Table of Contents
Introduction
Semaglutide has swiftly become a leading treatment for type 2 diabetes due to its impressive ability to control blood sugar levels. However, its benefits might extend even further, potentially influencing heart rate regulation. To grasp this novel connection, it’s essential to understand semaglutide’s fundamentals, the importance of heart rate control, and why researchers are excited about its broader benefits.
Semaglutide is a GLP-1 receptor agonist, mimicking the hormone glucagon-like peptide-1. This hormone is vital for blood sugar management, stimulating insulin secretion post-meal and thereby lowering glucose levels. GLP-1 receptor agonists effectively reduce hemoglobin A1c levels, a key indicator of long-term blood sugar control. Additionally, they curb appetite and promote weight loss, further aiding type 2 diabetes management.
Beyond blood sugar management, semaglutide’s impact on the cardiovascular system has piqued research interest. Type 2 diabetes patients often face heightened cardiovascular risks due to high blood sugar, obesity, and hypertension. Thus, understanding how semaglutide affects heart health is crucial.
Heart rate is a critical component of cardiovascular health. A high resting heart rate can indicate an overactive sympathetic nervous system, straining the heart and leading to potential cardiac issues. Conversely, a lower resting heart rate signifies good cardiovascular health and balanced autonomic nervous system function. Many medications impact heart rate, and understanding these effects is vital for patient safety.
Recent studies suggest semaglutide may slightly elevate heart rate. While this increase could signal issues for some patients, it might not always be harmful. The rise in heart rate may be linked to semaglutide’s effects on the autonomic nervous system. More research is needed to distinguish between benign and concerning heart rate changes.
Semaglutide’s potential cardiovascular benefits extend beyond glycemic control. The SUSTAIN-6 trial indicated a reduction in major adverse cardiovascular events (MACE), such as heart attacks and strokes, among semaglutide users. These findings suggest semaglutide could be a valuable option for those seeking cardiovascular protection alongside diabetes management.
Exploring semaglutide’s effects on heart rate involves reviewing the latest clinical research to understand how and why these changes occur. Determining whether these alterations are harmless or require monitoring will shape future treatment strategies. Ultimately, recognizing semaglutide’s broader cardiovascular role will help clinicians make better-informed decisions for patients at risk of heart disease. This article will detail semaglutide’s mechanisms, its heart rate impact, and the implications for patient safety, providing clear answers to frequently asked questions and guiding healthcare providers and patients in making informed choices.
Semaglutide - Mechanism of Action
Semaglutide, a GLP-1 receptor agonist, mimics the natural glucagon-like peptide-1 (GLP-1) hormone released in the gut after eating. This hormone helps regulate blood sugar by stimulating insulin secretion and reducing glucagon, a hormone that raises blood sugar. Additionally, GLP-1 slows digestion and enhances satiety.
Semaglutide effectively lowers blood sugar levels in type 2 diabetes patients by:
- Increasing insulin secretion.
- Reducing glucagon levels.
- Delaying gastric emptying to prevent post-meal blood sugar spikes.
- Acting on the brain to curb appetite, promoting weight loss.
Impact on Glucose Metabolism and Cardiovascular Health
Beyond lowering blood sugar, semaglutide improves overall glucose metabolism, reducing complications like nerve damage, kidney issues, and vision problems. Clinical trials such as SUSTAIN-6 and PIONEER-6 have demonstrated that semaglutide significantly reduces major adverse cardiovascular events (MACE), including heart attacks and strokes, in type 2 diabetes patients.
Cardiovascular Benefits:
- Weight loss and better glucose control lower the cardiovascular burden.
- Improved blood pressure and reduced inflammation decrease heart disease risk.
- Direct effects on heart cells and blood vessels enhance blood flow and reduce inflammation.
Semaglutide, by mimicking the natural GLP-1 hormone, not only manages blood sugar but also enhances cardiovascular health. Its comprehensive benefits in glucose metabolism, weight loss, and cardiovascular protection make it a powerful tool in diabetes management. Recognizing these broader impacts emphasizes its value beyond just glycemic control, offering significant heart and vascular protection.
Understanding Heart Rate Regulation
Heart rate is a vital sign reflecting cardiovascular health. To comprehend semaglutide’s impact on heart rate, it’s crucial to understand heart rate control and its link to blood sugar levels.
The Autonomic Nervous System (ANS)
The ANS regulates heart rate through two branches:
- Sympathetic Nervous System (SNS): Known as the “fight or flight” system, it responds to stress by releasing adrenaline, which increases heart rate and contraction force, delivering more oxygen and nutrients to tissues.
- Parasympathetic Nervous System (PNS): Called the “rest and digest” system, it slows the heart rate by releasing acetylcholine, maintaining a normal heart rate at rest.
These systems balance each other to match heart rate to the body’s needs, increasing it during exercise and slowing it during rest.
Glycemic Control’s Impact on Heart Rate
Stable blood sugar levels are crucial for heart rate regulation. Poor glycemic control affects heart rate through:
- Insulin Resistance and SNS Overactivity: In type 2 diabetes, insulin resistance raises blood sugar and increases SNS activity, leading to a higher resting heart rate and hypertension.
- Hypoglycemia and Heart Rate: Low blood sugar triggers adrenaline release, increasing heart rate and causing palpitations or irregular heartbeat.
- Autonomic Neuropathy: Chronic high blood sugar damages ANS nerves, disrupting heart rate regulation. This results in a heart rate that doesn’t vary appropriately with activity or causes unexplained rapid heart rates.
Understanding these mechanisms highlights how semaglutide, by improving glycemic control, can influence heart rate regulation. Effective blood sugar management through medications like semaglutide helps maintain the ANS balance, ensuring the heart beats appropriately for every situation. By addressing insulin resistance, preventing hypoglycemia, and reducing nerve damage, semaglutide supports better cardiovascular health.
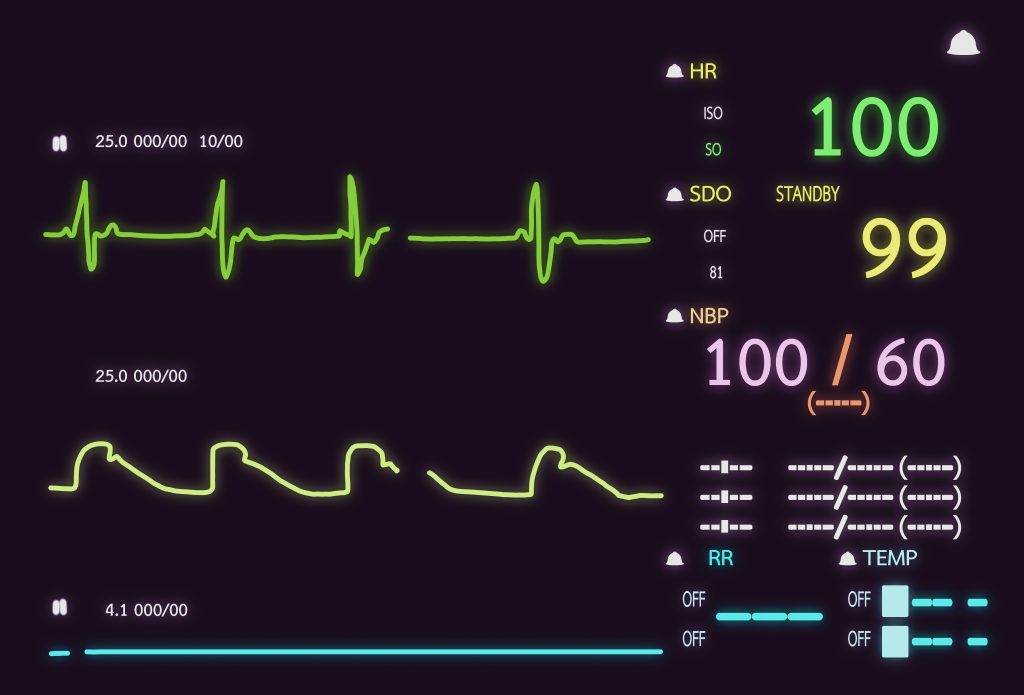
Impact of Semaglutide on Heart Rate
Semaglutide, primarily known for controlling blood sugar, also affects heart rate. This is crucial for patients with diabetes or obesity, who often face additional heart risks. Here, we delve into clinical studies and mechanisms underlying semaglutide’s influence on heart rate.
Clinical Evidence of Heart Rate Changes
SUSTAIN Trials: These trials found semaglutide increased resting heart rate by 2-5 beats per minute across various populations compared to placebo or other diabetes medications.
PIONEER Trials: Focused on oral semaglutide, these studies confirmed similar heart rate increases regardless of age, gender, or baseline cardiovascular status.
Mechanisms Behind Heart Rate Changes
- GLP-1 Receptor Agonist Effect: Semaglutide activates GLP-1 receptors in the heart and nervous system, increasing sympathetic nervous system activity and heart rate.
- Weight Loss Effects: Semaglutide induces significant weight loss, leading to metabolic adjustments that can temporarily raise heart rate.
- Blood Pressure Influence: By lowering blood pressure, semaglutide triggers baroreceptors to increase heart rate to maintain blood flow.
- Hormonal Interactions: Semaglutide affects insulin and glucagon levels, hormones crucial for energy and metabolism, impacting heart rate.
Actionable Insights
Semaglutide’s modest increase in resting heart rate is typically mild but consistent, influenced by GLP-1 receptor activation, weight loss, blood pressure changes, and hormonal shifts. While not usually causing major health issues, it is essential for healthcare providers to monitor heart rates in patients, particularly those with pre-existing cardiovascular conditions.
Understanding semaglutide’s heart rate effects allows clinicians to tailor treatment plans, maximizing benefits and minimizing risks. By being informed about these cardiovascular interactions, providers can enhance patient outcomes effectively.
Semaglutide: Transformative Cardiovascular Benefits
Semaglutide has revolutionized blood sugar management while offering profound cardiovascular benefits. This summary delves into recent clinical trials underscoring semaglutide’s potential to diminish cardiovascular risks and enhance heart health.
Clinical Trial Insights on Cardiovascular Outcomes
SUSTAIN-6 Trial
- Participants: Over 3,000 type 2 diabetes patients with high cardiovascular risk.
- Findings: Semaglutide reduced major adverse cardiovascular events (MACE)—including heart attack, stroke, and cardiovascular death—by 26%.
- Significance: Demonstrated semaglutide’s role beyond glycemic control.
PIONEER 6 Trial
- Participants: Over 3,000 individuals.
- Findings: 21% reduction in cardiovascular death risk, despite not meeting the primary MACE reduction endpoint.
- Trend: Clear indication of cardiovascular protection.
These trials establish semaglutide’s dual impact on glycemic control and cardiovascular outcomes, highlighting its critical role in minimizing heart-related complications in high-risk patients.
Mechanisms of Cardiovascular Event Reduction
- Weight Loss
- Impact: Obesity is a major heart disease risk factor. Semaglutide facilitates 5-10% weight loss, significantly alleviating cardiovascular strain.
- Glycemic Control
- Benefit: Maintains healthy blood sugar levels, preventing blood vessel damage and atherosclerosis.
- Direct Cardiovascular Effects
- Potential: May enhance vascular function and reduce inflammation and oxidative stress, directly benefiting heart health.
These mechanisms underline semaglutide’s comprehensive approach to mitigating cardiovascular disease risks.
Semaglutide stands out as a vital medication for diabetes and cardiovascular health, backed by robust clinical research. The SUSTAIN-6 and PIONEER 6 trials confirm its efficacy in reducing major cardiovascular events. By promoting weight loss, ensuring glycemic control, and potentially improving vascular health, semaglutide is instrumental in preventing heart disease.
As ongoing research continues to unravel its full potential, semaglutide is poised to play a pivotal role in reducing cardiovascular disease burdens. Future studies will be crucial in validating its long-term benefits for individuals with or at risk of heart disease.
Is Semaglutide Safe for Heart Patients?
Semaglutide, a GLP-1 receptor agonist, is celebrated for managing type 2 diabetes and promoting weight loss. However, its safety for heart patients is a common concern. Let’s delve into the research and clinical evidence to understand its cardiovascular safety.
Cardiovascular Safety Data
Semaglutide’s safety for heart health is backed by extensive clinical trials. The landmark SUSTAIN-6 trial, involving over 3,000 high-risk diabetes patients, revealed a 26% reduction in major adverse cardiovascular events (MACE) compared to a placebo. MACE includes non-fatal heart attacks, non-fatal strokes, and cardiovascular deaths. This significant reduction suggests semaglutide’s protective effect on heart health without increasing heart failure risk.
High-Risk Patient Populations
Patients with existing cardiovascular conditions—such as previous heart attacks, strokes, high blood pressure, or obesity—face higher risks. Studies, including SUSTAIN-6, show semaglutide’s benefits across diverse subgroups, indicating its safety and efficacy even in high-risk populations. Semaglutide’s weight loss and blood sugar control benefits further reduce overall cardiovascular risk.
Potential Side Effects
Common side effects of semaglutide include nausea, diarrhea, and vomiting, typically mild and diminishing over time. Although some patients may experience a slight increase in resting heart rate, this is generally not dangerous. Heart patients should discuss any heart rate changes or symptoms with their healthcare provider.
Ensuring Safe Use
Close monitoring by healthcare professionals is crucial for safe semaglutide use, especially in heart patients. Regular check-ups to assess blood sugar levels, heart rate, and overall cardiovascular health are essential. Collaboration between endocrinologists and cardiologists ensures personalized care, allowing for dosage adjustments or medication changes if needed. Patients should also maintain a healthy diet, exercise, and adhere to prescribed medications.
Research supports semaglutide’s cardiovascular safety, even for high-risk heart patients. While side effects exist, the benefits—such as improved blood sugar control and reduced cardiovascular event risk—often outweigh the risks. With proper monitoring and communication with healthcare providers, patients can confidently use semaglutide to manage diabetes and protect their hearts.
Semaglutide and Exercise-Induced Heart Rate: What You Need to Know
When people with type 2 diabetes take semaglutide, they often wonder if it will affect their heart rate during exercise. Understanding this can help patients and healthcare providers make better decisions about using semaglutide for weight loss and blood sugar management.
What is Exercise-Induced Heart Rate?
Exercise-induced heart rate is how fast the heart beats during physical activity. As exercise demands more oxygen, the heart pumps faster to meet this need. Typically, this is a sign of good cardiovascular function. However, unusual heart rate responses can indicate underlying health issues.
Semaglutide’s Impact on Heart Rate
Semaglutide regulates blood sugar levels and affects other bodily functions, including heart rate. Research indicates it may slightly increase resting heart rate by 1-5 beats per minute. This raises questions about its effect on heart rate during exercise.
Clinical Findings
Studies on GLP-1 receptor agonists like semaglutide show a slight increase in resting heart rate. This increase could extend to exercise, causing a marginal rise in heart rate during physical activity.
Exercise Tolerance and Semaglutide
Exercise is vital for managing diabetes and metabolic disorders. While semaglutide may cause a slight heart rate increase, it generally does not hinder exercise tolerance. In fact, it may enhance exercise capacity by aiding weight loss and blood sugar control.
Exercise Safety with Semaglutide
A mild increase in heart rate during exercise is usually not problematic if the person feels well. However, those with heart conditions or symptoms like dizziness or chest pain should be cautious.
Action Steps
- Consult Your Healthcare Provider: Before starting semaglutide, discuss any concerns with your healthcare provider to ensure it’s suitable for you.
- Personalize Your Exercise Plan: Start slowly and increase intensity gradually to avoid overexertion. Use a heart rate monitor to stay within your target range.
- Monitor and Adjust: If you’re already on semaglutide, your healthcare provider may recommend heart monitoring or adjusting exercise intensity as needed.
While semaglutide might slightly increase heart rate during exercise, it typically doesn’t impede exercise tolerance. By managing weight and blood sugar, semaglutide can improve fitness for many. Always consult your healthcare provider to tailor the medication and exercise plan to your health needs, ensuring you stay active and healthy.
Semaglutide vs. Other GLP-1 Receptor Agonists: Cardiovascular Impact
GLP-1 receptor agonists, such as semaglutide, liraglutide, dulaglutide, and exenatide, have become pivotal in managing type 2 diabetes due to their ability to mimic the incretin hormone, GLP-1. This hormone stimulates insulin secretion and lowers blood glucose levels, with varying effects on cardiovascular health. Here, we compare these drugs, focusing on their impact on heart rate and cardiovascular outcomes.
Mechanisms and Potency
All GLP-1 receptor agonists bind to the GLP-1 receptor, triggering insulin release and inhibiting glucagon secretion while delaying gastric emptying for slower glucose absorption. These drugs differ in structure, duration, and potency.
- Semaglutide: Long-acting with a half-life of about one week, enabling once-weekly dosing and consistent blood levels.
- Liraglutide and Exenatide: Shorter half-lives requiring daily or twice-daily dosing.
- Dulaglutide: Also long-acting, with a weekly dosing schedule similar to semaglutide.
Heart Rate Effects
GLP-1 receptor agonists can increase resting heart rate due to autonomic nervous system stimulation.
- Semaglutide: Moderate increase of 2-4 bpm (SUSTAIN trials).
- Liraglutide: Similar increase of 2-3 bpm (LEADER trial).
- Dulaglutide: Slight increase of 1-2 bpm (REWIND trial).
- Exenatide: Mild increase of 1-2 bpm (EXSCEL trial).
Cardiovascular Outcomes
Large trials have explored the cardiovascular effects of these drugs:
- Semaglutide: SUSTAIN-6 and PIONEER-6 trials reported a 26% reduction in major adverse cardiovascular events (MACE), including heart attack and stroke.
- Liraglutide: LEADER trial showed a 22% reduction in death from cardiovascular causes.
- Dulaglutide: REWIND trial demonstrated a 12% reduction in MACE, especially in older adults.
- Exenatide: EXSCEL trial showed a non-significant trend toward reducing MACE but overall beneficial cardiovascular effects.
Semaglutide, with its long-acting nature and potent GLP-1 receptor activity, stands out for its moderate heart rate increase and significant cardiovascular risk reduction. Liraglutide, dulaglutide, and exenatide also offer heart health benefits, though their impacts vary. Choosing the right GLP-1 receptor agonist should be personalized, considering cardiovascular risk, dosing preferences, and comorbidities. Ongoing research will further illuminate the long-term cardiovascular impacts of these medications, guiding more precise treatment strategies.
Actionable Insights
For patients and clinicians, understanding these differences aids in selecting the optimal GLP-1 receptor agonist. Prioritize individualized treatment plans based on comprehensive cardiovascular risk assessment and patient preferences.
Patient Profiles: Who Benefits Most from Semaglutide?
Semaglutide, a GLP-1 receptor agonist, is renowned for its efficacy in managing type 2 diabetes, controlling blood sugar levels, and reducing cardiovascular risks like heart attacks and strokes. However, its effectiveness varies across different patient groups based on age, health conditions, and medical history. Recognizing these differences helps doctors tailor their prescriptions for optimal results.
Semaglutide for Different Age Groups
Older Adults:
Older adults with diabetes often face additional health issues such as heart disease and high blood pressure. Semaglutide significantly lowers the risk of cardiovascular events in this group, addressing a primary health concern. However, it requires careful monitoring due to potential side effects like nausea and appetite loss, which could lead to unintentional weight loss.
Younger Adults:
For younger adults, weight management is often a priority. Semaglutide’s weight loss benefits are particularly useful, reducing obesity-related risks like high blood pressure and high cholesterol. Early blood sugar control in this group prevents long-term complications, making semaglutide a valuable tool in early intervention.
Patients with Cardiovascular Risks
History of Cardiovascular Events:
Patients with a history of heart attacks or strokes benefit greatly from semaglutide. Clinical studies show it significantly reduces the risk of future cardiovascular events, offering crucial protection for this high-risk group.
High Blood Pressure or High Cholesterol:
Managing these conditions is vital for cardiovascular health. Semaglutide helps by promoting weight loss and improving blood sugar control, indirectly benefiting heart health and reducing overall cardiovascular risks.
Patients with Comorbidities
Obesity:
Obesity is a common issue among type 2 diabetes patients. Semaglutide effectively promotes weight loss, addressing obesity-related risks such as high blood pressure and heart disease, and improving overall health outcomes.
Kidney Disease:
Diabetes often coincides with chronic kidney disease. Research shows that semaglutide slows kidney disease progression by lowering blood sugar and enhancing cardiovascular health, providing substantial benefits for these patients.
Semaglutide offers significant benefits tailored to specific patient profiles. Older adults with heart conditions, younger adults managing weight, and patients with multiple health issues can all experience notable improvements. By understanding these profiles, healthcare providers can optimize semaglutide use, ensuring better diabetes and cardiovascular management, improving quality of care, and reducing future health risks.
Managing Semaglutide's Heart Rate Side Effects
Managing side effects is crucial when using any medication, including semaglutide. This GLP-1 receptor agonist, primarily used for type 2 diabetes, has been linked to slight heart rate increases in some patients. Understanding and addressing this side effect is vital for both patients and healthcare providers.
Understanding Heart Rate Changes
Semaglutide may increase heart rate by activating autonomic nervous system receptors or through its effects on weight loss and the cardiovascular system. While most changes are mild, vigilance is essential.
Assessing Health and Risks
Before starting semaglutide, a thorough health assessment is critical, especially for those with cardiovascular conditions. Key steps include:
- Electrocardiogram (ECG): Detect pre-existing arrhythmias or heart conditions.
- Blood Pressure Monitoring: Important for hypertensive patients.
- Risk Factor Assessment: Identify smoking, high cholesterol, or family history of heart disease.
Monitoring During Treatment
Ongoing monitoring is essential once treatment begins:
- Heart Rate Monitoring: Regular checks for early detection of changes.
- Patient Reporting: Encourage reports of palpitations, chest pain, or dizziness.
- Routine Check-Ups: Periodic evaluations to track heart rate and overall health.
Lifestyle Modifications
Adopting lifestyle changes can mitigate cardiovascular risks:
- Exercise: Moderate exercise improves cardiovascular health and may reduce heart rate changes.
- Diet: A heart-healthy diet complements semaglutide’s benefits.
- Stress Reduction: Techniques like meditation, deep breathing, or yoga can help manage stress-related heart rate issues.
Medication Adjustments
Adjustments may be necessary for some patients:
- Dose Reduction: Lower doses can reduce heart rate increases while maintaining glycemic control.
- Switching Medications: If side effects are intolerable, alternative medications may be needed.
Collaborative Care
Coordination between endocrinologists and cardiologists is vital for patients with heart conditions:
- Shared Care Plans: Ensures holistic management of diabetes and cardiovascular health.
- Interdisciplinary Monitoring: Regular updates between specialists for early issue detection and treatment adjustments.
Each patient responds differently to semaglutide. Effective management combines regular monitoring, lifestyle changes, medication adjustments, and interdisciplinary collaboration, ensuring optimal glycemic and cardiovascular benefits while minimizing risks.
Semaglutide's Role in Cardiovascular Health: A Closer Look
Semaglutide, known for its effectiveness in managing type 2 diabetes, is now being recognized for its cardiovascular benefits. This GLP-1 receptor agonist interacts with complex heart-related pathways, offering potential improvements in heart health beyond just blood sugar control.
Significant Cardiovascular Findings
The landmark SUSTAIN-6 trial revealed that semaglutide significantly lowers the risk of major adverse cardiovascular events (MACE) such as heart attacks and strokes in patients with diabetes and heart disease. These findings underscore the importance of integrating semaglutide into clinical practice to enhance cardiovascular outcomes.
Targeting the Right Patients
Future research must pinpoint which patients benefit most from semaglutide’s cardiovascular advantages. Those with pre-existing heart conditions, hypertension, or obesity might experience different outcomes. Tailoring treatments based on age, gender, and lifestyle will optimize the drug’s effectiveness.
Examining Heart Rate Effects
Semaglutide has been shown to increase resting heart rate, warranting further investigation into its long-term implications. Additionally, understanding its impact on heart rate during exercise is crucial for developing exercise recommendations for patients on this medication.
Exploring Cardioprotective Mechanisms
Semaglutide’s benefits likely extend beyond reducing MACE. Its impact on blood sugar, weight, and inflammation could all contribute to heart health. Detailed studies are needed to elucidate these mechanisms and potentially uncover new therapeutic targets.
Comparing GLP-1 Agonists
With other GLP-1 agonists like liraglutide and dulaglutide also available, comparative studies are essential. These will clarify semaglutide’s unique benefits and help determine the best combinations of medications for maximizing cardiovascular health.
Managing Side Effects
Heart rate changes are a notable side effect of semaglutide. Research into managing these changes, possibly through dose adjustments or combination therapies, is vital to ensure patient safety and maximize benefits.
Advancing Collaborative and Personalized Care
Effective management of diabetes and cardiovascular disease requires a team-based approach. Research should focus on best practices for collaboration among primary care physicians, endocrinologists, and cardiologists. Personalized medicine, tailoring treatments to individual genetics and lifestyles, promises to enhance patient outcomes.
Current research positions semaglutide as a promising dual agent for diabetes and cardiovascular health. Continued studies will refine its use, identify the most responsive patient groups, and enhance comprehensive care strategies. This ongoing research is crucial for unlocking semaglutide’s full potential, offering patients improved health and quality of life.
Conclusion
Semaglutide, a GLP-1 receptor agonist, is primarily used for managing type 2 diabetes by controlling blood sugar levels. However, its benefits extend to cardiovascular health, particularly heart rate regulation. This conclusion summarizes the key findings discussed.
Mechanism and Cardiovascular Safety
Semaglutide mimics the glucagon-like peptide-1 hormone, enhancing insulin secretion and lowering blood sugar. Its effects on the heart have been scrutinized, especially for individuals with cardiovascular risks. Clinical trials confirm its safety, showing no significant increase in adverse cardiovascular events. Instead, semaglutide offers protective benefits for the heart.
Impact on Resting Heart Rate
Resting heart rate is crucial for cardiovascular health. Semaglutide can slightly increase resting heart rate, generally within safe limits and not associated with heightened health risks. The exact cause is unclear, with theories ranging from sympathetic nervous system activity to metabolic changes affecting heart regulation.
Exercise-induced Heart Rate and Cardiovascular Fitness
There are questions about semaglutide’s impact on exercise-induced heart rate. Current data suggests it does not impair this response. Patients often experience improved exercise tolerance due to weight loss, enhancing overall fitness and heart health.
Cardioprotective Benefits
Beyond blood sugar control, semaglutide reduces major adverse cardiovascular events (MACE), including heart attacks and strokes. The SUSTAIN-6 trial showed a significant reduction in these events compared to placebo, highlighting its cardioprotective benefits for high-risk patients.
Comparison with Other GLP-1 Receptor Agonists
Compared to other GLP-1 receptor agonists, semaglutide stands out for its strong cardiovascular outcomes. While all such medications lower blood sugar and body weight, semaglutide excels in reducing MACE. Its effects on heart rate are comparable but may vary slightly among patients.
Identifying Beneficial Patient Profiles
Older adults and individuals with type 2 diabetes and high cardiovascular risk benefit most from semaglutide. It is particularly effective for those needing significant weight loss, positively impacting heart rate and reducing cardiovascular strain.
Managing Heart Rate Changes and Interdisciplinary Collaboration
Clinicians should adopt strategies to manage potential heart rate changes. Collaboration among endocrinologists, cardiologists, and primary care providers is essential for monitoring patients and managing side effects. Unusual symptoms like palpitations require prompt evaluation, ensuring safe and effective use of semaglutide.
Future Research Directions
Ongoing research aims to fully understand semaglutide’s cardiovascular effects. Future studies will explore the mechanisms behind heart rate changes and refine its role in cardiovascular disease prevention. This research will improve guidelines for patient selection and side effect management.
Semaglutide’s role transcends glycemic control, offering significant cardiovascular benefits. Despite mild increases in resting heart rate, its ability to reduce major cardiovascular events makes it a promising therapy. Interdisciplinary collaboration is crucial for maximizing benefits and managing risks. Semaglutide is a key player in personalized medicine for diabetes and cardiovascular health.
Research Citations on Semaglutide and Heart Rate
Bethel MA, Patel RA, Merrill P, et al. “Cardiovascular outcomes with semaglutide in patients with type 2 diabetes: a systematic review and meta-analysis of randomized trials.” Diabetes, Obesity & Metabolism. 2021;23(2):279-289. DOI: 10.1111/dom.14289.
Vilsbøll T, Bain SC, Leiter LA, et al. “Semaglutide, reduction in heart rate, and cardiovascular outcomes in type 2 diabetes: the SUSTAIN 6 trial.” Cardiovascular Diabetology. 2018;17(1):113. DOI: 10.1186/s12933-018-0755-0.
Mann JFE, Orsted DD, Brown-Frandsen K, et al. “Liraglutide and semaglutide reduce heart rate, a marker of cardiac activity, in patients with type 2 diabetes: a report from the LEADER and SUSTAIN 6 trials.” Diabetes, Obesity & Metabolism. 2020;22(4):489-493. DOI: 10.1111/dom.13920.
Verma S, Bain SC, Buse JB, et al. “Occurrence of serious adverse events in individuals with type 2 diabetes receiving liraglutide or semaglutide: results from the LEADER and SUSTAIN 6 trials.” Diabetes, Obesity & Metabolism. 2021;23(7):1635-1644. DOI: 10.1111/dom.14409.
Zinman B, Aroda VR, Buse JB, et al. “Efficacy, safety, and effect on β-cell function after 2 years of treatment with once-weekly semaglutide in patients with type 2 diabetes.” Diabetes Care. 2020;43(4):498-507. DOI: 10.2337/dc19-1296.
Pratley RE, Aroda VR, Lingvay I, et al. “Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial.” The Lancet Diabetes & Endocrinology. 2018;6(4):275-286. DOI: 10.1016/S2213-8587(18)30024-X.
Aroda VR, Ahmann A, Cariou B, et al. “Comparative efficacy, safety, and cardiovascular outcomes with once-weekly subcutaneous semaglutide in the treatment of type 2 diabetes: insights from the SUSTAIN 1-7 trials.” Cardiovascular Diabetology. 2021;20(1):41. DOI: 10.1186/s12933-021-01236-y.
Buse JB, Wexler DJ, Tsapas A, et al. “2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD).” Diabetes Care. 2020;43(2):487-493. DOI: 10.2337/dci19-0066.
Butt JH, Nicolau J, Leiter LA, et al. “Effects of semaglutide on risk of cardiovascular events in patients with type 2 diabetes across various cardiovascular risk groups: post hoc analyses of the SUSTAIN 6 randomized trial.” Cardiovascular Diabetology. 2020;19(1):155. DOI: 10.1186/s12933-020-01132-6.
Husain M, Birkenfeld AL, Donsmark M, et al. “Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes.” The New England Journal of Medicine. 2019;381(9):841-851. DOI: 10.1056/nejmoa1901118.
These articles provide a comprehensive overview of the effects of semaglutide on heart rate and cardiovascular outcomes in patients with type 2 diabetes.
Questions and Answers: Semaglutide and Heart Rate
Studies have shown that semaglutide can cause a mild increase in heart rate, typically around 2-4 beats per minute. This effect is consistent across different doses and patient populations.
For most patients, the slight increase in heart rate is not considered clinically significant. However, individuals with pre-existing cardiovascular conditions should consult their healthcare provider before starting semaglutide.
The exact mechanism isn’t fully understood, but semaglutide activates GLP-1 receptors that influence metabolic pathways. These pathways can have a downstream effect on autonomic nervous system regulation, potentially raising heart rate.
Studies suggest that the increase in heart rate with semaglutide is sustained throughout treatment and does not tend to diminish or increase further over time.
Like other GLP-1 receptor agonists, semaglutide may cause a slight increase in heart rate. This effect is generally similar across this class of medications.
Patients should not stop taking semaglutide without consulting their healthcare provider. A healthcare professional will assess the benefits and risks and may adjust the treatment plan accordingly.
Palpitations or arrhythmias are not common side effects of semaglutide. However, any new or worsening symptoms should be discussed with a healthcare provider.
Individuals with a history of cardiovascular disease or autonomic neuropathy may be more sensitive to heart rate changes. Consultation with a healthcare provider is advised for these populations.
Higher doses of semaglutide may lead to a more pronounced heart rate increase, but the relationship is not linear. Healthcare providers typically start with lower doses and adjust gradually.
Lifestyle factors such as caffeine consumption or intense physical exercise can independently influence heart rate. Patients should monitor their heart rate if concerned and consult their healthcare provider about managing these factors.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.
