Table of Contents
Section 1: Introduction
Urinary Tract Infections (UTIs) are a prevalent condition affecting millions globally, with significant implications for patient well-being and healthcare systems. These infections, characterized by a range of uncomfortable symptoms, can impact anyone but are notably more common in certain populations. The management of UTIs often involves antibiotics, which, while effective, underscores the need for preventive strategies, particularly among individuals at higher risk due to medical conditions or medication use.
Semaglutide, a relatively new player in the pharmacological landscape, has garnered attention not just for its efficacy in managing Type 2 diabetes but also for its benefits in weight loss. As a glucagon-like peptide-1 (GLP-1) receptor agonist, semaglutide mimics an intestinal hormone that stimulates insulin release, thereby lowering blood sugar. Beyond its primary use, its role in weight management has been revolutionary, offering hope to those struggling with obesity, a condition known to exacerbate numerous health issues, including diabetes.
The introduction of semaglutide into the market has been met with enthusiasm, marked by its promising results in clinical trials and real-world applications. However, like all medications, it comes with a spectrum of side effects, ranging from mild gastrointestinal disturbances to more severe reactions. Among these, the potential link between semaglutide and an increased risk of UTIs has emerged as a topic of interest. This connection invites a closer examination, given the widespread use of the drug and the commonality of UTIs. Understanding whether semaglutide contributes to a heightened risk of UTIs is crucial, as it would influence patient management, medication counseling, and the development of strategies to mitigate such risks.
This article delves into the relationship between semaglutide and urinary tract infections, aiming to provide a comprehensive overview that addresses common questions and concerns. By exploring the mechanism of action of semaglutide, its benefits and side effects, and the nature of UTIs—including their causes, symptoms, and treatments—we seek to illuminate any potential links between the medication and UTIs. Additionally, we will examine other drug interactions that may promote UTIs and offer strategies for patients experiencing recurrent infections. Through a detailed analysis, supported by current research and clinical insights, this article aims to equip patients, healthcare providers, and researchers with the knowledge to navigate this complex intersection of drug therapy and infection risk.
Section 2: Overview of Semaglutide
Semaglutide represents a significant advancement in the treatment of Type 2 diabetes and obesity, two conditions with growing prevalence worldwide. As a glucagon-like peptide-1 (GLP-1) receptor agonist, it operates by mimicking the action of the incretin hormone, which plays a pivotal role in glucose homeostasis. Incretin hormones, such as GLP-1, are secreted by the gut in response to food intake and enhance insulin secretion from the pancreas in a glucose-dependent manner. Semaglutide’s ability to bind to the GLP-1 receptor with high affinity makes it an effective agent in lowering blood glucose levels in individuals with Type 2 diabetes.
Beyond glycemic control, semaglutide has a notable impact on weight management. Its mechanism extends to slowing gastric emptying and promoting satiety, which in turn assists in reducing caloric intake and supports significant weight loss. This dual action—managing both blood sugar levels and body weight—positions semaglutide as a versatile tool in the management of diabetes and obesity, offering benefits that extend beyond traditional treatment modalities.
The development of semaglutide was a result of extensive research into incretin-based therapies, seeking to harness the beneficial effects of GLP-1 in a more stable and longer-lasting formulation. Semaglutide’s once-weekly subcutaneous injection form, and more recently, an oral tablet, have improved patient adherence and satisfaction, addressing some of the challenges associated with daily diabetes management regimens.
Clinical trials have consistently demonstrated the efficacy of semaglutide in reducing hemoglobin A1c levels, a marker of long-term glucose control, and facilitating weight loss. The SUSTAIN and PIONEER trial series highlighted not only its effectiveness in these areas but also its cardiovascular safety profile, making it a suitable option for a broad spectrum of patients, including those with a high risk of cardiovascular events.
However, the introduction of any new medication necessitates a thorough understanding of its side effects. For semaglutide, these include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and abdominal pain, which are generally transient and diminish over time. More serious concerns, such as pancreatitis, changes in vision, and renal impairment, have been noted but occur less frequently. The exploration of semaglutide’s side effects has also prompted investigations into its relationship with urinary tract infections. Given the drug’s systemic effects and its impact on metabolism, understanding any potential link to UTIs is critical for comprehensive patient care. As we delve further into semaglutide’s role in the management of diabetes and obesity, the balance between its benefits and risks remains a focal point of discussion among healthcare providers and researchers alike.
Section 3: Understanding UTIs
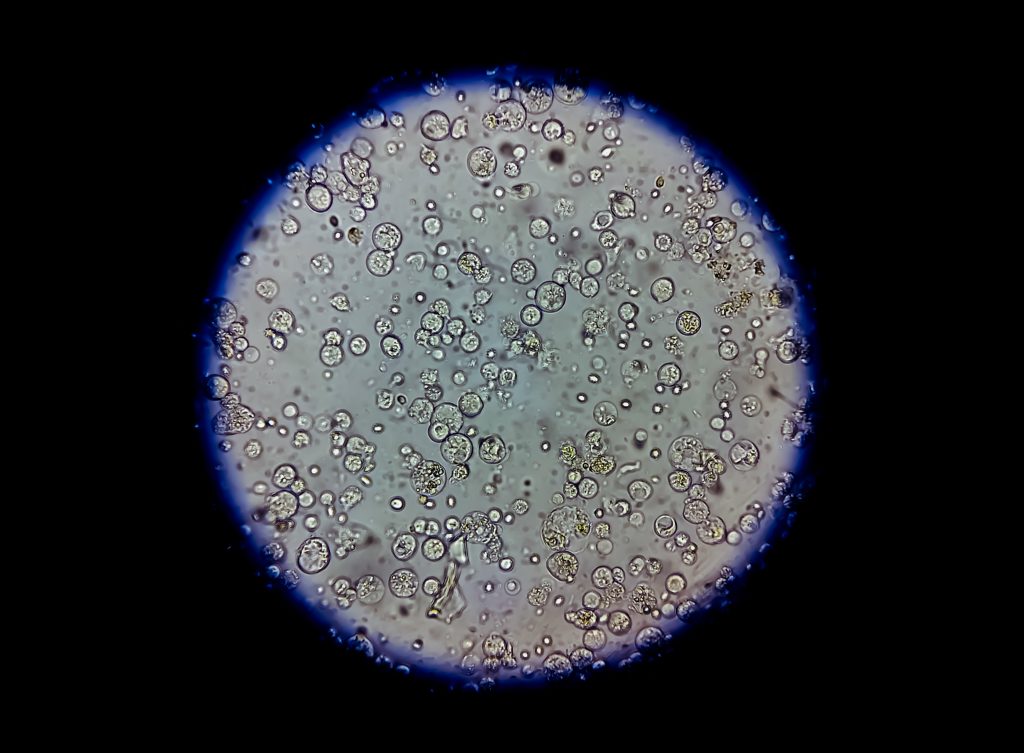
Urinary tract infections (UTIs) stand as one of the most common infections affecting individuals worldwide, presenting a significant health concern due to their frequency, recurrence, and potential for leading to more serious conditions. Characterized by the invasion and multiplication of pathogens within the urinary tract, UTIs can affect different parts of the system, including the bladder (cystitis), urethra (urethritis), and kidneys (pyelonephritis). Symptoms vary depending on the infection site but often include a persistent urge to urinate, a burning sensation during urination, cloudy or strong-smelling urine, and pelvic pain in women.
The primary cause of UTIs is the entry of bacteria, usually Escherichia coli (E. coli), from the bowel into the urinary tract through the urethra. Once these pathogens bypass the body’s defense mechanisms, they attach to the walls of the urinary tract, leading to infection. Women are particularly at risk due to their shorter urethra, which allows bacteria easier access to the bladder. Other risk factors contributing to UTI susceptibility include sexual activity, certain types of birth control, menopause, urinary catheter use, urinary tract abnormalities, and a suppressed immune system.
The treatment of UTIs typically involves antibiotics to eliminate the infection, with the choice of medication and duration of treatment depending on the infection’s severity and location. While effective, the repeated use of antibiotics poses concerns about antibiotic resistance, underscoring the importance of preventive measures and alternative strategies for managing recurrent UTIs.
Preventive strategies are crucial in reducing UTI risk and include maintaining proper hydration, practicing good urinary and genital hygiene, urinating after sexual intercourse to flush out bacteria, and avoiding irritants such as harsh soaps and spermicides. For individuals with recurrent UTIs, healthcare providers may recommend prophylactic antibiotics, lifestyle adjustments, or investigate underlying causes that may necessitate specialized treatment. Understanding UTIs, their causes, symptoms, and treatments is essential for managing this common condition and preventing its recurrence. By recognizing the risk factors and implementing preventive measures, individuals can significantly reduce their susceptibility to UTIs and the need for antibiotic treatment, thereby mitigating the risk of antibiotic resistance and ensuring better urinary tract health.

Section 4: Exploring the Link between Semaglutide and UTIs
The relationship between semaglutide use and urinary tract infections (UTIs) has garnered attention within the medical community, prompted by reported cases and clinical trial data suggesting a potential association. Semaglutide, widely used for its efficacy in managing Type 2 diabetes and obesity, has been observed to have a range of side effects, with UTIs being among the concerns raised by patients and healthcare providers.
To explore this link, it is crucial to examine the mechanism by which semaglutide could potentially influence UTI risk. Semaglutide operates by mimicking the incretin hormone GLP-1, enhancing insulin secretion, and delaying gastric emptying, which aids in blood glucose control and weight management. While these effects are beneficial for metabolic health, the question arises whether semaglutide’s impact on the body’s metabolism and immune function might inadvertently affect the urinary tract’s susceptibility to infections.
Clinical trials and observational studies provide valuable insights into this issue. Data from such studies indicate a slightly increased incidence of UTIs among semaglutide users compared to control groups. However, these findings necessitate a nuanced interpretation. It is important to consider factors such as the patient’s baseline UTI risk, the role of concurrent conditions like diabetes and obesity (which independently increase UTI risk), and the overall health profile of the study population.
The increased glucose levels in the urine of patients with poorly controlled diabetes can encourage bacterial growth, leading to a higher UTI risk. As semaglutide improves glycemic control, theoretically, it should reduce this risk over time. However, the initial changes in glucose metabolism and urinary composition following semaglutide initiation might temporarily alter the urinary environment, potentially influencing UTI susceptibility.
Furthermore, the weight loss associated with semaglutide use could alter immune function and the body’s defense mechanisms against infections, including UTIs. While weight loss generally has positive effects on health, rapid changes in body composition may have complex impacts on immune responses.
Current research suggests that while there may be a slight increase in UTI risk with semaglutide use, the benefits of the medication in managing diabetes and obesity likely outweigh this risk for most patients. It remains essential for healthcare providers to monitor patients for UTIs and other side effects, providing guidance on preventive measures and managing symptoms should they arise. The link between semaglutide and UTIs is an area of ongoing research. While preliminary data suggest a potential association, further studies are needed to fully understand the mechanisms at play and to develop strategies for minimizing UTI risk in patients using semaglutide.
Section 5: Drug Interactions and UTI Risk
The consideration of drug interactions is crucial in managing health conditions, especially for those on complex medication regimens, such as patients with Type 2 diabetes or obesity. Certain medications can influence the risk of developing urinary tract infections (UTIs) either by altering the body’s immune response, affecting the urinary tract’s natural defenses, or through direct pharmacological effects. While semaglutide is the focus of our discussion, understanding the broader landscape of drug interactions that may promote UTIs is vital for comprehensive patient care.
Pharmacologically, some medications can disrupt the balance of microflora in the body or modify urine composition, creating a more conducive environment for bacterial growth. For instance, drugs that cause urinary retention or reduce bladder emptying can increase UTI risk by allowing bacteria to multiply in the urinary tract. Medications such as anticholinergics, commonly used to treat overactive bladder, and some antipsychotics, have these side effects.
Moreover, certain classes of medications can impact immune system function, indirectly affecting the body’s ability to fight off infections. Corticosteroids, for example, widely used for their anti-inflammatory properties, can suppress immune responses, potentially elevating the risk of infections, including UTIs. Similarly, immunosuppressants, critical in managing autoimmune diseases and preventing organ transplant rejection, may increase susceptibility to UTIs by dampening the body’s defense mechanisms against pathogens.
Diabetes medications, in general, warrant particular attention due to the direct relationship between glucose control and UTI risk. Poor glycemic control can lead to higher levels of glucose in the urine, fostering a favorable environment for bacterial growth. While semaglutide aims to improve glycemic control, the initial adjustment period or any disruption in medication adherence could temporarily heighten UTI risk.
In the context of semaglutide, it’s also pertinent to consider its interaction with other medications prescribed for weight loss or diabetes management. The combined effects of multiple agents on gastric motility, glucose excretion, and immune modulation may cumulatively influence UTI risk. Therefore, a careful review of a patient’s medication regimen is essential, looking for potential interactions that could predispose them to UTIs or other adverse effects.
Healthcare providers should adopt a proactive approach, assessing medication regimens for potential UTI-promoting interactions and discussing preventive measures with patients. This might include strategies such as monitoring for symptoms of UTIs, maintaining good hydration, and possibly adjusting medications if recurrent UTIs become a significant issue. Ultimately, the goal is to balance effective management of the primary health condition with minimizing the risk of secondary complications like UTIs.
Section 6: Strategies for Patients with Recurring UTIs
Recurrent urinary tract infections (UTIs) pose a significant challenge for patients, impacting their quality of life and increasing the risk of complications. For individuals experiencing frequent UTIs, especially those on medications like semaglutide or with conditions like diabetes and obesity, developing effective prevention and management strategies is critical. This section outlines approaches to reduce the incidence of UTIs, focusing on lifestyle modifications, medical interventions, and personalized care plans.
Lifestyle Modifications: Simple changes in daily habits can significantly reduce UTI risk. Adequate hydration is fundamental, as it helps flush bacteria from the urinary tract. Patients should be encouraged to drink plenty of water throughout the day. Cranberry products, often touted for their UTI-preventing properties, can be beneficial for some individuals, although results vary and more research is needed to confirm their effectiveness. Good urinary hygiene, such as urinating after sexual intercourse and avoiding irritants like scented soaps and douches, is also advised.
Dietary Considerations: A balanced diet that supports immune function and overall health can play a role in preventing UTIs. Foods rich in antioxidants and vitamins, such as fruits, vegetables, and whole grains, should be emphasized. Additionally, reducing sugar intake may help manage blood glucose levels, potentially decreasing the risk of UTIs in diabetic patients.
Medical Interventions: For patients with recurrent UTIs, prophylactic antibiotics may be considered. This approach, however, requires careful consideration due to the risk of antibiotic resistance. Alternatives such as methenamine hippurate, a urinary antiseptic, might be recommended in certain cases. It’s essential for healthcare providers to tailor these interventions based on the patient’s medical history, current medications, and risk factors.
Personalized Care Plans: Recognizing the unique factors contributing to each patient’s UTI risk is crucial. For individuals on semaglutide or other medications that may influence UTI risk, regular monitoring and discussions about side effects are important. Adjusting the medication regimen, exploring alternative treatments for underlying conditions, and addressing modifiable risk factors can all be part of a comprehensive care plan.
Education and Empowerment: Equipping patients with knowledge about UTI prevention, symptoms, and the importance of early treatment can empower them to take an active role in managing their health. Education should include information on recognizing the signs of a UTI, when to seek medical advice, and strategies for reducing recurrence.
For patients with recurrent UTIs, a multi-faceted approach that combines lifestyle changes, medical interventions, and personalized care can be effective in reducing the frequency of infections. By addressing the underlying risk factors and providing targeted support, healthcare providers can help patients achieve better urinary tract health and improve their overall well-being.

Section 7: Managing UTI Risk in Patients on Semaglutide
In the context of increasing semaglutide use for Type 2 diabetes and obesity management, understanding how to mitigate the associated risk of urinary tract infections (UTIs) is essential for healthcare providers and patients alike. Semaglutide, while offering significant benefits in glycemic control and weight reduction, has been observed to potentially increase UTI risk, necessitating strategies to manage this risk effectively. This section outlines approaches to minimize UTI occurrences in patients using semaglutide, focusing on proactive measures, patient education, and tailored healthcare strategies.
Proactive Monitoring and Early Intervention: Regular monitoring for UTI symptoms is crucial for patients on semaglutide. Healthcare providers should educate patients about the signs of UTIs, such as increased urgency, painful urination, and cloudy or foul-smelling urine, and encourage them to report these symptoms promptly. Early detection and treatment of UTIs can prevent complications and reduce the risk of recurrent infections.
Hydration and Dietary Measures: Encouraging adequate hydration is a simple yet effective strategy to help flush bacteria from the urinary system, reducing UTI risk. Patients should be advised to consume plenty of water throughout the day. Dietary recommendations can also include foods with high water content and potentially cranberry products, though the latter should be considered on a case-by-case basis given the mixed evidence regarding their efficacy in UTI prevention.
Lifestyle Adjustments: Lifestyle modifications play a significant role in managing UTI risk. Patients should be counseled on proper genital hygiene practices, such as wiping from front to back and urinating after sexual activity to minimize bacterial exposure. For individuals with diabetes, maintaining optimal glycemic control is also crucial, as elevated glucose levels in the urine can promote bacterial growth.
Reviewing Medication Regimens: For patients experiencing recurrent UTIs while on semaglutide, a thorough review of their medication regimen may be necessary. This includes evaluating the use of semaglutide in conjunction with other medications that may affect UTI risk or urinary function. Adjustments to the medication regimen should be considered if alternative treatments can provide similar benefits with a lower risk of UTIs.
Individualized Patient Education: Tailoring education to the individual patient’s needs, including discussions on the importance of medication adherence, lifestyle and dietary recommendations, and strategies for UTI prevention, is essential. Empowering patients with knowledge and practical advice enables them to take an active role in their health management, potentially reducing the incidence of UTIs.
Managing UTI risk in patients on semaglutide requires a comprehensive approach that includes proactive monitoring, patient education, lifestyle and dietary modifications, and a careful review of medication regimens. By adopting these strategies, healthcare providers can help minimize UTI risk, enhancing the overall effectiveness of semaglutide treatment and improving patient outcomes.
Section 8: Research Citations
Semaglutide, a glucagon-like peptide-1 receptor agonist (GLP-1 RA), has emerged as a promising therapy for type 2 diabetes mellitus due to its potent glucose-lowering effects and cardiovascular benefits. However, recent clinical trials have raised concerns regarding its association with urinary tract infections (UTIs). This review examines the existing evidence on the relationship between semaglutide use and UTIs to provide clinicians with valuable insights into the potential risks and benefits of this medication.
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834-1844. doi:10.1056/NEJMoa1607141
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669-2701. doi:10.2337/dci18-0033
- Aroda VR, Bain SC, Cariou B, et al. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol. 2017;5(5):355-366. doi:10.1016/S2213-8587(17)30092-4
- Pratley RE, Aroda VR, Lingvay I, et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 2018;6(4):275-286. doi:10.1016/S2213-8587(18)30024-X
- Ahrén B, Masmiquel L, Kumar H, et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-week, open-label, randomized clinical trial. Diabetes Care. 2018;41(2):258-266. doi:10.2337/dc17-1200
- US Food and Drug Administration (FDA). Highlights of prescribing information: Rybelsus (semaglutide) tablets, for oral use. Accessed January 10, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf
- Holst JJ, Vilsbøll T, Deacon CF. The incretin system and its role in type 2 diabetes mellitus. Mol Cell Endocrinol. 2009;297(1-2):127-136. doi:10.1016/j.mce.2008.08.012
- Frias JP, Nauck MA, Van J, et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet. 2018;392(10160):2180-2193. doi:10.1016/S0140-6736(18)32260-8
- Iepsen EW, Torekov SS, Holst JJ. Liraglutide for type 2 diabetes and obesity: a 2015 update. Expert Rev Cardiovasc Ther. 2015;13(7):753-767. doi:10.1586/14779072.2015.1045775
- Jendle J, Grunberger G, Blevins T, et al. Efficacy and safety of dulaglutide in the treatment of type 2 diabetes: a comprehensive review of the dulaglutide clinical data focusing on the AWARD phase 3 clinical trial program. Diabetes Metab Res Rev. 2016;32(8):776-790. doi:10.1002/dmrr.2812
Section 9: Conclusion
The relationship between semaglutide use and the risk of urinary tract infections (UTIs) represents a complex interplay of pharmacological effects, patient-specific factors, and broader health considerations. Semaglutide, as a GLP-1 receptor agonist, has transformed the therapeutic landscape for individuals with Type 2 diabetes and obesity, offering significant benefits in terms of glycemic control and weight reduction. However, the potential for increased UTI risk necessitates a nuanced understanding and proactive management strategies to ensure patient safety and optimal treatment outcomes.
Throughout this article, we have explored the mechanisms by which semaglutide exerts its effects, the nature of UTIs and their impact on health, and the potential link between semaglutide use and increased UTI incidence. We have also delved into the broader context of drug interactions and their role in UTI risk, alongside practical strategies for patients experiencing recurrent UTIs. This comprehensive approach underscores the importance of balancing the undeniable benefits of semaglutide with the need to mitigate adverse effects, including UTIs.
Key to managing UTI risk in patients on semaglutide is a multifaceted strategy that includes patient education, lifestyle modifications, regular monitoring for symptoms, and, when necessary, medical intervention. Patients should be empowered with knowledge about UTI prevention, signs and symptoms of infections, and the importance of maintaining optimal hydration and hygiene practices. Healthcare providers play a crucial role in this process, offering tailored advice, reviewing medication regimens for potential interactions, and closely monitoring patient progress.
Moreover, the exploration of drug interactions highlights the critical need for a holistic view of patient care, particularly for those with complex medical histories or on multiple medications. Understanding how different drugs can influence UTI risk, either directly or indirectly, is essential for preventing infections and ensuring the safe use of semaglutide and other medications.
In conclusion, while semaglutide presents a valuable tool in the management of diabetes and obesity, its potential association with UTIs requires attention and proactive management. Future research should continue to elucidate this relationship, exploring the underlying mechanisms and developing strategies to minimize UTI risk. By fostering a collaborative approach between patients and healthcare providers, it is possible to maximize the benefits of semaglutide while minimizing its risks, enhancing the quality of care for individuals with Type 2 diabetes and obesity. For personalized care and expert advice, don’t hesitate to contact us at BMI Doctors today.
Questions and Answers: Semaglutide and UTI
Research suggests a potential link between semaglutide use and an increased incidence of UTIs. However, the risk appears to be relatively small and should be balanced against the significant benefits of semaglutide in managing Type 2 diabetes and obesity.
Users should watch for increased urgency and frequency of urination, a burning sensation when urinating, cloudy or strong-smelling urine, and pelvic pain. Early detection and treatment of UTIs can prevent complications.
Individuals with a history of recurrent UTIs, women, the elderly, and those with compromised immune systems may be at higher risk and should take additional precautions.
Maintaining proper hydration, practicing good urinary and genital hygiene, and monitoring for UTI symptoms can help reduce your risk. Discuss any concerns with your healthcare provider for personalized advice.
Do not stop taking semaglutide without consulting your healthcare provider. UTIs can typically be treated with antibiotics without the need to discontinue semaglutide therapy.
Management includes prescribing antibiotics for the infection and reviewing the patient’s overall medication regimen and health status to adjust treatment plans as necessary.
Current research does not indicate a significant difference in UTI risk between the injectable and oral forms of semaglutide. Patient experience may vary, and both forms have similar efficacy and safety profiles.
There is no evidence to suggest that semaglutide affects the severity of UTIs. The severity is more likely influenced by individual health factors and the timeliness of treatment.
UTI symptoms are generally consistent across populations, whether or not they are taking semaglutide. However, individuals with diabetes may experience more frequent or severe infections.
For the most reliable information, consult your healthcare provider and review the patient information leaflet provided with your medication. Reputable medical websites and resources recommended by your healthcare provider can also offer valuable insights.

Dr. Melissa VanSickle
Dr. Melissa Vansickle, MD is a family medicine specialist in Onsted, MI and has over 24 years of experience in the medical field. She graduated from University of Michigan Medical School in 1998. She is affiliated with medical facilities Henry Ford Allegiance Health and Promedica Charles And Virginia Hickman Hospital. Her subspecialties include General Family Medicine, Urgent Care, Complementary and Integrative Medicine in Rural Health.
