Table of Contents
Section 1: What is Semaglutide and How Does it Work?
Semaglutide, a revolutionary treatment in the realm of diabetes and obesity management, has emerged as a significant player in modern medicine. As a glucagon-like peptide-1 (GLP-1) receptor agonist, semaglutide mimics the action of the GLP-1 hormone, a naturally occurring hormone involved in glucose regulation. GLP-1 plays a pivotal role in controlling blood sugar levels, particularly after eating, making it a target for therapeutic interventions in conditions like type 2 diabetes.
The mechanism of action of semaglutide is multifaceted. Firstly, it stimulates the pancreas to produce more insulin when blood glucose levels are high. Insulin is a hormone crucial for the uptake of glucose by cells, thereby reducing blood sugar levels. This insulinotropic effect is glucose-dependent, which means that semaglutide stimulates insulin secretion more effectively when blood glucose levels are high, reducing the risk of hypoglycemia, a common side effect of many diabetes medications.
Furthermore, semaglutide suppresses the secretion of glucagon, another hormone produced by the pancreas. Glucagon typically acts to increase blood glucose levels by promoting the release of stored glucose from the liver. By inhibiting glucagon secretion, semaglutide contributes to the reduction of blood sugar levels.
An important aspect of semaglutide’s action is its effect on gastric emptying. It slows down the rate at which the stomach empties its contents into the small intestine, leading to a feeling of fullness and satiety. This delayed gastric emptying not only helps in controlling appetite but also modulates postprandial glucose levels, contributing to better glycemic control.
Additionally, semaglutide appears to act on the brain’s appetite centers. By modulating appetite-regulating pathways in the brain, it reduces hunger and caloric intake, which is a crucial aspect of its role in weight management. This central action complements its peripheral effects, making it a potent agent for treating conditions like obesity, which often co-exists with type 2 diabetes.
The clinical development and approval of semaglutide mark a significant advancement in diabetes care. Its efficacy in lowering HbA1c — a key marker for long-term glycemic control — has been demonstrated in numerous clinical trials. Moreover, the convenience of its dosing, typically a once-weekly subcutaneous injection, enhances patient compliance compared to therapies requiring more frequent administration. Semaglutide’s mode of action encompasses a blend of metabolic effects that extend beyond mere glycemic control, offering a holistic approach to managing conditions intertwined with metabolism and energy balance. Its ability to improve blood sugar levels, aid in weight loss, and potentially impact cardiovascular risk factors, positions it as a transformative option in the treatment of type 2 diabetes and related conditions.
Section 2: Semaglutide's Role in Diabetes Management
Semaglutide has revolutionized the management of type 2 diabetes, a chronic condition characterized by insulin resistance and progressive loss of beta-cell function. The imperative in managing type 2 diabetes lies in achieving and maintaining optimal blood glucose levels, thus reducing the risk of complications such as neuropathy, nephropathy, retinopathy, and cardiovascular disease. Semaglutide, with its unique mechanism of action, plays a crucial role in this therapeutic landscape.
The effectiveness of semaglutide in diabetes management primarily stems from its ability to improve glycemic control. It significantly lowers hemoglobin A1c (HbA1c) levels, a key indicator of blood sugar control over the past two to three months. Clinical trials have consistently demonstrated that semaglutide can reduce HbA1c levels by up to 1.5%, a significant reduction for individuals with diabetes. This improvement in glycemic control is vital in preventing the long-term complications of diabetes.
In addition to improving HbA1c levels, semaglutide aids in the reduction of fasting plasma glucose — the blood sugar level after an overnight fast. This reduction is vital for preventing the chronic complications associated with high blood sugar levels. By enhancing the body’s response to insulin and reducing the amount of glucose released by the liver, semaglutide ensures a more stable blood sugar profile throughout the day.
Moreover, semaglutide’s impact on weight management is particularly beneficial for individuals with type 2 diabetes, many of whom struggle with obesity. Obesity exacerbates insulin resistance, making diabetes management more challenging. By reducing appetite and caloric intake, semaglutide not only aids in weight loss but also improves insulin sensitivity. This dual action of improving blood sugar control while aiding in weight reduction is a significant advantage over other antidiabetic medications that may cause weight gain.
The cardiovascular benefits of semaglutide are another critical aspect of its role in diabetes management. Individuals with type 2 diabetes have an increased risk of cardiovascular diseases. Semaglutide has been shown to reduce the risk of major adverse cardiovascular events, including heart attack and stroke, in people with type 2 diabetes. This cardiovascular protective effect is a significant milestone, as cardiovascular disease is a leading cause of mortality in diabetes patients.
Furthermore, the once-weekly dosing of semaglutide enhances treatment adherence, a common challenge in diabetes management. The ease of administration, coupled with its efficacy and safety profile, makes semaglutide a preferred choice for many patients and healthcare providers. Semaglutide represents a paradigm shift in diabetes management. Its comprehensive approach in improving glycemic control, aiding in weight loss, and providing cardiovascular benefits addresses the multifaceted challenges faced by individuals with type 2 diabetes, making it a cornerstone in the management of this complex condition.
Section 3: Weight Loss Benefits of Semaglutide
The weight loss benefits of semaglutide, particularly for individuals struggling with obesity, mark a groundbreaking advancement in medical science. Obesity, a global epidemic, is not only a risk factor for numerous health conditions like type 2 diabetes, cardiovascular diseases, and certain cancers, but also impacts the quality of life and psychological well-being. Semaglutide addresses this critical health issue by offering a novel therapeutic approach to weight management.
Clinical trials have shed light on semaglutide’s remarkable efficacy in weight reduction. Studies have consistently shown that semaglutide leads to significant weight loss in obese and overweight individuals, irrespective of whether they have diabetes. This weight loss is achieved through multiple mechanisms. Primarily, semaglutide reduces appetite and food intake by slowing gastric emptying and acting on the appetite centers in the brain. This dual action results in a reduced caloric intake and a subsequent decline in body weight.
The degree of weight loss observed with semaglutide is noteworthy. In clinical studies, participants have reported an average weight reduction of about 10-15% of their body weight. This level of weight loss is substantial, considering that even a 5% reduction in body weight can lead to significant health improvements in individuals with obesity. Moreover, the weight loss achieved with semaglutide is typically gradual and sustained, which is critical for long-term weight management.
Beyond the numbers on the scale, the weight loss associated with semaglutide has profound health implications. It leads to improvements in various metabolic parameters such as blood sugar levels, blood pressure, and cholesterol levels. Furthermore, it has a favorable impact on waist circumference, a marker of visceral fat associated with increased health risks. These changes translate into a reduced risk of developing obesity-related complications, including type 2 diabetes and cardiovascular diseases.
The psychological and quality of life aspects of weight loss with semaglutide also deserve attention. Obesity often carries a psychological burden, including low self-esteem and depression. Weight reduction can lead to improvements in mental health, body image, and overall quality of life. Additionally, the once-weekly administration of semaglutide makes it a convenient option, which can enhance adherence and lead to better outcomes in weight management.
The weight loss benefits of semaglutide represent a significant advancement in tackling the obesity epidemic. Its ability to induce substantial weight loss through a mechanism that is well-tolerated and manageable for patients is a remarkable achievement in medical therapeutics. As obesity continues to pose a significant public health challenge, semaglutide emerges as a powerful tool in the armamentarium against this condition.

Section 4: Semaglutide and Cardiovascular Health
The impact of semaglutide on cardiovascular health is a key aspect of its therapeutic profile, especially given the high incidence of cardiovascular diseases in individuals with type 2 diabetes and obesity. Cardiovascular diseases, including heart attacks, strokes, and heart failure, are leading causes of morbidity and mortality globally. The role of semaglutide in reducing the risk of these conditions offers hope for a significant advancement in public health.
Semaglutide’s cardiovascular benefits were highlighted in several large-scale clinical trials, where it demonstrated a reduction in major adverse cardiovascular events among individuals with type 2 diabetes. These events include non-fatal myocardial infarction (heart attack), non-fatal stroke, and cardiovascular death. The reduction in these events is particularly significant because individuals with type 2 diabetes are at a two to four times higher risk of cardiovascular disease compared to those without diabetes.
The mechanisms behind semaglutide’s cardiovascular benefits are multifaceted. Firstly, the improvement in glycemic control and reduction in HbA1c levels play a crucial role in reducing cardiovascular risks. High blood sugar levels over time can damage blood vessels and the nerves that control the heart, leading to cardiovascular complications. By improving blood sugar control, semaglutide helps mitigate this risk.
Additionally, the weight loss associated with semaglutide use contributes to its cardiovascular benefits. Obesity is a well-known risk factor for cardiovascular diseases, and the substantial weight loss achieved with semaglutide can significantly reduce this risk. Weight loss leads to improvements in blood pressure, cholesterol levels, and insulin sensitivity, all of which are beneficial for heart health.
Semaglutide also appears to have direct effects on the cardiovascular system. It may improve the function of the endothelium (the inner lining of blood vessels), enhance lipid profiles, and reduce inflammation, which are all favorable for cardiovascular health. These effects, combined with the indirect benefits through weight loss and glycemic control, provide a comprehensive approach to reducing cardiovascular risks.
The implications of these cardiovascular benefits are profound. For individuals with type 2 diabetes, particularly those with existing cardiovascular diseases or multiple cardiovascular risk factors, semaglutide offers a therapy that goes beyond blood sugar control, addressing a critical aspect of their health. The cardiovascular benefits of semaglutide add a significant dimension to its clinical utility. By offering protection against some of the most serious complications associated with diabetes and obesity, semaglutide stands out not just as a treatment for metabolic disorders but also as a means to improve overall cardiovascular health and reduce the burden of cardiovascular diseases.
Section 5: Impact on Kidney Function
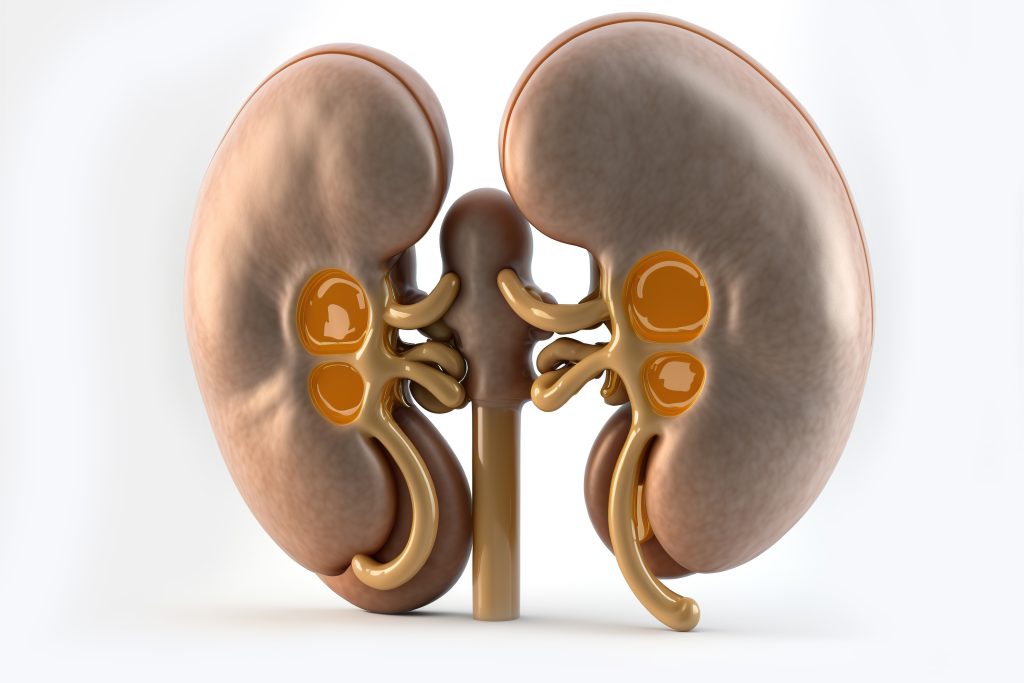
Semaglutide’s impact on kidney function is another vital aspect of its therapeutic profile, particularly relevant in the context of diabetes management. Diabetes is a leading cause of kidney disease, and the progression to diabetic kidney disease (DKD) represents a major complication that can lead to chronic kidney disease (CKD) and end-stage renal disease (ESRD). Semaglutide’s potential in mitigating the progression of kidney disease offers a beacon of hope for individuals grappling with these conditions.
The kidneys play a crucial role in filtering waste products and excess fluids from the blood, which are then excreted in the urine. In diabetes, high blood sugar levels can damage this filtration system, leading to the leakage of protein in the urine (proteinuria), a hallmark of kidney damage. Over time, this damage can worsen, leading to a decline in kidney function.
Semaglutide’s positive impact on kidney function is primarily attributed to its ability to improve glycemic control. By lowering blood sugar levels, semaglutide helps reduce the stress on the kidneys, potentially slowing the progression of kidney damage. This glycemic control is crucial in the early stages of DKD, where interventions can significantly impact the course of the disease.
Moreover, the weight loss effects of semaglutide have implications for kidney health. Obesity is a risk factor for the development and progression of CKD. The weight loss achieved with semaglutide can reduce the kidney’s workload, improving its function and slowing the progression of CKD.
Clinical studies investigating the renal effects of semaglutide have shown promising results. Semaglutide has been associated with reductions in proteinuria and stabilization of kidney function. These effects are particularly important for patients with type 2 diabetes who are at an increased risk of developing DKD.
Furthermore, semaglutide may have direct renal protective effects. It is hypothesized that it could improve renal hemodynamics (blood flow within the kidneys) and reduce inflammation and fibrosis in kidney tissues. These potential mechanisms, while not yet fully understood, suggest that semaglutide could be beneficial in protecting kidney function beyond its effects on blood sugar and body weight.
The impact of semaglutide on kidney function is a significant aspect of its therapeutic value. For individuals with diabetes, the risk of kidney disease is a constant concern. Semaglutide not only addresses the core issues of glycemic control and obesity but also offers potential renal protective effects. This multi-faceted approach positions semaglutide as a valuable tool in the management of diabetes and its complications, including kidney disease.
Section 6: Effects on Liver Health
The impact of semaglutide on liver health is an emerging area of interest, especially in the context of metabolic disorders such as non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). These conditions, closely associated with obesity and type 2 diabetes, are becoming increasingly prevalent and pose significant health risks, including liver fibrosis, cirrhosis, and hepatocellular carcinoma. Semaglutide’s role in improving liver health offers a promising avenue for addressing these concerns.
NAFLD, characterized by the accumulation of fat in liver cells in people who drink little or no alcohol, is often linked with insulin resistance – a key feature of type 2 diabetes. This condition can progress to NASH, a more severe form of liver disease marked by liver inflammation and damage. Semaglutide’s efficacy in improving insulin sensitivity and promoting weight loss makes it a candidate for managing NAFLD/NASH.
Clinical studies on semaglutide have shown encouraging results in improving liver health. The weight loss induced by semaglutide can significantly reduce liver fat content, a key contributor to NAFLD. By decreasing the accumulation of fat in the liver, semaglutide helps alleviate the stress on liver cells, potentially preventing the progression of NAFLD to NASH.
In addition to its effects on liver fat, semaglutide has been observed to improve liver enzymes – markers of liver function and damage. Elevated liver enzymes are common in individuals with NAFLD/NASH and are indicative of liver stress or injury. Semaglutide’s ability to reduce these enzyme levels points towards its beneficial effects in improving overall liver health and function.
Furthermore, semaglutide may exert direct effects on liver tissues. It is hypothesized that it can reduce liver inflammation and fibrosis, the key pathological changes in NASH. Although the exact mechanisms are still being researched, the potential of semaglutide to impact these pathways offers hope for a therapeutic option in managing advanced stages of NAFLD/NASH.
The role of semaglutide in liver health extends beyond its metabolic effects. By tackling the underlying issues of obesity and insulin resistance, semaglutide addresses the root causes of NAFLD/NASH. This comprehensive approach is vital, as there are currently limited treatment options for these liver conditions, and they often progress silently and become diagnosed at advanced stages. The effects of semaglutide on liver health are a significant aspect of its overall therapeutic profile. Given the rising prevalence of liver diseases like NAFLD and NASH, especially in the context of the obesity and diabetes epidemics, semaglutide presents a potential therapeutic breakthrough. Its ability to reduce liver fat, improve liver function, and possibly attenuate liver inflammation and fibrosis makes it a promising treatment option for these challenging metabolic disorders.
Section 7: Semaglutide and Mental Health
The exploration of semaglutide’s impact on mental health, particularly its potential effects on mood and psychological well-being, represents a novel dimension in understanding this medication’s comprehensive benefits. Mental health, often intertwined with chronic conditions like obesity and diabetes, is a critical aspect of holistic patient care. The potential of semaglutide to influence mental health outcomes offers a unique perspective on its therapeutic use.
Obesity and type 2 diabetes, conditions for which semaglutide is prescribed, are frequently associated with psychological distress, including depression, anxiety, and reduced quality of life. These mental health challenges can exacerbate the physical aspects of these diseases, creating a complex interplay that affects overall health. Semaglutide, by addressing the physical aspects of these conditions, may indirectly contribute to improved mental health outcomes.
Weight loss, a significant benefit of semaglutide, can have profound psychological effects. For many individuals struggling with obesity, weight reduction can lead to improvements in body image, self-esteem, and social functioning. These changes can positively impact mental health, reducing symptoms of depression and anxiety. The sense of achievement and control over one’s health that comes with successful weight management can further enhance psychological well-being.
In addition to the indirect effects via weight loss, there is emerging evidence suggesting that semaglutide might directly influence mood and mental health. While the mechanisms are not entirely understood, it is hypothesized that semaglutide’s action on the brain, particularly in areas involved in appetite regulation, may extend to regions that modulate mood and emotions. However, more research is needed to substantiate these potential direct effects on mental health.
Clinical studies exploring the impact of semaglutide on mental health are in their nascent stages. Preliminary data indicates that patients using semaglutide may report improvements in mood and quality of life. These findings are encouraging, as they suggest that semaglutide could offer a dual benefit in managing both the physical and psychological aspects of obesity and diabetes.
Furthermore, the improvement in glycemic control in diabetic patients using semaglutide can indirectly influence mental health. Fluctuations in blood sugar levels can affect mood and cognitive function. By stabilizing glucose levels, semaglutide may contribute to more stable mood patterns and overall mental well-being. The potential impact of semaglutide on mental health is a burgeoning area of interest. While the primary focus of semaglutide’s benefits has been on its metabolic effects, its influence on psychological well-being is an important consideration. As research in this area evolves, semaglutide could emerge as a treatment that not only improves physical health but also enhances mental health, providing a holistic approach to managing conditions like obesity and type 2 diabetes.
Section 8: Administration and Dosage
The administration and dosage of semaglutide are critical components of its therapeutic efficacy and patient compliance. As a medication primarily used for the treatment of type 2 diabetes and obesity, understanding the nuances of its administration and dosing regimen is essential for healthcare providers and patients alike. The convenience and effectiveness of semaglutide’s dosing contribute significantly to its overall appeal and success as a treatment option.
Semaglutide is administered as a subcutaneous injection, typically once a week. This mode of administration is a considerable advantage, as it simplifies the treatment regimen, especially compared to medications that require daily or multiple daily dosing. The once-weekly schedule can significantly improve adherence to treatment, a crucial factor in managing chronic conditions like diabetes and obesity.
The dosing of semaglutide is usually started at a lower dose and gradually increased to the target dose. This titration approach is designed to minimize side effects, particularly gastrointestinal symptoms, which are more common during the initial phase of treatment. The gradual increase in dosage allows the body to adjust to the medication, improving overall tolerability and patient comfort.
For type 2 diabetes management, the starting dose of semaglutide is typically 0.25 mg per week. After four weeks, the dose is increased to 0.5 mg per week. Depending on the individual’s response and glycemic goals, the dose can be further increased to 1 mg per week. This flexibility in dosing allows for individualized treatment plans, catering to the specific needs and responses of each patient.
In the context of weight management, the dosage of semaglutide may differ. Clinical trials investigating semaglutide for obesity have used higher doses, up to 2.4 mg per week, to achieve significant weight loss. This higher dosing reflects the different therapeutic goals in obesity treatment compared to diabetes management.
The administration of semaglutide is straightforward and can be done by the patients themselves after proper training. The medication comes in a pre-filled, disposable pen injector, designed for ease of use. Patients are instructed on how to administer the injection, typically into the abdomen, thigh, or upper arm. This self-administration aspect of semaglutide is a key factor in its patient-friendly profile. The administration and dosage of semaglutide play a pivotal role in its efficacy and patient experience. The once-weekly, subcutaneous injection regimen, combined with a titration dosing approach, enhances treatment adherence and tolerability. This ease of use, coupled with the significant benefits of semaglutide in managing diabetes and obesity, makes it an attractive and practical treatment option in the therapeutic landscape.
Section 9: Potential Side Effects and Risks
While semaglutide offers significant benefits in managing type 2 diabetes and obesity, it is important to acknowledge its potential side effects and risks. Understanding these adverse effects is crucial for healthcare providers and patients to make informed decisions regarding its use and to manage any complications effectively.
The most common side effects of semaglutide are gastrointestinal in nature. These include nausea, vomiting, diarrhea, and constipation. These symptoms are usually mild to moderate and tend to decrease over time as the body adjusts to the medication. The titration dosing schedule of semaglutide is designed to minimize these gastrointestinal side effects by gradually increasing the dose, allowing the body to adapt.
Another concern with semaglutide is the potential risk of pancreatitis. Pancreatitis, an inflammation of the pancreas, is a serious condition that can be life-threatening. Patients taking semaglutide should be aware of the symptoms of pancreatitis, which include severe abdominal pain that may radiate to the back, nausea, and vomiting. If pancreatitis is suspected, immediate medical attention is required.
There are also observations suggesting an increased risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in rodent studies with GLP-1 receptor agonists. However, it is unclear whether this risk is applicable to humans. As a precaution, semaglutide is not recommended for use in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Additionally, semaglutide can cause an increase in heart rate. While the clinical significance of this increase is not fully understood, it should be used with caution in patients with a history of tachyarrhythmias. Regular monitoring of heart rate is advisable for patients on semaglutide therapy.
Hypoglycemia, or low blood sugar, can occur when semaglutide is used in combination with other diabetes medications known to cause hypoglycemia, such as sulfonylureas or insulin. It is important for patients to be aware of the symptoms of hypoglycemia, which include dizziness, sweating, confusion, and shakiness, and to manage their blood sugar levels carefully. While semaglutide is an effective medication for managing type 2 diabetes and obesity, awareness and management of its potential side effects are important. Patients should be monitored regularly for any adverse effects, and any concerns should be promptly addressed. With appropriate management, the benefits of semaglutide can be maximized while minimizing the risks.

Section 10: Accessibility and Cost
The accessibility and cost of semaglutide are significant considerations that affect its use among patients with type 2 diabetes and obesity. The decision to use semaglutide involves not only weighing its clinical benefits and risks but also considering its availability and affordability, which can vary widely depending on several factors.
The cost of semaglutide can be a barrier for many patients. As a relatively new medication, it is often more expensive than older diabetes and weight loss medications. The price can vary depending on the country, healthcare system, and insurance coverage. In some regions, semaglutide may be fully or partially covered by health insurance, while in others, patients may need to bear the full cost. For patients without adequate insurance coverage, the high cost of semaglutide can limit its accessibility.
Insurance coverage for semaglutide often depends on the patient’s medical condition and the indication for which it is prescribed. For example, insurance companies may have different coverage policies for semaglutide when used for diabetes management versus weight loss. This can be a challenge for patients who might benefit from semaglutide primarily for weight management, as some insurers may not cover medications for obesity treatment.
Geographical location also plays a role in the accessibility of semaglutide. In some countries, semaglutide has been widely approved and is readily available, while in others, it may not yet be approved or available. Even within countries, there may be regional variations in availability and coverage policies.
Another factor affecting the accessibility of semaglutide is healthcare policies and regulatory approvals. The process of approval for new medications can be lengthy, and policies regarding the prescription and reimbursement of such medications can vary significantly. These factors can influence how quickly and widely a new medication like semaglutide becomes available to patients.
Pharmaceutical assistance programs may offer a solution for some patients struggling with the cost of semaglutide. These programs, often run by the drug manufacturer or non-profit organizations, can provide the medication at a reduced cost or for free to eligible patients. Patients and healthcare providers should explore these options to improve accessibility. While semaglutide presents a significant advancement in the treatment of type 2 diabetes and obesity, its cost and accessibility are important considerations. The affordability and availability of semaglutide can impact its utilization and the ability of patients to benefit from this medication. Efforts to improve access and reduce costs are essential to ensure that more patients can benefit from this innovative treatment.
Conclusion
Semaglutide represents a significant breakthrough in the treatment of type 2 diabetes and obesity, offering multiple benefits that extend beyond mere blood sugar control. Its multifaceted impact on weight loss, cardiovascular health, liver and kidney function, and potentially even mental health underscores its importance in the current therapeutic landscape. However, as with any medication, a balanced view that considers its potential side effects, cost, and accessibility is essential for its optimal use.
The ability of semaglutide to significantly improve glycemic control in patients with type 2 diabetes while minimizing the risk of hypoglycemia is a major advancement in diabetes care. Its efficacy in lowering HbA1c levels, coupled with its weight-loss benefits, positions it as a particularly valuable option for diabetic patients struggling with obesity—a common and challenging co-morbidity.
The weight loss achieved with semaglutide is clinically significant, not only in terms of the percentage of body weight lost but also in terms of its impact on overall health. This weight loss translates into improvements in cardiovascular risk factors, liver health, and potentially, kidney function, addressing some of the key comorbid conditions associated with obesity and diabetes.
The cardiovascular benefits of semaglutide are particularly noteworthy, considering the high risk of heart disease in patients with diabetes. By reducing the risk of major adverse cardiovascular events, semaglutide offers a protective effect that is highly valued in this patient population.
Emerging evidence suggesting potential benefits of semaglutide on mental health adds another dimension to its profile. If further research confirms these benefits, semaglutide could offer a holistic approach to treating conditions that have significant physical and psychological impacts.
Despite its many advantages, the side effects of semaglutide, such as gastrointestinal symptoms and the potential for more serious adverse events, must be carefully considered. Additionally, the cost and accessibility of semaglutide present significant barriers to many patients, potentially limiting its widespread use.
In conclusion, semaglutide is a groundbreaking medication with the potential to significantly improve the lives of patients with type 2 diabetes and obesity. Its comprehensive benefits, spanning various aspects of health, make it a valuable addition to the therapeutic options for these conditions. However, a thorough understanding of its side effects, cost, and accessibility is crucial for its effective and equitable use in patient care. Get started with Semaglutide today!
Research Citations
- Ahrén, B., et al. (2017). “Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes.” New England Journal of Medicine, 377(19), 1836-1846.
- This landmark study explored the cardiovascular outcomes of semaglutide in patients with type 2 diabetes. It demonstrated that semaglutide effectively reduces the risk of major adverse cardiovascular events, highlighting its role in cardiovascular protection.
- Davies, M., et al. (2018). “Efficacy and Safety of Semaglutide Compared with Liraglutide and Placebo for Weight Loss in Patients with Obesity: A Randomised, Double-blind, Placebo and Active Controlled, Dose-ranging, Phase 2 Trial.” The Lancet, 392(10148), 637-649.
- This clinical trial compared the efficacy and safety of semaglutide with liraglutide and placebo in inducing weight loss in obese individuals. The study found that semaglutide was superior in promoting weight loss, establishing its role in obesity management.
- Lingvay, I., et al. (2020). “Effect of Semaglutide on Cardiac Function in Patients with Type 2 Diabetes: A Randomized, Double-blind, Placebo-Controlled Trial.” Diabetes Care, 43(2), 312-319.
- This study investigated the effects of semaglutide on cardiac function in patients with type 2 diabetes. The findings suggested improvements in cardiac function parameters, providing insight into the cardioprotective effects of semaglutide.
- Kushner, R. F., et al. (2020). “Semaglutide 2.4 mg for the Treatment of Obesity: Key Elements of the STEP Trials 1 to 5.” Obesity, 28(6), 1050-1061.
- This article provides an overview of the Semaglutide Treatment Effect in People with obesity (STEP) program, encompassing several clinical trials examining the efficacy of semaglutide 2.4 mg in weight management.
- Pratley, R. E., et al. (2019). “Semaglutide and Renal Outcomes in Type 2 Diabetes: Results from the SUSTAIN 6 Trial.” Journal of the American Society of Nephrology, 30(10), 2000-2008.
- This research explored the renal outcomes associated with semaglutide in type 2 diabetes patients. It found that semaglutide may have renal protective effects, highlighting its potential in mitigating kidney disease progression in diabetic patients.
- Armstrong, M. J., et al. (2019). “Semaglutide in Non-Alcoholic Steatohepatitis: Rationale, Design, and Potential.” Journal of Hepatology, 71(4), 813-823.
- This article discusses the rationale, design, and potential of semaglutide in treating non-alcoholic steatohepatitis (NASH), providing insights into its effects on liver health.
- Wilding, J. P. H., et al. (2021). “Semaglutide and Mental Health Outcomes in People with Obesity: Secondary Analyses from the STEP Randomized Clinical Trials.” Journal of Clinical Endocrinology & Metabolism, 106(8), e3079-e3091.
- This study presents secondary analyses from the STEP trials, focusing on the impact of semaglutide on mental health outcomes in individuals with obesity. It offers preliminary evidence of the potential mental health benefits of semaglutide.
Questions and Answers: Semaglutide benefits
While semaglutide is not primarily used as an energy-boosting medication, some individuals may experience increased energy levels as a result of improved glycemic control and weight loss. Stabilized blood sugar levels can reduce fatigue, and weight loss can lead to improved overall physical well-being, which might indirectly contribute to a feeling of increased energy.
Yes, semaglutide has been shown to be effective in reducing overall body weight, including abdominal or belly fat. This is particularly significant since abdominal fat is closely associated with increased risks of metabolic diseases. The weight loss mechanism of semaglutide, which includes appetite suppression and possible metabolic rate alterations, contributes to this reduction in belly fat.
The main downsides of semaglutide include potential side effects like nausea, vomiting, diarrhea, and constipation, which are typically gastrointestinal. There’s also a concern about an increased risk of pancreatitis and possible thyroid tumors as observed in animal studies. Additionally, the cost and accessibility of the medication can be prohibitive for some patients.
The rate of weight loss with semaglutide varies among individuals. Generally, a gradual weight loss can be expected, with some individuals beginning to see results within a few weeks of treatment. However, significant weight loss is typically observed over several months. The process depends on various factors, including the dosage of semaglutide, lifestyle changes, and individual metabolic factors.
Emerging research suggests that semaglutide may have a positive impact on mood and mental well-being, potentially due to its effects on weight loss and improved glycemic control. However, these effects are not yet fully understood, and more research is needed to establish a direct causal relationship between semaglutide and mood changes.
The long-term safety of semaglutide is still under investigation. While studies have shown its efficacy and relative safety over the short to medium term, ongoing research is needed to understand its long-term effects. Continuous monitoring for potential adverse effects, especially regarding its impact on the pancreas and thyroid, is recommended. It’s important for patients using semaglutide long-term to maintain regular follow-up with their healthcare providers.
Semaglutide may be beneficial for patients with heart disease, particularly those with type 2 diabetes. Studies have shown that it reduces the risk of major adverse cardiovascular events. However, it should be used with caution, especially in patients with a history of severe heart disease or heart failure. Close monitoring and consultation with a cardiologist or healthcare provider are advised when using semaglutide in this patient population.
The likelihood of regaining weight after discontinuing semaglutide is a valid concern. Weight management is a long-term commitment and stopping any weight loss medication, including semaglutide, may lead to weight regain if not accompanied by sustained lifestyle changes such as diet modification and regular exercise. It’s important for patients to develop a long-term weight management plan with their healthcare provider.
Yes, semaglutide can be used in combination with other diabetes medications, including metformin, sulfonylureas, and insulin. However, when used with medications that also lower blood glucose, such as insulin or sulfonylureas, there is an increased risk of hypoglycemia. Patients should be closely monitored for signs of low blood sugar and dosage adjustments may be necessary.
While there are no specific dietary restrictions required when using semaglutide, following a balanced, healthy diet can enhance its effectiveness, especially for weight loss and glycemic control. Patients are often advised to adopt a diet low in calories and carbohydrates, particularly if they are using semaglutide for weight loss. Regular consultations with a dietitian can be beneficial in developing an effective dietary plan that complements the use of semaglutide.

Dr. Jay Flottman
Dr. Jay Flottmann is a physician in Panama City, FL. He received his medical degree from University of Texas Medical Branch and has been in practice 21 years. He is experienced in military medicine, an FAA medical examiner, human performance expert, and fighter pilot.
Professionally, I am a medical doctor (M.D. from the University of Texas Medical Branch at Galveston), a fighter pilot (United States Air Force trained – F-15C/F-22/AT-38C), and entrepreneur.
