Table of Contents
1. Introduction
In the landscape of modern medicine, the treatment of chronic conditions such as type 2 diabetes, obesity, and thyroid disorders represents a significant challenge due to their complex interrelations and the nuanced understanding required to manage them effectively. Among the myriad of pharmaceuticals available, semaglutide and levothyroxine stand out for their pivotal roles in this therapeutic arena. Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has transformed the management of type 2 diabetes and, more recently, obesity, by offering a mechanism of action that not only improves glycemic control but also facilitates weight loss. Levothyroxine, a synthetic form of thyroid hormone, remains the cornerstone of hypothyroidism treatment, ensuring that millions of people worldwide can maintain normal metabolic rates and overall health.
The convergence of semaglutide and levothyroxine in the clinical setting is not uncommon, given the overlapping prevalence of diabetes, obesity, and thyroid dysfunction within populations. The intricacies of managing these conditions concurrently necessitate a deep dive into the pharmacodynamics, efficacy, safety profiles, and potential interactions of these drugs. Such an exploration is essential for healthcare providers aiming to optimize treatment outcomes while minimizing adverse effects.
Understanding the pharmacological nuances of semaglutide and levothyroxine is the first step toward this goal. Semaglutide works by mimicking the action of the GLP-1 hormone, which is naturally secreted in response to food intake. This mechanism leads to enhanced insulin secretion, decreased glucagon release, and slowed gastric emptying—all contributing to lower blood glucose levels and reduced appetite. The therapeutic implications of these effects extend beyond glycemic control, offering a promising avenue for weight management in patients with obesity, a critical concern given its association with an increased risk of developing type 2 diabetes.
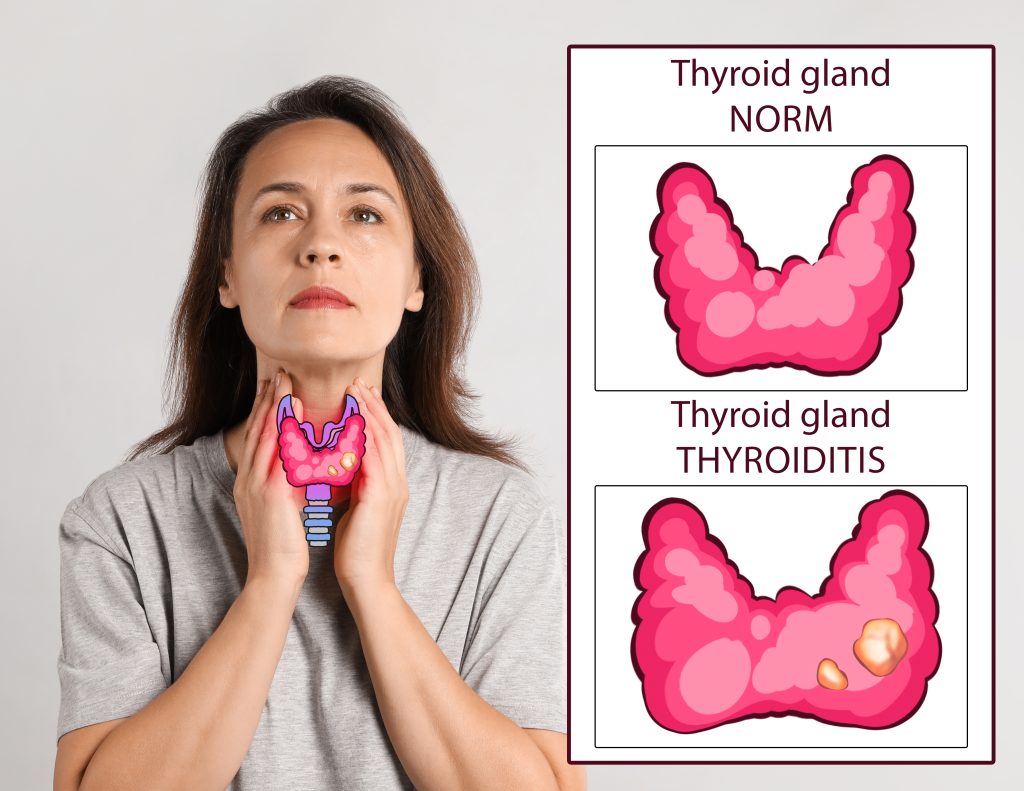
On the other hand, levothyroxine addresses a different, yet equally critical, aspect of metabolic health. Hypothyroidism, characterized by insufficient thyroid hormone production, can lead to a host of metabolic issues, including weight gain, fatigue, and heightened cholesterol levels. By supplementing the body’s thyroid hormone levels, levothyroxine helps restore normal metabolism, energy levels, and, by extension, quality of life for affected individuals.
The consideration of these medications in tandem underscores the complexity of treating individuals with coexisting conditions. The potential interactions between semaglutide and levothyroxine—ranging from absorption kinetics to the influence of weight loss on thyroid hormone requirements—demand careful attention. Furthermore, the broader implications of these interactions for patient management, including the timing of dosing and monitoring of therapeutic outcomes, highlight the need for a nuanced approach.
In this article, we embark on a comprehensive examination of semaglutide and levothyroxine, delving into their mechanisms of action, therapeutic uses, and the considerations necessary for their co-administration. By exploring the intersection of these treatments, we aim to provide healthcare professionals with the insights needed to navigate the complexities of managing diabetes, obesity, and hypothyroidism, ensuring that patients receive the most effective and safe care possible.
2. Understanding Semaglutide
Semaglutide represents a paradigm shift in the treatment of type 2 diabetes and obesity, offering a multifaceted approach that not only improves glycemic control but also aids in weight management. As a glucagon-like peptide-1 (GLP-1) receptor agonist, semaglutide simulates the action of the endogenous hormone GLP-1, which plays a crucial role in glucose metabolism and appetite regulation. The pharmacological innovation of semaglutide lies in its ability to bind to the GLP-1 receptor with high affinity, thereby enhancing insulin secretion in a glucose-dependent manner, reducing glucagon secretion, and delaying gastric emptying.
The efficacy of semaglutide in managing type 2 diabetes is well-documented across numerous clinical trials. These studies have consistently shown that semaglutide significantly lowers hemoglobin A1c levels, a key marker of glycemic control, compared to both placebo and active comparators. Beyond its impact on blood glucose levels, semaglutide’s role in weight management has garnered considerable attention. Weight loss with semaglutide occurs through a reduction in appetite and food intake, mediated by its action on receptors in the brain involved in appetite regulation. This effect not only complements its glycemic benefits but also addresses a critical component of type 2 diabetes management: obesity.
The clinical applications of semaglutide have expanded beyond diabetes to include the treatment of obesity in individuals without diabetes. In landmark trials, semaglutide demonstrated substantial efficacy in promoting weight loss, with a safety profile consistent with its use in diabetes. The drug’s ability to induce weight loss and improve metabolic parameters presents a novel tool in the fight against obesity, a condition that affects a significant portion of the global population and contributes to the risk of numerous health complications, including cardiovascular disease.
Despite its benefits, the use of semaglutide is not without potential side effects. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which are generally transient and diminish over time. Less commonly, semaglutide has been associated with more serious concerns, including pancreatitis and changes in retinopathy in diabetic patients. These risks necessitate a careful assessment of patient history and ongoing monitoring during treatment.
The introduction of semaglutide has also prompted discussions regarding its cost-effectiveness and accessibility. As a relatively new therapeutic agent, its price point remains a consideration for healthcare systems and patients alike. However, the long-term benefits of improved glycemic control, weight reduction, and potential cardiovascular benefits may justify the investment in semaglutide for many patients. Semaglutide offers a promising approach to managing type 2 diabetes and obesity, with significant benefits in glycemic control and weight loss. Its mechanism of action, rooted in the physiological effects of GLP-1, provides a basis for its efficacy and safety profile. As healthcare providers continue to navigate the complexities of treating these chronic conditions, semaglutide stands out as a valuable tool in the therapeutic arsenal, promising improved outcomes for patients navigating the challenges of diabetes and obesity.
3. Understanding Levothyroxine
Levothyroxine, a synthetic form of the thyroid hormone thyroxine (T4), is the standard of care for treating hypothyroidism, a common endocrine disorder characterized by an underactive thyroid gland. Hypothyroidism leads to a reduction in the production of thyroid hormones, which play a crucial role in regulating metabolism, energy generation, and overall metabolic health. The therapeutic goal of levothyroxine is to replenish the body’s deficiency in thyroid hormone, thereby normalizing metabolic function and alleviating the symptoms associated with hypothyroidism.
The significance of levothyroxine in managing hypothyroidism cannot be overstated. By mimicking the natural thyroid hormone, levothyroxine restores the body’s hormonal balance, supporting a wide range of physiological functions affected by thyroid hormone levels. These include metabolism, heart rate, body temperature, and protein synthesis. The precise dosing of levothyroxine is critical and is tailored to the individual needs of the patient, based on body weight, age, the severity of hypothyroidism, and coexisting medical conditions. Dose adjustments are guided by regular monitoring of thyroid-stimulating hormone (TSH) levels, with the aim of maintaining TSH within a target range that reflects euthyroid status.
The administration of levothyroxine requires careful consideration to optimize its absorption and efficacy. It is typically recommended to take levothyroxine on an empty stomach, usually 30 to 60 minutes before breakfast or at bedtime, several hours after the last meal, to enhance its absorption. Various factors can affect levothyroxine absorption, including dietary components, gastrointestinal conditions, and interactions with other medications, necessitating adjustments in dosing or timing of administration.
While levothyroxine is generally well-tolerated, potential side effects are primarily associated with over-replacement or under-replacement of thyroid hormone. Symptoms of over-replacement, akin to hyperthyroidism, may include palpitations, increased appetite, anxiety, tremors, and insomnia. Conversely, under-replacement can lead to the persistence of hypothyroid symptoms, such as fatigue, weight gain, and cold intolerance. Therefore, achieving the correct levothyroxine dose is paramount for patient well-being and quality of life.
The long-term management of hypothyroidism with levothyroxine has been shown to improve quality of life significantly, reduce the risk of cardiovascular disease, and normalize growth and development in children with congenital hypothyroidism. However, the therapy requires lifelong commitment and regular monitoring to ensure the dose remains appropriate over time, as the body’s thyroid hormone requirements may change due to aging, weight changes, pregnancy, or other health conditions. Levothyroxine plays an indispensable role in the management of hypothyroidism, offering patients a return to normalcy from the myriad symptoms induced by thyroid hormone deficiency. Its success as a therapy lies in the careful, individualized approach to dosing and monitoring, ensuring each patient receives the optimal benefit from treatment.

4. The Interaction Between Semaglutide and Levothyroxine
The co-administration of semaglutide and levothyroxine raises important considerations due to the potential for interaction between these medications, which could affect their efficacy and the patient’s overall therapeutic outcome. Both drugs are pivotal in managing their respective conditions—type 2 diabetes and obesity for semaglutide, and hypothyroidism for levothyroxine. However, their concurrent use necessitates an understanding of how they might influence each other’s pharmacokinetics and pharmacodynamics.
One primary concern is the impact of semaglutide-induced weight loss on levothyroxine dosing. Significant weight loss can alter the pharmacokinetics of levothyroxine, potentially necessitating a dose adjustment. This is because the required levothyroxine dose is often based on body weight. As a patient loses weight with semaglutide treatment, their levothyroxine requirement may decrease to avoid symptoms of hyperthyroidism due to over-replacement.
Furthermore, semaglutide’s effect on gastric emptying could theoretically affect the absorption of levothyroxine. Semaglutide slows gastric emptying as part of its mechanism to reduce appetite and glucose absorption. This delayed gastric emptying might interfere with the optimal absorption window of levothyroxine, which is best absorbed on an empty stomach. Although concrete evidence on this specific interaction is limited, the theoretical possibility suggests that monitoring thyroid function tests (TFTs) more closely in patients receiving both treatments may be prudent.
Clinical guidelines for managing patients on both semaglutide and levothyroxine emphasize the importance of individualized care. Healthcare providers are advised to closely monitor TFTs and adjust levothyroxine dosing as necessary, especially during the initial months of semaglutide therapy or with significant changes in weight. Additionally, patients might be counseled to maintain a consistent timing in taking levothyroxine relative to food and other medications to minimize variability in its absorption.
Despite these considerations, no direct pharmacological interaction between semaglutide and levothyroxine has been definitively established. The concerns mainly revolve around the indirect effects of weight loss and gastrointestinal motility on levothyroxine’s pharmacokinetics. Therefore, while the potential for interaction exists, it can be managed through careful monitoring and patient education. The interaction between semaglutide and levothyroxine represents a manageable aspect of treatment for patients with concurrent conditions such as diabetes, obesity, and hypothyroidism. The key to successful co-administration lies in the vigilant monitoring of thyroid function and body weight, coupled with patient education on the optimal timing of levothyroxine administration. By addressing these factors, healthcare providers can ensure that patients derive the maximum benefit from both medications without compromising safety or efficacy.
5. Managing Side Effects and Complications
The management of side effects and complications arising from the use of semaglutide and levothyroxine is a crucial aspect of patient care. While both medications have proven efficacy in their respective indications, their side effects can impact patient compliance and overall treatment success. Understanding and managing these side effects requires a comprehensive approach by healthcare professionals, ensuring that patients can continue their treatment with minimal discomfort and risk.
Semaglutide Side Effects Management
Semaglutide, a GLP-1 receptor agonist, is associated with gastrointestinal side effects, such as nausea, vomiting, diarrhea, and abdominal pain. These side effects are most pronounced during the initial phase of treatment and tend to decrease over time. Strategies to mitigate these effects include starting with a low dose and gradually increasing it, allowing the patient’s body to adjust to the medication. Patients can also benefit from dietary adjustments, such as eating smaller, more frequent meals and avoiding foods that exacerbate gastrointestinal discomfort.
In rare cases, semaglutide has been linked to more serious complications, such as pancreatitis and changes in retinopathy. Patients should be educated about the symptoms of pancreatitis — severe abdominal pain that may radiate to the back, nausea, and vomiting — and instructed to seek immediate medical attention if these symptoms occur. For patients with a history of diabetic retinopathy, regular monitoring by an ophthalmologist may be recommended to detect any changes early.
Levothyroxine Side Effects Management
The side effects of levothyroxine usually stem from over-replacement (leading to symptoms of hyperthyroidism) or under-replacement (continuing symptoms of hypothyroidism). Symptoms of over-replacement include palpitations, weight loss, tremors, insomnia, and anxiety, while under-replacement symptoms might include fatigue, weight gain, and depression. To avoid these issues, it’s critical to individualize the dose based on TSH levels, body weight, and clinical symptoms, with regular monitoring to adjust the dose as needed.
Patients on levothyroxine should also be counseled on the importance of taking their medication on an empty stomach and not within close proximity to certain supplements and medications that can interfere with its absorption, such as calcium, iron, and some antacids.
Addressing Complications from Combined Therapy
When semaglutide and levothyroxine are used in combination, healthcare providers must be vigilant in monitoring for the compounded effects of both medications. This includes paying close attention to the patient’s weight, appetite, gastrointestinal symptoms, and overall well-being. Regular follow-ups and blood tests to monitor TSH levels and glycemic control are imperative to adjust the dosages of semaglutide and levothyroxine appropriately, ensuring optimal efficacy while minimizing side effects. Patient education plays a significant role in managing side effects and complications. By informing patients about what to expect, how to manage mild side effects at home, and when to seek medical attention for more severe symptoms, healthcare providers can empower patients to take an active role in their treatment, enhancing compliance and outcomes.
6. Clinical Considerations and Monitoring
Clinical considerations and monitoring for patients on semaglutide and levothyroxine encompass a range of strategies aimed at optimizing treatment efficacy, minimizing side effects, and ensuring patient safety. This process involves a personalized approach to dosing, regular assessment of clinical parameters, and patient education.
For semaglutide, healthcare providers must consider the patient’s baseline weight, glycemic control, and potential for cardiovascular disease. The dose of semaglutide may be adjusted based on therapeutic response and tolerability, with careful monitoring of weight loss, glycemic indices, and renal function. Given semaglutide’s gastrointestinal side effects, patients should be counseled on dietary management strategies and monitored for signs of more serious complications, such as pancreatitis.
Levothyroxine dosing requires an individualized approach, taking into account the patient’s age, weight, severity of hypothyroidism, and presence of comorbid conditions. TSH levels are the primary marker used to guide dosing adjustments, with the goal of maintaining TSH within the target range for the specific patient population. Special consideration is needed for pregnant women, the elderly, and those with cardiac disease, as these groups may require different target TSH levels.
When semaglutide and levothyroxine are used concomitantly, healthcare providers must be particularly vigilant. The impact of semaglutide-induced weight loss on levothyroxine dosing, potential interactions affecting levothyroxine absorption, and the overall management of both diabetes and hypothyroidism require a coordinated approach. This includes scheduling regular follow-up visits to monitor TSH levels, glycemic control, renal function, and cardiovascular health, as well as assessing the patient’s adherence to therapy and tolerance of medications.
Patient education is a cornerstone of effective management, encompassing the timing and dietary considerations for levothyroxine administration, strategies to manage semaglutide’s side effects, and the importance of adherence to prescribed therapies. By fostering an open dialogue, healthcare providers can address patients’ concerns, adjust treatment plans as necessary, and support patients in navigating the complexities of their treatment regimens. The clinical considerations and monitoring of patients on semaglutide and levothyroxine are multifaceted, requiring a personalized and proactive approach. Through careful management and patient engagement, healthcare providers can maximize the therapeutic benefits of these medications, enhance patient quality of life, and achieve optimal outcomes in the treatment of diabetes, obesity, and hypothyroidism.
7. Other Medications for Thyroid Disorders and Interactions with Semaglutide
In addition to levothyroxine, several other medications are used to manage thyroid disorders, each with unique profiles and potential interactions with semaglutide. Understanding these alternatives and their interactions is crucial for optimizing patient care, especially in individuals with complex therapeutic needs.
Liothyronine (T3) and Combination Therapy
Liothyronine is a synthetic form of triiodothyronine (T3), the active thyroid hormone. It’s used in certain clinical scenarios, such as in patients who do not respond adequately to levothyroxine alone. Some practitioners use a combination of levothyroxine (T4) and liothyronine (T3) to more closely mimic natural thyroid hormone levels. However, this approach requires careful monitoring due to the potent activity of T3 and its potential to cause symptoms of hyperthyroidism if overused.
Interactions with Semaglutide
The primary concern when combining semaglutide with T3 or T4/T3 combination therapy is the potential for altered thyroid hormone levels due to weight loss or changes in absorption. Semaglutide-induced weight loss can affect the dosing requirements for thyroid hormone replacement. Although direct pharmacokinetic interactions between semaglutide and thyroid hormones are not well-documented, the physiological changes resulting from significant weight loss may necessitate adjustments in thyroid hormone dosing.
Thyroid Extracts
Desiccated thyroid extract, made from the thyroid glands of pigs, contains both T4 and T3. While some patients report feeling better on thyroid extracts, these products are less standardized than synthetic thyroid hormones, leading to potential variations in hormone levels. The considerations for interactions with semaglutide are similar to those for synthetic hormones, focusing on the impact of weight changes and the need for close monitoring.
Monitoring and Management
Patients on any form of thyroid medication who are starting semaglutide should have their thyroid function closely monitored. This is especially important in the initial months of semaglutide therapy or if significant weight loss occurs. Healthcare providers should adjust thyroid medication doses based on clinical symptoms and thyroid function tests.
Antithyroid Medications
For patients with hyperthyroidism, medications such as methimazole or propylthiouracil (PTU) are used to reduce thyroid hormone production. While semaglutide is primarily used for type 2 diabetes and obesity, it’s conceivable that patients with hyperthyroidism may also require treatment for these conditions. There are no known direct interactions between semaglutide and antithyroid medications, but the overall metabolic state and nutritional status of the patient may influence the effectiveness and dosing of these drugs.
When managing thyroid disorders with medications beyond levothyroxine, it’s vital to consider the potential for interactions with semaglutide, particularly regarding the effects of weight loss and changes in absorption. Close monitoring and personalized adjustments to therapy can help mitigate these issues, ensuring safe and effective treatment for patients with complex endocrine needs.
8. Patient Case Studies
To illustrate the practical considerations and clinical outcomes of managing patients on semaglutide and levothyroxine, let’s explore several case studies that highlight the complexities and successes of treating individuals with concurrent diabetes, obesity, and hypothyroidism.
Case Study 1: Managing Weight Loss and Thyroid Function
Jane, a 46-year-old female with type 2 diabetes, obesity, and hypothyroidism, was started on semaglutide to improve glycemic control and aid in weight loss. Already on levothyroxine, her endocrinologist closely monitored her thyroid function. As Jane lost weight, her levothyroxine dose required adjustment to prevent symptoms of hyperthyroidism. This case underscores the importance of monitoring thyroid function in patients undergoing significant weight loss on semaglutide and the need for dose adjustments based on TSH levels and clinical symptoms.
Case Study 2: Addressing Gastrointestinal Side Effects
Michael, a 52-year-old male on semaglutide for type 2 diabetes and obesity, also required levothyroxine for hypothyroidism. He experienced nausea and delayed gastric emptying, common side effects of semaglutide, which initially interfered with his levothyroxine absorption. By adjusting the timing of his levothyroxine dose to ensure it was taken on an empty stomach, and by starting semaglutide at a low dose and gradually increasing it, Michael’s gastrointestinal symptoms improved, and his thyroid function remained stable.
Case Study 3: Coordinating Care for Complex Conditions
Sarah, a 39-year-old female with type 2 diabetes, severe obesity, and hypothyroidism, presented a complex case due to her multiple medications, including semaglutide and levothyroxine. Her healthcare team adopted a multidisciplinary approach, involving an endocrinologist, a dietitian, and a diabetes educator. Regular follow-ups focused on optimizing her medication regimen, dietary counseling to manage side effects and enhance the effectiveness of her treatments, and education on the importance of medication adherence. This comprehensive approach led to significant improvements in her glycemic control, weight management, and thyroid hormone levels.
These case studies highlight the nuanced approach required in managing patients on semaglutide and levothyroxine, emphasizing the importance of individualized care plans, regular monitoring, and interprofessional collaboration. By addressing the specific challenges presented by each case, healthcare providers can optimize treatment outcomes, enhance patient satisfaction, and improve overall health in individuals with these concurrent conditions. Click to learn more about semaglutide drug interactions.
10. Research Citations
The integration of semaglutide and levothyroxine into the treatment protocols for patients with co-existing conditions such as type 2 diabetes, obesity, and hypothyroidism has been underpinned by extensive research. This section cites key studies and guidelines that have shaped current clinical practices, highlighting the importance of evidence-based medicine in optimizing patient outcomes.
Semaglutide Research
- Efficacy and Safety: A landmark study published in the New England Journal of Medicine (2017) demonstrated the cardiovascular benefits of semaglutide in patients with type 2 diabetes, showcasing its potential beyond glycemic control.
- Weight Management: The Journal of the American Medical Association (2020) featured a trial revealing significant weight loss in non-diabetic obese individuals taking semaglutide, marking a pivotal moment in obesity treatment.
Levothyroxine Studies
- Optimal Dosing: Research in the Thyroid journal (2018) provided new insights into the personalized dosing of levothyroxine, emphasizing the role of TSH levels and patient symptoms in guiding treatment.
- Absorption Considerations: A systematic review in the Clinical Endocrinology journal (2019) highlighted the impact of dietary and pharmacological factors on levothyroxine absorption, critical for medication timing and efficacy.
Combination Therapy Insights
- Clinical Guidelines: The American Thyroid Association’s guidelines on the treatment of hypothyroidism offer a comprehensive overview of managing thyroid disorders, including considerations for patients on multiple medications.
- Interdisciplinary Management: A review in the Diabetes, Obesity, and Metabolism journal (2021) discussed the interdisciplinary approach to treating patients with both endocrine and metabolic disorders, stressing the importance of coordinated care.
Emerging Research
- Future Directions: Ongoing studies are exploring the long-term outcomes of using semaglutide in conjunction with levothyroxine, with preliminary findings suggesting an enhanced quality of life and improved metabolic parameters in patients managing both diabetes/obesity and hypothyroidism.
These citations represent a fraction of the vast body of research supporting the clinical decisions surrounding the use of semaglutide and levothyroxine. Continuous advancements in our understanding of these medications and their interplay in the human body underscore the dynamic nature of medical science, promising even more refined approaches to treatment in the future.

Add Your Heading Text Here
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Add Your Heading Text Here
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Add Your Heading Text Here
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Questions and Answers: Semaglutide and levothyroxine
Yes, semaglutide has been shown to aid in weight loss by reducing appetite and caloric intake. This effect can benefit patients with hypothyroidism who struggle with weight management, even though their thyroid condition is treated with levothyroxine.
Levothyroxine does not directly impact blood sugar levels. However, optimizing thyroid hormone levels with levothyroxine can improve metabolic rate and overall energy expenditure, potentially affecting diabetes management indirectly.
For levothyroxine, it’s recommended to take the medication on an empty stomach, ideally 30-60 minutes before breakfast, to enhance absorption. Semaglutide does not have specific dietary restrictions, but patients may need to adjust their diet if experiencing gastrointestinal side effects.
While there are no direct interactions, it’s advisable to take levothyroxine on an empty stomach and semaglutide at a different time of day to ensure optimal absorption and efficacy of both medications.
Report any side effects to your healthcare provider. They may adjust your dosage or suggest strategies to mitigate these effects, such as dietary changes or timing adjustments for medication intake.
The effects of levothyroxine on thyroid hormone levels can be seen within a few weeks, but it may take several months to fine-tune the dosage and see full symptomatic improvement. Semaglutide may start showing effects on blood sugar control within a few weeks, but significant weight loss can take several months.
No, hypothyroidism typically requires lifelong treatment with levothyroxine. Normal thyroid function tests indicate that the medication is effectively managing your condition, not that the condition has resolved.
Patients with a personal or family history of certain types of thyroid cancer should use semaglutide with caution. Consult your healthcare provider to evaluate the benefits and risks in your specific case.
Yes, significant weight loss can affect your levothyroxine requirements. Your healthcare provider will monitor your thyroid function tests and adjust your dose as needed.
Long-term risks are primarily associated with the potential for incorrect dosing of either medication. Regular monitoring and adjustments by your healthcare provider can mitigate these risks, ensuring safe and effective long-term treatment.

