measures. Here are some key categories:
- Individuals with a History of Blood Clots: If you’ve had blood clots before, you are more likely to develop them again. This history increases the risk when taking medications that can potentially affect blood clotting, like semaglutide.
- People with Clotting Disorders: Some people have inherited or acquired conditions that make their blood clot more easily. Conditions such as Factor V Leiden, prothrombin gene mutation, and antiphospholipid syndrome are examples of clotting disorders that can increase the risk.
- Those with Certain Chronic Illnesses: Chronic diseases such as cancer, heart disease, and inflammatory bowel disease (like Crohn’s disease or ulcerative colitis) can increase the risk of blood clots. These conditions can cause changes in the blood that make clots more likely.
- Patients Who are Immobile for Long Periods: Long periods of immobility, such as being bedridden or sitting for long periods (like on long flights), can lead to blood clots. This immobility slows down blood flow, which can cause clots to form.
Factors That May Increase Risk
Several factors can heighten the risk of blood clots for people taking semaglutide. Knowing these can help in taking proactive steps to reduce risk:
Lifestyle Factors
- Smoking: Smoking damages blood vessels and can increase the tendency for blood to clot. Quitting smoking is beneficial not just for reducing clot risk but also for overall health.
- Obesity: Excess weight can put extra pressure on veins and slow down blood flow, increasing the risk of clot formation. Weight management is crucial for reducing this risk.
Medications
- Hormone Replacement Therapy (HRT) and Birth Control Pills: These medications can increase the risk of blood clots. If you are taking these along with semaglutide, your doctor needs to be aware.
- Other Medications: Some medications, like steroids or certain cancer treatments, can also increase clotting risk. Always inform your healthcare provider about all medications you are taking.
Age and Gender
- Older Age: As people age, the risk of blood clots increases. This is due to changes in the blood and veins over time.
- Female Gender: Women, especially those who are pregnant, postpartum, or using hormone-based medications, are at a higher risk for blood clots.
Recommendations for Risk Assessment Before Starting Semaglutide
Before starting semaglutide, it’s important to assess your risk for blood clots. Here’s how you can do it:
- Consult with Your Healthcare Provider: Discuss your medical history in detail with your doctor. Make sure to mention any previous blood clots, clotting disorders, chronic illnesses, and lifestyle factors like smoking or prolonged immobility.
- Undergo Necessary Tests: Your doctor might recommend tests to assess your clotting risk. These can include blood tests to check for clotting disorders or imaging tests if there’s a concern about existing clots.
- Develop a Risk Management Plan: Based on your risk factors, your doctor can help create a plan to minimize your risk. This might include lifestyle changes, close monitoring, or even preventive medications.
- Regular Monitoring: Once you start taking semaglutide, regular check-ups are vital. These help in early detection and management of any potential issues, including blood clots.
By understanding who is at risk and taking proactive steps, you can safely benefit from semaglutide while minimizing the risk of blood clots. Always stay informed and maintain open communication with your healthcare provider to ensure the best possible outcomes.

Recognizing the Symptoms of Blood Clots
Blood clots are serious and can lead to major health problems if not treated quickly. If you are taking semaglutide, it is important to know the signs and symptoms of blood clots so you can seek help right away if needed. Here, we will discuss the common signs and symptoms to watch for, why early detection is crucial, and how you can monitor your health effectively.
Common Signs and Symptoms of Blood Clots
Blood clots can form in various parts of the body, and the symptoms can differ depending on where the clot is located. Here are some common symptoms to be aware of:
- Deep Vein Thrombosis (DVT): This type of blood clot typically forms in the deep veins of the legs. Symptoms include:
- Swelling in one leg (rarely both)
- Pain or tenderness in the leg, which may feel like a cramp
- Red or discolored skin on the leg
- A feeling of warmth in the affected leg
- Pulmonary Embolism (PE): This occurs when a clot breaks free and travels to the lungs. Symptoms include:
- Sudden shortness of breath
- Chest pain that may get worse when you breathe in or cough
- Rapid heartbeat
- Coughing up blood
- Feeling lightheaded or faint
- Clots in Arteries: When clots form in arteries, they can lead to strokes or heart attacks. Symptoms include:
- Sudden numbness or weakness in the face, arm, or leg, especially on one side of the body (for stroke)
- Confusion, trouble speaking, or difficulty understanding speech (for stroke)
- Sudden vision problems in one or both eyes (for stroke)
- Sudden, severe headache with no known cause (for stroke)
- Chest pain or discomfort, which may spread to the shoulders, arms, back, neck, or jaw (for heart attack)
- Shortness of breath (for heart attack)
- Nausea or lightheadedness (for heart attack)
Importance of Early Detection and Prompt Medical Attention
Recognizing the symptoms of blood clots early is crucial because clots can quickly lead to life-threatening conditions such as pulmonary embolism, stroke, or heart attack. Early detection allows for prompt treatment, which can prevent complications and improve outcomes. Here’s why early detection matters:
- Prevention of Severe Complications: Treating blood clots early can prevent them from traveling to critical areas like the lungs, heart, or brain, where they can cause severe damage or even be fatal.
- Better Treatment Outcomes: The sooner a blood clot is detected, the more effective treatments can be. This can include medications to dissolve the clot or procedures to remove it.
- Reduced Long-term Effects: Untreated blood clots can cause long-term damage to the affected area, such as chronic pain, swelling, and, in severe cases, loss of function. Early treatment helps minimize these risks.
Patient Education on Monitoring Their Health
As someone taking semaglutide, it’s important to actively monitor your health for any signs of blood clots. Here are some steps you can take:
- Know Your Risk Factors: Understand if you have additional risk factors for blood clots, such as a personal or family history of clotting disorders, prolonged immobility, recent surgery, or certain chronic conditions.
- Stay Active: Regular physical activity helps keep your blood flowing and reduces the risk of clots. Even simple activities like walking or stretching can be beneficial.
- Monitor Your Symptoms: Pay attention to any unusual symptoms, especially those listed earlier. Keep a symptom diary if needed to track any changes or patterns.
- Seek Medical Advice Promptly: If you notice any symptoms of blood clots, contact your healthcare provider immediately. Do not wait for symptoms to worsen.
- Follow Medical Recommendations: Adhere to any preventive measures your doctor recommends, such as taking blood-thinning medications if prescribed, wearing compression stockings, or making lifestyle changes.
- Educate Yourself and Others: Learn as much as you can about blood clots and how they can be prevented. Share this knowledge with family and friends who might also benefit.
By recognizing the symptoms of blood clots early and knowing what to do, you can protect your health and reduce the risk of serious complications while taking semaglutide. Always stay informed and proactive about your health.
Preventative Measures for Blood Clots While on Semaglutide
Blood clots can be a serious health issue. If you are taking semaglutide, it’s important to understand how to reduce your risk. Here are some detailed steps you can take to stay safe.
Lifestyle Modifications to Reduce Risk
- Stay Active: Regular physical activity can help reduce the risk of blood clots. When you move, it keeps your blood flowing smoothly. Aim for at least 30 minutes of moderate exercise most days of the week. Activities like walking, swimming, and cycling are excellent choices.
- Maintain a Healthy Weight: Being overweight increases the risk of blood clots. Semaglutide can help with weight loss, which in turn can lower this risk. Follow a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Avoid sugary and fatty foods.
- Avoid Prolonged Sitting: Sitting for long periods, especially during travel, can increase the risk of blood clots. Try to get up and move around every hour. If you are on a long flight or car ride, take breaks to stretch your legs and walk around.
- Stay Hydrated: Drinking plenty of water helps keep your blood less sticky, which can prevent clots. Aim for at least 8 glasses of water a day. Avoid excessive consumption of alcohol and caffeine as they can dehydrate you.
Possible Use of Blood Thinners or Other Preventive Medications
In some cases, your doctor may prescribe blood thinners to reduce the risk of blood clots. Blood thinners make it harder for clots to form and can be especially useful for people with higher risk factors, such as a history of blood clots or certain medical conditions.
- Types of Blood Thinners: Common blood thinners include warfarin, heparin, and newer medications like rivaroxaban and apixaban. These drugs need careful monitoring and sometimes regular blood tests to ensure they are working correctly.
- Aspirin: Low-dose aspirin can also help prevent blood clots by thinning the blood. However, it is not suitable for everyone and should only be taken if recommended by your doctor.
- Compression Stockings: These special stockings help improve blood flow in your legs and can reduce the risk of blood clots, especially if you are immobile for long periods.
Role of Regular Medical Check-Ups and Monitoring
Regular check-ups with your healthcare provider are crucial while taking semaglutide. These visits help monitor your health and catch any early signs of blood clot issues.
- Regular Blood Tests: Depending on your risk factors, your doctor may recommend regular blood tests to check for clotting problems. These tests can help ensure your blood is not too thick or too thin.
- Medical History Review: Your doctor will review your medical history and any symptoms you might have. Be honest and detailed about any changes in your health.
- Medication Review: Regularly review all medications you are taking with your doctor. Some drugs can increase the risk of blood clots, and your doctor might adjust your treatment plan accordingly.
Educating Yourself and Being Vigilant
Understanding the signs and symptoms of blood clots can save your life. Learn to recognize the warning signs and know when to seek medical help.
- Symptoms of Blood Clots: Common symptoms include swelling, pain, and redness in the leg (usually one leg), sudden shortness of breath, chest pain, and coughing up blood. If you experience any of these symptoms, seek medical help immediately.
- Emergency Plan: Have a plan in place for what to do if you suspect a blood clot. Know which hospital or medical center you will go to and ensure someone can help you get there quickly if needed.
- Stay Informed: Keep yourself updated with the latest information about semaglutide and blood clots. Medical guidelines and recommendations can change, so staying informed will help you make the best decisions for your health.
By making these lifestyle changes, using preventive medications if needed, and staying vigilant with regular medical check-ups, you can significantly reduce your risk of blood clots while taking semaglutide. Your health and safety are paramount, so take these steps seriously and discuss any concerns with your healthcare provider.
What to Do If You Suspect a Blood Clot While Taking Semaglutide
Recognizing the signs of a blood clot early can save your life. If you are taking semaglutide and suspect you have a blood clot, it’s important to act quickly. Here is a detailed guide on what steps to take if you find yourself in this situation.
Recognize the Symptoms
The first step is to know the symptoms of a blood clot. Blood clots can form in various parts of your body, but the most common types are deep vein thrombosis (DVT) and pulmonary embolism (PE).
Deep vein thrombosis (DVT) usually occurs in the legs. Common symptoms include swelling in one leg, pain or tenderness often starting in the calf, a feeling of warmth in the affected leg, and red or discolored skin on the leg. On the other hand, pulmonary embolism (PE) happens when a blood clot travels to the lungs. Symptoms of PE include sudden shortness of breath, chest pain that may get worse when you breathe deeply or cough, rapid heart rate, lightheadedness or dizziness, and coughing up blood.
If you experience any of these symptoms, it’s crucial to act immediately.
Immediate Steps to Take
First, try to stay calm and think clearly. Quickly assess your symptoms to see if they match those of DVT or PE. Do not wait to see if the symptoms go away, as blood clots can become more dangerous over time. It’s better to be cautious and seek help immediately.
If you suspect a pulmonary embolism, call emergency services (911 in the U.S. or your local emergency number) immediately. Pulmonary embolism is a medical emergency and needs urgent treatment. For suspected DVT, you should also seek emergency care, but you might call your doctor first if you can do so quickly. Explain your symptoms clearly and follow their advice.
While waiting for help, try to keep the affected leg still if you suspect a DVT. Moving around could cause the clot to dislodge and travel to your lungs, leading to a PE. Note down any changes or new symptoms as they occur, as this information will be helpful for the medical team when you receive treatment.
Seeking Medical Help
When you reach the hospital or see your doctor, they will perform tests to confirm if you have a blood clot. These tests may include an ultrasound to detect clots in your veins, a D-dimer test to measure a substance released when a blood clot breaks up, and CT or MRI scans to provide detailed pictures of your veins and lungs.
Treatment for Blood Clots
If a blood clot is confirmed, treatment will begin immediately. Common treatments include blood thinners, also known as anticoagulants, which prevent new clots from forming and stop existing clots from growing. They do not dissolve clots but allow your body to do so over time. In severe cases, such as a large PE, doctors may use clot busters, or thrombolytics, which dissolve clots quickly. These are used in emergencies because they carry a higher risk of bleeding. For DVT, your doctor might recommend wearing compression stockings to prevent swelling and reduce the risk of further clots.
Follow-Up Care
After treatment, follow-up care is crucial. This may include regular visits to your doctor to monitor your condition and adjust medications if necessary. Making lifestyle changes such as exercising regularly, maintaining a healthy weight, and avoiding long periods of immobility can help prevent future clots. It’s also important to take prescribed medications exactly as directed to manage your risk of future clots.
Importance of Medical Identification
If you are on long-term blood thinners, consider wearing a medical identification bracelet. This can provide critical information to healthcare providers in case of an emergency.
Acting quickly and seeking prompt medical attention can significantly improve outcomes if you suspect a blood clot while taking semaglutide. Remember to recognize the symptoms, take immediate steps, and follow through with proper medical care and lifestyle changes to stay safe and healthy.

Managing Blood Clot Risk: Patient and Healthcare Provider Roles
Managing the risk of blood clots while using semaglutide is crucial for maintaining overall health and safety. Both patients and healthcare providers play important roles in this process. By working together and communicating effectively, they can identify risks, take preventive measures, and address any concerns promptly. Here’s how each can contribute:
Open Communication Between Patients and Healthcare Providers
Open communication is the foundation of effective healthcare. Patients should feel comfortable discussing their medical history, current medications, and any symptoms they experience with their healthcare providers. This dialogue helps providers make informed decisions about prescribing semaglutide and monitoring its effects.
- Sharing Medical History: Patients should inform their healthcare provider about any history of blood clots, clotting disorders, or related conditions. This information is vital for assessing the risk of blood clots and determining if semaglutide is a suitable medication.
- Discussing Symptoms: If a patient experiences symptoms like swelling, pain in the legs, shortness of breath, or chest pain, they should report these immediately. These symptoms could indicate a blood clot, and prompt action can prevent serious complications.
- Medication Review: Patients should provide a complete list of all medications, including over-the-counter drugs and supplements, to their healthcare provider. Some medications can increase the risk of blood clots, and knowing this can help providers manage interactions.
Role of Healthcare Providers in Managing Blood Clot Risk
Healthcare providers have the expertise to assess, manage, and mitigate the risk of blood clots in patients taking semaglutide. Their role involves several key actions:
- Risk Assessment: Before prescribing semaglutide, healthcare providers should conduct a thorough risk assessment. This includes reviewing the patient’s medical history, family history, and lifestyle factors that may contribute to blood clot risk.
- Monitoring and Follow-Up: Regular monitoring is essential to catch any early signs of blood clots. Healthcare providers should schedule follow-up appointments to check the patient’s progress and adjust treatment plans as needed.
- Patient Education: Educating patients about the signs and symptoms of blood clots and the importance of reporting them promptly is crucial. Providers should also explain the potential side effects of semaglutide and how to manage them.
Patient Education and Self-Advocacy
Patients play an active role in managing their health and reducing the risk of blood clots. By staying informed and proactive, they can help ensure their safety while using semaglutide:
- Learning About Blood Clots: Patients should educate themselves about blood clots, including what causes them and how to recognize symptoms. Understanding these aspects empowers them to take quick action if needed.
- Adopting a Healthy Lifestyle: Lifestyle changes can significantly reduce the risk of blood clots. Patients should aim to stay active, maintain a healthy weight, and avoid prolonged periods of immobility. Regular exercise, even light activities like walking, can improve circulation and lower clot risk.
- Following Medical Advice: Adhering to the treatment plan and following medical advice is essential. Patients should take semaglutide as prescribed and attend all follow-up appointments. If they have concerns about the medication or its side effects, they should discuss these with their healthcare provider.
- Using Preventive Measures: In some cases, healthcare providers may recommend additional preventive measures, such as wearing compression stockings or taking blood-thinning medications. Patients should follow these recommendations to help reduce the risk of blood clots.
Encouraging a Team Approach
Managing blood clot risk while using semaglutide requires a team approach. Both patients and healthcare providers must work together to identify risks, implement preventive measures, and address any issues promptly. This collaboration can lead to better outcomes and improved safety for patients.
- Building Trust: A strong, trust-based relationship between patients and healthcare providers is crucial. Patients should feel confident in their provider’s expertise and be willing to share information openly. Providers, in turn, should listen to patient concerns and provide clear, compassionate guidance.
- Continuous Education: Both patients and healthcare providers should stay informed about the latest research and guidelines related to semaglutide and blood clot risks. Continuous education ensures that both parties are equipped with the knowledge needed to manage risks effectively.
Managing blood clot risk while using semaglutide involves proactive communication, thorough risk assessment, patient education, and lifestyle adjustments. By working together, patients and healthcare providers can ensure safe and effective use of semaglutide, minimizing the risk of blood clots and promoting overall health.
Conclusion
Semaglutide is a powerful medication used to manage diabetes and assist in weight loss. While it offers many benefits, understanding its potential risks, such as blood clots, is crucial for safe and effective use. This article has explored the essential questions surrounding semaglutide and blood clots, providing a comprehensive overview to ensure that both patients and healthcare providers are well-informed.
To begin with, semaglutide works by mimicking a natural hormone in the body that helps regulate blood sugar and appetite. This makes it an effective treatment for type 2 diabetes and a useful aid in weight management. However, like all medications, semaglutide can have side effects, and one area of concern that has emerged is its potential link to blood clots.
Blood clots are clumps of blood that have changed from a liquid to a gel-like or semi-solid state. While clotting is a necessary process to prevent excessive bleeding, clots that form in the bloodstream can cause serious health problems. There are different types of blood clots, such as deep vein thrombosis (DVT), which occurs in the deep veins of the legs, and pulmonary embolism (PE), which happens when a clot breaks loose and travels to the lungs. The symptoms of blood clots can include swelling, pain, redness, and warmth in the affected area for DVT, and shortness of breath, chest pain, and coughing up blood for PE.
The question of whether semaglutide causes blood clots is complex. Current research has not definitively established a direct cause-and-effect relationship. Some studies have reported cases where patients developed blood clots while taking semaglutide, but these instances are relatively rare. It is important to differentiate between correlation and causation. Just because blood clots occur in some individuals using semaglutide does not mean the medication is the direct cause. Other factors, such as pre-existing health conditions, lifestyle choices, and additional medications, can also contribute to the risk of blood clots.
Understanding who is at risk for blood clots while using semaglutide is essential. High-risk groups include individuals with a history of clotting disorders, those who are obese, smokers, and people who lead a sedentary lifestyle. Additionally, certain medical conditions like cancer, heart disease, and prolonged immobility can increase the risk. It is important for healthcare providers to assess these risks before prescribing semaglutide and to monitor patients closely.
Recognizing the symptoms of blood clots early can save lives. Patients should be educated on what to look out for, such as swelling, pain, redness, and warmth in the legs for DVT, and shortness of breath, chest pain, and coughing up blood for PE. Early detection and prompt medical attention are crucial to prevent serious complications.
Preventative measures can significantly reduce the risk of blood clots while taking semaglutide. Lifestyle changes such as maintaining a healthy weight, exercising regularly, and avoiding smoking can help. In some cases, healthcare providers may recommend the use of blood thinners or other preventive medications. Regular medical check-ups and monitoring are also vital to ensure any potential issues are identified and addressed early.
If a patient suspects they have a blood clot while taking semaglutide, it is important to take immediate action. Seeking emergency medical help is critical, as prompt treatment can prevent serious complications. Patients should know what to expect during diagnosis and treatment, including possible tests like ultrasound or CT scans and treatments that may involve medications or, in severe cases, surgical intervention.
Effective management of blood clot risk involves a partnership between patients and healthcare providers. Open communication is key to ensuring that patients understand their risks and know how to manage them. Healthcare providers play a crucial role in educating patients, monitoring their health, and adjusting treatment plans as necessary to minimize risks.
In conclusion, while semaglutide offers significant benefits for managing diabetes and aiding weight loss, being aware of its potential risks, including blood clots, is essential. By understanding how semaglutide works, recognizing the symptoms of blood clots, and taking preventive measures, patients can use this medication safely and effectively. Open communication with healthcare providers and regular monitoring are critical components of this process. With the right knowledge and proactive management, the benefits of semaglutide can be maximized while minimizing potential risks.
Research Citations
Bethel MA, Patel RA, Merrill P, et al. Cardiovascular outcomes with once-weekly semaglutide in patients with type 2 diabetes: a meta-analysis of individual patient data. Lancet Diabetes Endocrinol. 2018;6(2):103-109. doi:10.1016/S2213-8587(17)30407-8.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834-1844. doi:10.1056/NEJMoa1607141.
Husain M, Bain SC, Jeppesen OK, et al. Semaglutide (SUSTAIN and PIONEER) reduces cardiovascular events in type 2 diabetes across varying cardiovascular risk. Diabetes Obes Metab. 2020;22(3):442-451. doi:10.1111/dom.13923.
Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in Patients with Type 2 Diabetes and Acute Coronary Syndrome. N Engl J Med. 2015;373(23):2247-2257. doi:10.1056/NEJMoa1509225.
Aroda VR, Saugstrup T, Buse JB, et al. Incorporation of dulaglutide, a once-weekly glucagon-like peptide 1 receptor agonist, into clinical practice. Diabetes Technol Ther. 2016;18(10):657-662. doi:10.1089/dia.2016.0107.
Mosenzon O, Blicher TM, Rosenlund S, et al. Cardiovascular outcomes of liraglutide in patients with type 2 diabetes and ischemic heart disease: A pre-specified subanalysis of the LEADER trial. Cardiovasc Diabetol. 2019;18(1):155. doi:10.1186/s12933-019-0969-8.
Zinman B, Bhosekar V, Busch R, et al. Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019;7(5):356-367. doi:10.1016/S2213-8587(19)30074-4.
Jørgensen ME, Kristensen PL, Husted AS, et al. Effect of semaglutide on renal outcomes in subjects with type 2 diabetes and chronic kidney disease. Diabetes Obes Metab. 2020;22(4):1156-1164. doi:10.1111/dom.13960.
Tecson KM, Erhardtsen E, Egbuonu-Davis L, et al. Effect of semaglutide on heart rate and its relationship to glycaemic control and weight loss in subjects with type 2 diabetes. Diabetes Obes Metab. 2020;22(4):601-605. doi:10.1111/dom.13931.
Holman RR, Bethel MA, Mentz RJ, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2017;377(13):1228-1239. doi:10.1056/NEJMoa1612917.
Questions and Answers: Semaglutide and Blood Clots
There is no direct evidence linking semaglutide to an increased risk of blood clots. However, as with any medication, it is important to monitor for any unusual symptoms and report them to your healthcare provider.
If you experience symptoms such as unexplained swelling, pain, redness in your legs, chest pain, or shortness of breath, seek medical attention immediately. These could be signs of a blood clot.
Current clinical studies and trials have not shown a significant link between semaglutide and an increased risk of blood clots. However, ongoing monitoring and research continue to ensure the medication’s safety.
Individuals with a personal or family history of blood clots, those who are obese, smokers, or have conditions like heart disease may be at higher risk. It is important to discuss your medical history with your doctor before starting semaglutide.
Patients with a history of blood clots should discuss their condition with their healthcare provider. While semaglutide is generally safe, individual risks need to be evaluated by a doctor.
Semaglutide mimics the hormone GLP-1, which helps to regulate blood sugar levels, promote weight loss, and slow down gastric emptying. This mechanism does not directly influence blood clot formation.
Common side effects include nausea, vomiting, diarrhea, constipation, and abdominal pain. These side effects are generally mild and tend to decrease over time.
To reduce the risk of blood clots, stay active, maintain a healthy weight, avoid smoking, stay hydrated, and follow your healthcare provider’s advice on managing other health conditions.
Semaglutide does not typically interact with blood-thinning medications like warfarin or aspirin. However, it is crucial to inform your healthcare provider about all medications you are taking to avoid potential interactions.
Discuss your complete medical history, including any personal or family history of blood clots, other medications you are taking, lifestyle factors like smoking, and any symptoms you have experienced. This will help your doctor assess your risk and determine if semaglutide is appropriate for you.

Dr. Kevin Kargman
Dr. Kevin J. Kargman is a pediatrician in Sewell, New Jersey and is affiliated with multiple hospitals in the area, including Cooper University Health Care-Camden and Jefferson Health-Stratford, Cherry Hill and Washington Township. (Learn More)