Table of Contents
Introduction: Why Tirzepatide and Fatty Liver Disease Matter
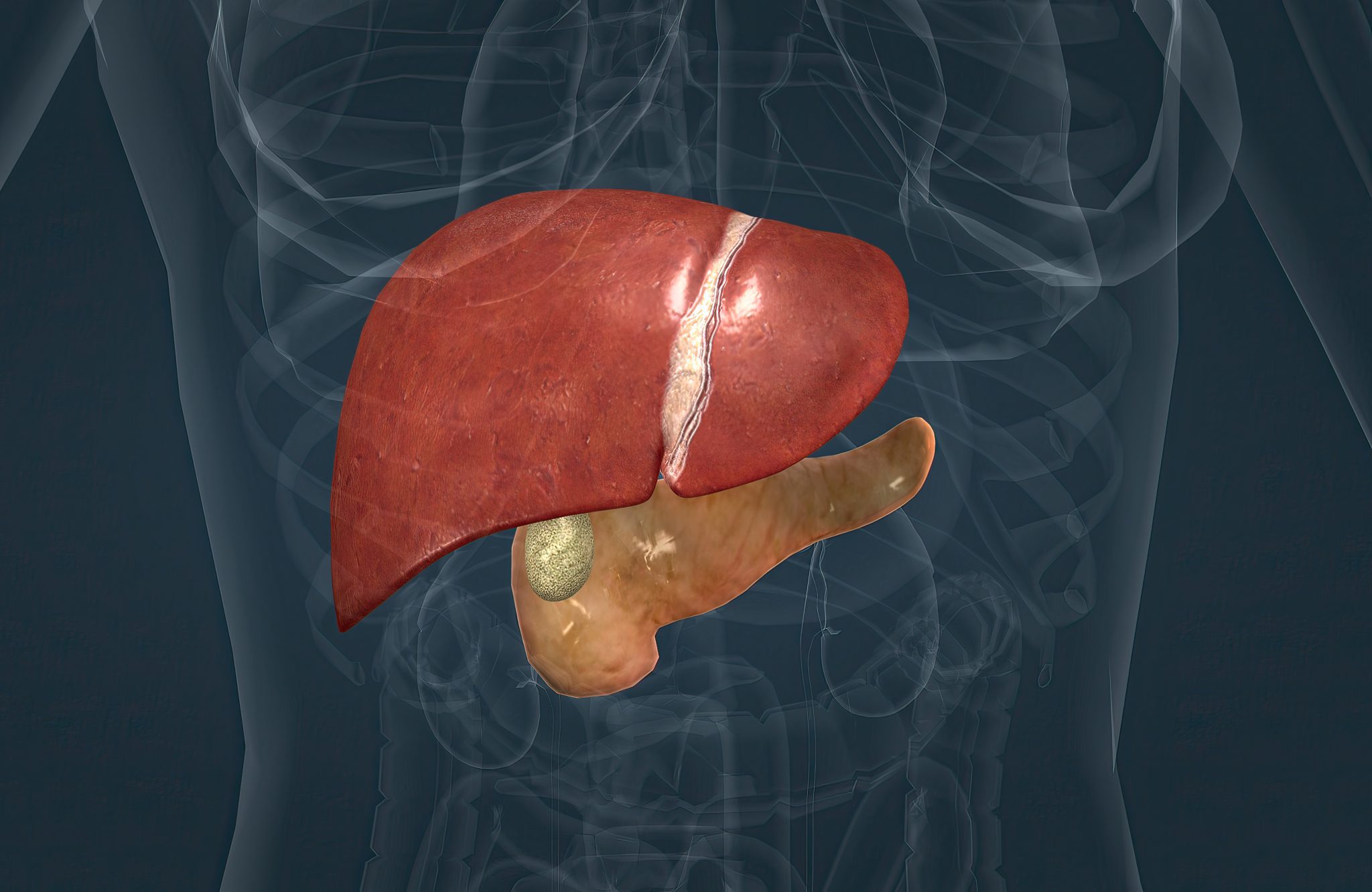
Fatty liver disease has become one of the most common liver problems in the world today. It happens when too much fat builds up in the liver. Doctors call this condition non-alcoholic fatty liver disease (NAFLD) when alcohol is not the main cause. If the liver also shows swelling, cell injury, and scarring, the disease is called non-alcoholic steatohepatitis (NASH). Over time, NASH can lead to advanced scarring, known as fibrosis, and even cirrhosis or liver cancer. These liver complications are serious and can shorten life. What makes fatty liver especially concerning is that it is closely linked to obesity, type 2 diabetes, and heart disease. As obesity and diabetes have risen worldwide, fatty liver has become an urgent health issue affecting millions.
Right now, there are no widely approved medicines made specifically for fatty liver disease in most parts of the world. Doctors mainly tell patients to lose weight, eat healthier food, and exercise more. These steps can improve the liver, but they are often hard to keep up with. Many patients struggle to lose enough weight to see a real difference in their liver health. Because of this, researchers have been searching for medicines that can target both body weight and liver fat at the same time. That is where tirzepatide has caught attention.
Tirzepatide is a new type of medicine that was first developed for type 2 diabetes. It is given as a weekly injection. Tirzepatide works by activating two natural hormones in the body: GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones help control blood sugar, appetite, and energy use. By acting on both hormones, tirzepatide can lower blood sugar, reduce appetite, and cause significant weight loss. In fact, some studies show that people taking tirzepatide can lose over 20% of their body weight, which is more than what many other diabetes or weight-loss medicines can achieve.
Because weight loss is one of the most powerful tools to improve fatty liver, researchers began to test tirzepatide in patients with NAFLD and NASH. Early findings are very promising. Some studies using advanced imaging have shown that tirzepatide can reduce the amount of fat stored in the liver. Other studies report improvements in liver blood tests like ALT and AST, which are often high in people with fatty liver. There are also early signs that tirzepatide may help improve inflammation and scarring in the liver, but these results are still being studied in larger, longer trials.
This article will explore the latest research and clinical trial evidence on tirzepatide and fatty liver disease. The goal is to answer the most common questions people ask when searching online, such as: Can tirzepatide actually reverse fatty liver? How does it work in the liver? How much improvement can patients expect, and how quickly? Is it safe for people with liver disease? Can people without diabetes use it? And how should progress be monitored once treatment begins?
To answer these questions, the article will look at what we know from published studies, what is still under investigation, and how doctors might use tirzepatide in real-world practice. The article will also place tirzepatide in the larger picture of NAFLD and NASH care, which still relies on lifestyle changes and careful management of weight, diabetes, cholesterol, and blood pressure. Since fatty liver is often a sign of broader metabolic disease, the benefits of tirzepatide may go beyond the liver to also protect the heart, blood vessels, and pancreas.
The reader should understand from the start that while tirzepatide looks very promising, the science is still developing. No single medicine is yet a complete solution for fatty liver. Still, tirzepatide represents one of the most hopeful advances so far, especially because it tackles both body weight and metabolic health at once. By the end of this article, readers will have a clear picture of what tirzepatide can and cannot do for fatty liver today, what results might be realistic, and what new findings are expected in the near future.
NAFLD and NASH in 2025: Definitions, Staging, and Unmet Needs
Fatty liver disease has become one of the most common liver problems worldwide. It is closely linked with rising rates of obesity, type 2 diabetes, and metabolic syndrome. In this section, we will look at how experts define the disease today, how it progresses, and why new treatments like tirzepatide are being studied so closely.
Understanding the New Terms: MASLD and MASH
In the past, doctors used the terms NAFLD (non-alcoholic fatty liver disease) and NASH (non-alcoholic steatohepatitis). These terms described people who had too much fat in their liver but did not drink much alcohol.
In 2023, medical groups proposed new names:
- MASLD: Metabolic dysfunction–associated steatotic liver disease. This means fat buildup in the liver caused mainly by problems with metabolism, such as insulin resistance, obesity, and high blood sugar.
- MASH: Metabolic dysfunction–associated steatohepatitis. This is the more serious form. It includes not only fat in the liver, but also inflammation and liver cell injury. Over time, this can lead to scar tissue, also known as fibrosis.
Doctors still use NAFLD and NASH often, but MASLD and MASH are becoming the preferred terms. The new names highlight the strong connection between fatty liver and metabolic diseases.
The Stages of Fatty Liver Disease
Fatty liver disease does not look the same in every person. It is a spectrum that ranges from mild to severe:
- Simple steatosis (fatty liver): Extra fat builds up in the liver. Many people may not have symptoms, and the liver can still work normally.
- MASH (formerly NASH): Inflammation and liver cell injury appear. This stage carries a higher risk of progression.
- Fibrosis: The liver begins to form scar tissue as it tries to repair itself. Fibrosis can be mild at first but may become advanced.
- Cirrhosis: Severe scarring changes the structure of the liver and makes it hard for the organ to work. Cirrhosis increases the risk of liver failure and liver cancer.
Not everyone with fatty liver will progress to cirrhosis. However, because so many people are affected worldwide, even a small percentage progressing to severe disease means millions of people could face serious complications.
How Fatty Liver Develops: The Science in Simple Terms
At the root of fatty liver is insulin resistance. When the body cannot use insulin well, fat builds up in the liver. This fat is not harmless—it can become toxic and cause liver cells to swell and die. The dying cells trigger inflammation, which attracts immune cells to the liver.
Over time, repeated cycles of injury and healing lead to fibrosis, the scarring process. Just like scars on the skin, liver scars are the body’s way of trying to repair damage. But too much scar tissue makes the liver stiff and less able to function.
In addition to insulin resistance, other factors can worsen fatty liver:
- High sugar intake (especially from sugary drinks).
- High cholesterol and triglycerides.
- Genetic differences that affect fat handling in the liver.
- Gut bacteria changes that influence inflammation.
Current Standard of Care
Right now, there are no widely approved medicines specifically for NAFLD or NASH. The main treatment is lifestyle change, especially weight loss. Studies show that losing 7–10% of body weight can significantly reduce liver fat, improve inflammation, and even reverse fibrosis in some cases.
Doctors usually recommend:
- A healthy, balanced diet that reduces calories and cuts down on added sugars.
- Regular physical activity, aiming for at least 150 minutes of moderate exercise per week.
- Limiting or avoiding alcohol, even though the disease is not caused by drinking.
Other treatments focus on managing conditions linked to fatty liver, such as:
- Diabetes control with medications that improve insulin sensitivity.
- Cholesterol treatment with statins, which are safe in most liver patients.
- Blood pressure control to lower overall cardiovascular risk.
While these steps are important, many patients find it hard to lose enough weight and keep it off. This gap has pushed researchers to look for new therapies that target both metabolism and liver disease at the same time.
Why Incretin-Based Therapies Are Important
Incretins are natural hormones that help regulate blood sugar and appetite. Medicines that mimic these hormones—such as GLP-1 receptor agonists (semaglutide, liraglutide) and the newer dual GIP/GLP-1 agonist tirzepatide—were first developed for diabetes and obesity.
Researchers noticed that patients taking these drugs not only lost weight but also showed improvements in liver fat and inflammation. This led to clinical trials testing whether incretin therapies could be a breakthrough option for NAFLD and NASH.
Tirzepatide is especially interesting because it acts on two pathways (GIP and GLP-1), and early results suggest it may reduce liver fat more strongly than older medicines. If confirmed, this could represent a major step forward in treating MASLD and MASH.
Can Tirzepatide Reverse Fatty Liver?
One of the most common questions patients and healthcare providers ask today is whether tirzepatide can actually reverse fatty liver disease. To answer this, it helps to first understand what “reverse” means in this setting, then review what the evidence shows across imaging tests, blood markers, and liver tissue samples.
What Does “Reverse” Mean in Fatty Liver Disease?
In medicine, reversal of fatty liver does not always mean that the liver is completely “cured.” Instead, doctors look for specific signs of improvement, such as:
- Reduced liver fat content – measured by imaging tests such as MRI-PDFF (proton density fat fraction) or ultrasound-based elastography.
- Improved liver enzymes – lower levels of ALT (alanine aminotransferase) and AST (aspartate aminotransferase), which are markers of liver injury.
- Resolution of NASH (nonalcoholic steatohepatitis) – shown on liver biopsy when inflammation and ballooning of liver cells are no longer present.
- Regression of fibrosis – meaning that scar tissue in the liver is reduced by at least one stage when compared with baseline.
When researchers or doctors say a therapy “reverses fatty liver,” they usually mean that at least one or more of these improvements has occurred.
Evidence From Imaging Studies
The strongest and most consistent finding so far is that tirzepatide reduces liver fat content.
- In clinical trials of people with obesity and type 2 diabetes, MRI scans showed that tirzepatide significantly lowered the percentage of fat in the liver after 6 to 12 months of treatment.
- In some studies, patients experienced absolute reductions of 8–10% or more in liver fat fraction. This is important, because research has shown that even a 5% reduction in liver fat can improve liver health and lower the risk of progression.
- The effect also seems to be dose-dependent. Higher doses of tirzepatide, such as 10 mg or 15 mg once weekly, tend to produce greater reductions in liver fat compared with lower doses.
This imaging evidence is strong and supports the idea that tirzepatide can directly reduce fat buildup in the liver.
Evidence From Blood Markers
Another way to measure liver improvement is by looking at liver enzymes in the blood.
- Many patients on tirzepatide see lower ALT and AST levels within months of starting therapy.
- These changes often parallel weight loss and improvements in blood sugar, suggesting that both metabolic control and fat reduction play a role.
- Some trials also show improvements in non-invasive fibrosis scores, such as FIB-4 or NAFLD fibrosis score. While not perfect, these tools give an estimate of liver scarring risk without needing a biopsy.
Overall, the reduction in liver enzymes and risk scores adds more evidence that tirzepatide has a beneficial effect on fatty liver disease.
Evidence From Liver Biopsies
The most direct way to test whether tirzepatide reverses fatty liver is through liver biopsy, which allows pathologists to see inflammation, fat, and scarring under a microscope.
- Early-phase trials and ongoing studies have begun to collect biopsy data, but so far, published biopsy results are limited.
- In some small studies, patients on tirzepatide showed signs of NASH resolution without worsening fibrosis, which is a key regulatory endpoint.
- Signals of fibrosis regression are less clear. Some studies show improvement in non-invasive markers, but actual biopsy-proven fibrosis reduction still needs confirmation in larger and longer trials.
At this stage, biopsy data suggest that tirzepatide may help reduce inflammation and fat, but whether it can consistently reverse scarring (fibrosis) is not yet proven.
What Is “Likely,” “Possible,” and “Not Yet Proven”
- Likely: Tirzepatide reduces liver fat and improves liver enzyme levels. These effects have been repeatedly shown in multiple clinical trials.
- Possible: Tirzepatide may resolve NASH in some patients. Early biopsy data and indirect evidence suggest this is possible, especially with higher doses and longer treatment.
- Not yet proven: Tirzepatide reverses liver fibrosis. While there are positive signals, strong proof requires large phase 3 trials with biopsy endpoints and long-term follow-up.
The current evidence shows that tirzepatide can meaningfully improve fatty liver disease, especially by lowering liver fat and improving liver enzymes. It may also help resolve NASH in some patients. However, whether it can fully reverse the disease—including scarring and long-term outcomes like cirrhosis—remains under investigation.
For now, tirzepatide looks very promising, but more research is needed to confirm how far its benefits go in reversing the full spectrum of fatty liver disease.
How Does Tirzepatide Work in the Liver?
Tirzepatide is a new type of medicine that was first developed to treat type 2 diabetes and obesity. It is sometimes called a dual incretin agonist because it works on two important hormone systems in the body: GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones are part of a natural group called incretins that help regulate blood sugar, appetite, and energy balance.
In people with fatty liver disease, these same pathways seem to also improve how the liver stores and handles fat. Understanding how tirzepatide works gives us a clearer picture of why it may help in conditions like NAFLD (nonalcoholic fatty liver disease) and NASH (nonalcoholic steatohepatitis).
Dual action: GLP-1 and GIP
Most people are already familiar with GLP-1 medicines, since drugs like semaglutide are widely used for diabetes and weight loss. GLP-1 receptor activation lowers blood sugar, slows stomach emptying, reduces appetite, and promotes weight loss.
Tirzepatide goes one step further by also stimulating GIP receptors. GIP is another incretin hormone released by the small intestine after meals. When GIP is activated together with GLP-1, the two hormones work in a complementary way:
- GLP-1 effect: decreases appetite, lowers food intake, and supports blood sugar control.
- GIP effect: improves fat metabolism in fat tissue, increases insulin sensitivity, and may enhance the body’s ability to burn calories.
The combination is believed to create a stronger, more balanced improvement in weight loss and metabolic health than GLP-1 alone.
Indirect effects on the liver
The liver in NAFLD is overloaded with fat. Most of this fat comes from extra calories stored in fat tissue and then sent to the liver. Tirzepatide helps reduce this burden through several indirect mechanisms:
- Weight loss and calorie reduction:
By reducing appetite and helping people eat less, tirzepatide leads to significant weight loss. Even a 7–10% loss of body weight can reduce liver fat and inflammation in many patients. Tirzepatide often produces weight loss well above this threshold. - Improved insulin sensitivity:
Insulin resistance is a major driver of fatty liver disease. When tissues stop responding properly to insulin, the liver produces more glucose and stores more fat. Tirzepatide improves insulin sensitivity in muscle, fat, and the liver, which lowers the supply of fat to the liver and reduces new fat production. - Better fat handling by adipose tissue:
Healthy fat tissue should store extra energy safely. In obesity and insulin resistance, fat “spills over” into the liver and muscles. Tirzepatide seems to restore healthier fat tissue function, reducing this overflow and decreasing liver fat storage.
Possible direct effects on the liver
Scientists are also studying whether tirzepatide acts directly on the liver, beyond its effects on weight and blood sugar. While human studies are ongoing, early laboratory and animal research suggests:
- GLP-1 and GIP receptors may be present in liver and fat tissue.
- Activation of these receptors might reduce de novo lipogenesis (the liver’s process of making new fat).
- Tirzepatide may reduce oxidative stress and inflammatory signals in the liver.
- It could also slow the build-up of scar tissue (fibrosis), though this has not been firmly proven in humans yet.
These potential direct actions are exciting, but the strongest evidence so far still points to weight loss and metabolic improvement as the main drivers of benefit.
Weight-loss dependent vs. independent effects
A key question researchers ask is: Are tirzepatide’s benefits in fatty liver only due to weight loss, or is there something extra?
Current evidence shows that:
- Most of the improvements in liver fat content are linked to how much weight a person loses.
- However, some studies suggest there may be added benefits even when weight loss is accounted for, especially in improving insulin sensitivity and reducing liver inflammation.
- More research is needed to separate these effects, but for now, clinicians usually explain that the majority of liver benefits come through sustained weight reduction.
Tirzepatide is not a liver-specific drug, but its strong effects on weight loss, insulin resistance, and fat metabolism make it a promising therapy for fatty liver disease. While most of its benefits likely come from lowering body weight and improving overall metabolic health, research continues to explore whether it may also act directly inside the liver to reduce fat, calm inflammation, and slow scarring.
How Much Liver Fat Reduction Can Patients Expect—and How Fast?
One of the most common questions people ask is how quickly tirzepatide can lower liver fat and by how much. To understand this, it helps to know how doctors measure improvement and what the research has shown so far.
How Doctors Measure Liver Fat
Liver fat can be checked in different ways:
- Blood tests: High ALT and AST levels are signs of liver injury. These often improve within weeks when the liver starts healing.
- Imaging tests: Special scans, like MRI-PDFF (proton density fat fraction) or FibroScan with CAP (controlled attenuation parameter), can measure liver fat directly. These tests are very sensitive and can show fat loss even before blood tests improve.
- Biopsy: This is the most accurate way to see changes in fat, inflammation, and fibrosis, but it is invasive, so it’s not done often in studies.
Most clinical trials with tirzepatide use imaging and blood tests rather than biopsy, but these still give strong evidence.
How Fast Do Changes Happen?
Tirzepatide begins to affect the body as soon as treatment starts, but the speed of change depends on the marker being measured:
- Liver enzymes (ALT, AST):
Improvements in ALT and AST have been seen in as little as 4 to 8 weeks. This early change shows that liver cells are under less stress and damage. - Liver fat on MRI-PDFF:
Meaningful reductions in fat fraction are usually seen within 12 to 24 weeks. Studies suggest that a reduction of about 30% or more in liver fat on MRI-PDFF is linked to better chances of resolving NASH (the more severe form of fatty liver). - Histology (biopsy changes):
To see clear changes in inflammation and fibrosis on biopsy, treatment usually needs to continue for at least 12 to 18 months. This is because fibrosis (scar tissue) develops slowly and also takes longer to improve.
How Much Reduction Is Typical?
The amount of liver fat reduction depends on the dose of tirzepatide and the person’s baseline weight and metabolic health.
- In clinical trials, tirzepatide has shown reductions in liver fat of 30% to 60%, depending on the dose.
- For example, at higher doses (10 mg to 15 mg weekly), many patients reached MRI-PDFF reductions of 8–10 percentage points, which can mean moving from severe fatty liver into a healthier range.
- Even lower doses can give meaningful improvements, especially when combined with weight loss and lifestyle changes.
To put this into context, doctors usually aim for at least 5–7% total body weight loss to see improvements in liver fat, and 10% or more weight loss to see improvements in inflammation and scarring. Tirzepatide helps many patients reach or exceed these targets.
Factors That Influence Response
Not everyone responds in the same way. Some factors that influence how much liver fat falls and how quickly include:
- Baseline BMI and fat distribution:
People with higher body mass index or central obesity may start with higher liver fat and see larger reductions, but they may also need longer treatment. - Presence of type 2 diabetes:
Patients with diabetes often have higher insulin resistance, so improvements may be slower at first. Still, tirzepatide improves blood sugar and insulin sensitivity, which helps reduce fat over time. - Adherence to treatment:
Regular weekly injections are needed for best results. Skipping doses or stopping too soon can limit liver improvements. - Lifestyle factors:
Combining tirzepatide with a balanced diet, reduced alcohol use, and regular exercise can speed improvements. Resistance training and protein intake help maintain lean muscle while fat is lost.
What Patients Can Realistically Expect
- Within 1–2 months: Small but real improvements in liver enzymes (ALT/AST). Some patients may also notice early weight loss, which contributes to liver benefits.
- Within 3–6 months: Significant liver fat reduction on imaging in most patients, often by 30% or more.
- Within 12 months and beyond: Ongoing weight loss and continued fat reduction, with some patients showing signs of NASH resolution and possible fibrosis improvement.
Why Patience Matters
It is important to set realistic expectations. Fatty liver disease develops over many years. While tirzepatide works quickly on weight and liver fat, improvements in fibrosis and overall liver health take time. Doctors often say that short-term changes are encouraging, but the true test is sustained improvement over 1–2 years. Patients should think of tirzepatide as part of a long-term plan for metabolic and liver health, not as a quick fix.
Does Tirzepatide Improve NASH Inflammation and Fibrosis?
One of the most important questions about fatty liver disease is whether tirzepatide can do more than just lower liver fat. People with NAFLD may develop nonalcoholic steatohepatitis (NASH), also called metabolic dysfunction–associated steatohepatitis (MASH). NASH is the more serious stage of disease because it involves inflammation and damage to liver cells. Over time, this damage can lead to fibrosis (scar tissue) and eventually cirrhosis, which can cause liver failure or liver cancer.
Because of this, researchers are not only asking whether tirzepatide reduces fat in the liver, but also whether it improves inflammation and fibrosis. Let’s look at what the current evidence shows.
What Do “NASH Resolution” and “Fibrosis Improvement” Mean?
When scientists test new drugs for fatty liver, they look at very specific endpoints on liver biopsy:
- NASH resolution without worsening fibrosis: This means the signs of steatohepatitis (fat, ballooned cells, inflammation) improve or disappear, while scar tissue does not get worse.
- Fibrosis improvement: This means at least one stage of fibrosis regression is seen, without worsening of the other features of NASH.
These endpoints are important because the U.S. Food and Drug Administration (FDA) and European regulators use them to decide if a treatment can be approved. So, any new therapy like tirzepatide is judged against these measures.
Evidence So Far on Inflammation
Most of the completed tirzepatide studies have focused on liver fat reduction, measured by MRI scans, and improvements in blood markers such as ALT and AST. These are good signs, but they are indirect measures of inflammation.
Some smaller biopsy-based trials and ongoing phase 2 studies have begun to show that patients on tirzepatide can achieve higher rates of NASH resolution compared to placebo. Early reports suggest that when patients lose a significant amount of weight (often 15% or more of body weight), many also show improvements in the ballooning and inflammatory activity in the liver.
Still, the exact percentage of patients who achieve full NASH resolution on tirzepatide is not yet known, because large phase 3 trials are still underway. But the signals are promising, and they are consistent with what has been seen for GLP-1 agonists like semaglutide.
Evidence So Far on Fibrosis
Fibrosis is the most difficult part of fatty liver disease to treat. While liver fat can be reduced within months, fibrosis often takes years to regress.
In early tirzepatide studies, some patients have shown reductions in non-invasive fibrosis scores such as the FIB-4 or ELF test. Imaging tests, like elastography, have also suggested improvement in liver stiffness, which may mean less scar tissue. However, these are indirect markers.
So far, very few patients have had follow-up biopsies showing confirmed fibrosis regression. This does not mean tirzepatide does not help fibrosis; it may just mean we need longer studies to see the effect. Fibrosis tends to improve only after fat and inflammation are reduced for a sustained period of time. Since tirzepatide produces large and lasting weight loss, there is reason to believe it will also help fibrosis over years of use.
Why This Matters for Patients
The distinction between improving steatosis (fat only) versus improving NASH and fibrosis is critical. Fat reduction lowers liver stress and improves lab numbers, but stopping inflammation and reversing fibrosis is what prevents long-term outcomes like cirrhosis, liver cancer, or need for a transplant.
If tirzepatide can truly improve both NASH and fibrosis, it could become one of the first medications to address the root disease process, not just the fat buildup. That is why ongoing trials are so closely watched.
What We Know vs. What Is Still Unknown
What we know now:
- Tirzepatide consistently lowers liver fat, sometimes dramatically.
- ALT and AST (markers of inflammation) usually improve in parallel.
- Some early data suggest higher rates of NASH resolution compared to placebo.
- Non-invasive fibrosis markers often improve, but biopsy-proven fibrosis data are limited.
What we do not know yet:
- Whether tirzepatide can achieve FDA-accepted endpoints of NASH resolution and/or fibrosis improvement in large, long-term trials.
- How durable these improvements are after several years.
- Whether fibrosis regression will be seen at the same level as fat and inflammation improvements.
Clinical Relevance
Even though the full biopsy data are not yet available, tirzepatide’s ability to cause large weight loss and improve insulin sensitivity is already meaningful. Weight loss of 10% or more is known to improve NASH and sometimes fibrosis, regardless of how it is achieved. Tirzepatide gives many patients the best chance of reaching this weight-loss target.
So, while we cannot yet say with certainty that tirzepatide reverses fibrosis, the early evidence points in that direction, and ongoing trials will answer this question more clearly.
Is Tirzepatide’s Benefit Independent of Weight Loss?
One of the most common questions about tirzepatide is whether its liver benefits come only from weight loss, or if it has effects on the liver beyond lowering body weight. This is an important point, because while weight loss is the main proven treatment for fatty liver disease, not all patients can reach the level of weight reduction needed to reverse inflammation or fibrosis. Understanding whether tirzepatide has weight-loss–independent effects helps doctors know how best to use it in people with NAFLD or NASH.
Weight Loss and the Liver: Why It Matters
Weight gain, especially excess belly fat, plays a key role in the development of NAFLD. Extra fat leads to insulin resistance, which then drives fat buildup inside the liver (steatosis). Over time, this can lead to inflammation, cell injury, and eventually fibrosis. Studies have shown that losing at least 7–10% of body weight can improve or even reverse fatty liver disease in many patients.
Because of this, it is logical to think that tirzepatide’s benefits are simply the result of the large weight loss it produces. Many people taking tirzepatide lose 15–20% of their body weight, which is much greater than what most lifestyle-only approaches achieve. The question is: does tirzepatide also improve liver health in ways that are not just explained by weight reduction?
What Studies Show When Adjusting for Weight Loss
Clinical trial data have started to look at this question. In some studies, researchers compared changes in liver fat and liver enzymes after adjusting for the amount of weight each patient lost. Even after taking weight loss into account, some improvements in liver fat and liver inflammation markers remained.
For example:
- Imaging studies using MRI-PDFF (a test that measures liver fat directly) showed that liver fat content dropped significantly in people taking tirzepatide. While much of this drop was tied to weight loss, some of the effect appeared stronger than expected based on weight alone.
- Blood tests like ALT and AST, which measure liver inflammation, also improved. These changes often occurred early in treatment, sometimes before patients had lost large amounts of weight, suggesting other direct or indirect mechanisms.
Possible Weight-Loss–Independent Effects
Several biological pathways may explain how tirzepatide helps the liver beyond weight loss:
- Improved Insulin Sensitivity
Tirzepatide lowers blood sugar by improving the way the body responds to insulin. Better insulin sensitivity reduces the liver’s production of new fat and lowers stress on liver cells. - Reduced De Novo Lipogenesis
The liver often produces fat from excess sugar. Tirzepatide may slow this process, decreasing fat buildup inside the liver. - Healthier Adipose Tissue Function
By improving how fat tissue stores and releases energy, tirzepatide may prevent “overflow” fat from spilling into the liver. - Anti-Inflammatory Actions
Some studies suggest GLP-1 and GIP receptor activity can reduce inflammatory signals in the body. Less inflammation means less liver cell injury. - Effects on Lipid Handling
Tirzepatide improves cholesterol and triglyceride levels. Lower triglycerides in the blood may reduce delivery of fat to the liver.
What This Means for Patients
While weight loss remains the main driver of improvement, tirzepatide likely offers additional benefits. This means that even patients who lose less weight than expected might still see liver health gains. For example, a person who loses only 5% of body weight may still experience a larger drop in liver fat or ALT levels than would normally occur with lifestyle changes alone.
However, it is important to be realistic. The strongest and most consistent liver benefits still come with larger weight reductions. In clinical studies, people who achieved 10–15% weight loss saw the most dramatic improvements in steatosis and inflammation. Fibrosis improvement, which is harder to achieve, usually requires both weight loss and time on therapy.
For clinicians, this evidence means tirzepatide should be thought of as both a weight-loss therapy and a possible liver-targeting treatment. While we cannot yet say it directly “treats NASH” outside of clinical trials, it is fair to recognize that tirzepatide’s liver effects go beyond the scale.
For patients, the message is clear: losing weight with tirzepatide is extremely helpful for fatty liver, but even small improvements in weight may come with additional liver health benefits. Still, lifestyle steps such as healthy eating, exercise, and avoiding alcohol remain key partners in treatment.
Who Is a Candidate? Eligibility, Contraindications, and Precautions
When we talk about using tirzepatide for fatty liver disease, an important question is: Who should actually take it? Not every patient with fatty liver is a good candidate. Doctors must weigh potential benefits against possible risks. In this section, we will look closely at eligibility, safety concerns, and special precautions for different patient groups.
Appropriate Patient Profiles
Tirzepatide was first approved for type 2 diabetes and later for obesity management. Both of these conditions are strongly linked to fatty liver disease. Because of that overlap, the “ideal” candidate is usually someone who has:
- Obesity (BMI ≥30), or overweight (BMI ≥27) with weight-related problems such as fatty liver, high blood pressure, or high cholesterol.
- Type 2 diabetes, which often worsens liver fat and inflammation.
- Metabolic syndrome, meaning a cluster of conditions like large waist size, insulin resistance, high triglycerides, or low HDL cholesterol.
These are the groups where the clinical trials have shown the strongest benefit. Weight loss from tirzepatide, combined with improved insulin sensitivity, can reduce fat buildup in the liver and lower inflammation.
Contraindications: When Tirzepatide Should Not Be Used
There are certain situations where tirzepatide is not recommended at all. These are called contraindications, meaning the risks are considered too high. Current guidance highlights the following:
- History of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN2). Tirzepatide, like other drugs in this class, carries a boxed warning about thyroid tumors in animal studies. Even though this has not been proven in humans, anyone with a personal or family history of these cancers should avoid it.
- Prior serious reaction to tirzepatide or its ingredients. Severe allergic reactions are rare, but they can happen.
- Pregnancy and breastfeeding. Safety has not been established in these groups. Because weight loss drugs can affect fetal growth, they are not recommended during pregnancy.
Precautions: Situations That Require Extra Care
Even if a patient does not fall into the strict contraindication list, doctors still need to be careful with some groups. These are situations where tirzepatide may be used, but with closer monitoring:
- History of pancreatitis. While a clear link has not been proven, incretin-based drugs have been associated with cases of pancreatitis. Patients with past pancreatitis should be counseled and monitored.
- Gallbladder disease. Rapid weight loss increases the risk of gallstones, which can also affect the liver and bile ducts.
- Severe gastrointestinal problems. Since tirzepatide slows stomach emptying, people with gastroparesis or severe gut issues may struggle with side effects like nausea, vomiting, or abdominal pain.
- Kidney disease. Tirzepatide itself is not directly harmful to the kidneys, but dehydration from vomiting or diarrhea can worsen kidney function. People with moderate to severe kidney disease need hydration monitoring.
- Liver disease. In compensated cirrhosis (where the liver is scarred but still functioning), tirzepatide may still be considered. In decompensated cirrhosis (where there are complications like ascites, varices, or encephalopathy), safety data are lacking and it should generally be avoided.
Use in Older Adults
Many people with fatty liver disease are older, and age brings additional health concerns. Clinical studies suggest tirzepatide works in older adults, but side effects like gastrointestinal upset or weight loss–related frailty may be more noticeable. Doctors often start at the lowest dose and titrate very carefully in this group.
Renal and Hepatic Impairment
- Renal impairment: No dose adjustment is required for mild to moderate kidney disease, but close monitoring for dehydration and lab changes is advised.
- Hepatic impairment: In mild liver disease, tirzepatide can be used without dose adjustment. In advanced liver disease, evidence is still limited, so decisions must be individualized.
Special Populations
- Patients without diabetes: People who have fatty liver but no diabetes may still benefit from tirzepatide if they are obese. Clinical trials show liver fat reduction in this group too. The challenge is usually cost and insurance approval rather than safety.
- Women of childbearing age: Effective birth control should be discussed because the drug is not safe in pregnancy. A washout period before conception is generally recommended.
- Patients with multiple medications: Because tirzepatide delays stomach emptying, it may affect absorption of some oral drugs (for example, antibiotics or thyroid medication). Doctors sometimes adjust timing of doses or monitor drug levels more closely.
The best candidates for tirzepatide are adults with obesity and/or type 2 diabetes who also have fatty liver disease. Contraindications are limited but important to remember—especially thyroid cancer history and pregnancy. Many other patients can use tirzepatide safely, but careful monitoring is needed if they have advanced liver disease, kidney problems, or other chronic health issues. Doctors individualize treatment by balancing benefits for the liver against possible risks in each patient.
What Dose, and How Is It Titrated for Liver Benefits?
When doctors prescribe tirzepatide, they do not start at the highest dose right away. Instead, they follow a step-by-step process called dose titration. This method helps the body adjust slowly, reduces side effects, and makes it easier for patients to stay on the medicine long term. For people with fatty liver disease, the same rules apply. Let’s break this down in detail.
Standard Dosing Schedule
Tirzepatide is available in different weekly doses: 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg. The general schedule looks like this:
- Start low: Patients usually begin with 2.5 mg once a week.
- Gradual increase: After 4 weeks, the dose is usually raised to 5 mg once a week.
- Step up every 4 weeks: If tolerated, the dose is then increased by 2.5 mg every 4 weeks (for example, from 5 mg to 7.5 mg, then to 10 mg, and so on).
- Target dose: Many patients end up at 10 mg, 12.5 mg, or 15 mg, depending on their weight loss goals, side effects, and response.
This slow rise in dose gives the gut and nervous system time to adjust. Because nausea, vomiting, and diarrhea are common at the beginning, titration is key to making the treatment sustainable.
Why the Dose Matters for Fatty Liver
The main way tirzepatide helps fatty liver is by reducing body weight and improving insulin resistance. Research shows that greater weight loss leads to greater improvements in liver fat and inflammation. Higher doses of tirzepatide (such as 10–15 mg weekly) generally produce the strongest weight loss.
- Liver fat reduction: MRI scans show that people on higher doses often see larger drops in liver fat percentage compared to those on lower doses.
- NASH improvement: In early studies, doses of 10–15 mg were linked to more frequent resolution of NASH features such as ballooning and inflammation.
- Fibrosis signals: While results are still developing, higher doses may also have stronger effects on slowing or improving fibrosis.
That said, not everyone can tolerate the top dose, and not everyone needs it. Even moderate doses (like 7.5 or 10 mg) can lead to meaningful improvements in liver fat, especially if combined with lifestyle changes.
When to Slow Down or Hold the Dose
Not all patients move smoothly up the titration ladder. Doctors may decide to hold at a lower dose for a longer period if:
- Side effects are strong: Persistent nausea, vomiting, diarrhea, or abdominal discomfort.
- Weight loss is already significant: If someone is meeting health goals at 7.5 or 10 mg, there may be no need to push to 15 mg.
- Underlying health issues: Conditions like kidney disease or dehydration risk may make higher doses less safe.
It is important for patients to communicate openly with their care team. In some cases, the dose can be reduced if side effects are too bothersome.
Practical Tips for Titration Success
- Consistency: Take the injection on the same day each week. Missing doses can cause stomach upset when restarting.
- Hydration: Drinking enough fluids helps reduce nausea and protects kidney function.
- Food choices: Small, frequent meals and avoiding greasy or fried food can help with GI side effects.
- Patience: Benefits for liver fat usually appear after months of consistent dosing. It is not an overnight fix.
How Dose Relates to Liver Outcomes
Doctors and researchers believe that the liver benefits of tirzepatide are dose-dependent. This means that the more effective the dose is for weight loss, the more likely it will reduce fat in the liver and improve other liver markers. However, it is not only about dose—it is also about time.
- Short-term (weeks to months): Lower ALT and AST levels often improve even at mid-level doses.
- Medium-term (6–12 months): MRI and elastography studies show significant liver fat reduction, especially at higher doses.
- Long-term (beyond 1 year): The goal is not just liver fat reduction, but histologic changes—resolution of NASH and possible improvement in fibrosis. These outcomes are most likely with sustained high-dose therapy plus weight loss.
Balancing Benefits and Tolerability
The art of tirzepatide dosing is finding the “sweet spot” between maximum liver and metabolic benefits and tolerable side effects. For some, that is 15 mg weekly. For others, it may be 7.5 or 10 mg. Importantly, there is no one-size-fits-all dose. The treatment must be personalized.
Safety Profile in People With Fatty Liver
When doctors think about prescribing tirzepatide for people with fatty liver disease, one of the most important questions is safety. Because people with NAFLD (nonalcoholic fatty liver disease) or NASH (nonalcoholic steatohepatitis) often have other health problems—like diabetes, obesity, or high blood pressure—it is important to understand how safe this medicine is for them. Below, we look at what the research shows about side effects, how common they are, and what to watch for.
Common Side Effects
The most frequent side effects of tirzepatide involve the stomach and intestines. These are called gastrointestinal (GI) side effects. They include:
- Nausea: Many people feel queasy when they first start the medicine. This usually improves after a few weeks.
- Vomiting: Some patients may vomit, especially when the dose is increased.
- Diarrhea: Loose stools are common but usually mild.
- Constipation: Some patients have the opposite problem and feel constipated.
These effects tend to happen during the first few weeks of therapy or after the dose is raised. Doctors often manage them by increasing the dose more slowly, encouraging patients to eat smaller meals, and staying hydrated. For most people, these symptoms lessen with time.
Less Common but Important Risks
There are other risks that are less common but worth noting:
- Gallbladder problems: Rapid weight loss, which tirzepatide can cause, increases the risk of gallstones. Gallstones may lead to gallbladder pain or inflammation.
- Pancreatitis: A small number of patients taking medicines in this drug family have had inflammation of the pancreas. The warning signs are severe stomach pain, often radiating to the back, sometimes with vomiting. This is rare but serious.
- Low blood sugar (hypoglycemia): Tirzepatide itself rarely causes low blood sugar unless it is combined with medicines like sulfonylureas or insulin. If a patient is taking these, their doctor may need to lower the dose.
- Hair thinning: Some people report temporary hair loss during rapid weight loss. This is usually related to nutritional changes rather than the medicine itself, but it can still be distressing.
- Kidney stress: Dehydration from vomiting or diarrhea can temporarily affect kidney function. Patients with kidney disease need close monitoring.
Safety for the Liver
Because patients with fatty liver are already concerned about their liver health, it is natural to ask: Is tirzepatide safe for the liver itself?
Research so far suggests it is. In fact, most studies show improvements in liver enzymes such as ALT (alanine aminotransferase) and AST (aspartate aminotransferase), which are markers of liver injury. Some trials show that as liver fat decreases, these enzyme levels also drop.
Rare cases of liver problems have been reported in people taking GLP-1–related drugs, but there is no clear evidence that tirzepatide directly harms the liver. Doctors still recommend checking blood tests regularly—especially if the patient has advanced fibrosis or cirrhosis.
Drug Interactions and Special Considerations
- Other diabetes medications: As mentioned, tirzepatide may cause low blood sugar if combined with insulin or sulfonylureas. Dose adjustments help prevent this.
- Blood pressure and cholesterol drugs: Most people take these safely alongside tirzepatide. In fact, blood pressure and cholesterol often improve as patients lose weight.
- Cirrhosis: People with early, compensated cirrhosis (where the liver still works well) may be able to use tirzepatide, but there is little research in advanced, decompensated cirrhosis. For these patients, safety is less certain, and careful monitoring is needed.
- Other conditions: Tirzepatide should not be used in people with a personal or family history of medullary thyroid cancer or MEN2 syndrome. Pregnant or breastfeeding women should also avoid it.
Monitoring Safety Over Time
Doctors usually recommend a clear safety plan for patients on tirzepatide who also have fatty liver:
- Before starting: Check weight, blood sugar, HbA1c, kidney function, and liver enzymes.
- During treatment: Recheck liver enzymes, kidney function, and weight every few months.
- If symptoms appear: Severe abdominal pain, yellowing of the skin or eyes, or unexplained fatigue should be checked immediately.
Most patients tolerate tirzepatide well, especially if the dose is increased gradually. Still, ongoing follow-up is key to catching rare but serious problems early.
Tirzepatide is generally safe for people with fatty liver, but side effects are common at the start, especially stomach upset. Most improve with time. Less common risks include gallstones, pancreatitis, and dehydration-related kidney stress. Importantly, evidence so far shows that tirzepatide does not damage the liver and may actually improve liver enzyme levels as fat in the liver decreases. Careful monitoring and open communication between patient and doctor help make treatment both safe and effective.
Can People Without Diabetes Use Tirzepatide for Fatty Liver?
Tirzepatide was first approved for people with type 2 diabetes. Later, it gained approval for obesity treatment in certain countries, even for those without diabetes. Because fatty liver disease (NAFLD or NASH) is very common in people who are overweight but do not have diabetes, a key question is whether tirzepatide can also help this group. This section looks closely at the evidence, the science, and the real-world issues for people without diabetes who may want to use tirzepatide to improve liver health.
Evidence in People Without Diabetes
Several clinical trials have tested tirzepatide in people who are overweight or obese but do not have diabetes. These studies show strong effects on weight loss and body fat reduction, which are directly linked to improvements in fatty liver.
- Liver Fat Reduction: Imaging studies such as MRI-PDFF (a scan that measures liver fat) show that tirzepatide can cut down liver fat by 30% or more in some participants without diabetes. These reductions are much greater than lifestyle changes alone in most studies.
- Liver Enzymes: Blood tests like ALT and AST, which signal liver inflammation, also improve in people without diabetes. Lower liver enzymes suggest reduced liver stress and damage.
- Histology (Tissue Data): Early biopsy data are limited, but results hint that tirzepatide may improve inflammation and ballooning injury in the liver. Whether it can reverse scar tissue (fibrosis) is still under study, and long-term trials are ongoing.
In short, while most research started with people with diabetes, newer studies confirm that people without diabetes can also see strong liver improvements.
Why Might Non-Diabetics Benefit?
Even without diabetes, many people with fatty liver share the same root problems: insulin resistance, excess body weight, and fat buildup in the liver. Tirzepatide tackles these problems in several ways:
- It reduces appetite and calorie intake, leading to significant weight loss.
- It improves how the body responds to insulin, lowering fat storage in the liver.
- It reduces fat release from adipose tissue (body fat) into the bloodstream, which decreases the burden on the liver.
Because of these effects, benefits in fatty liver disease are not limited to those with diabetes.
Insurance and Regulatory Status
One of the biggest hurdles is not the science but the practical side: access.
- For Diabetes: Tirzepatide is widely covered for people with type 2 diabetes.
- For Obesity: Coverage varies by country and health plan. In some places, tirzepatide is approved for weight loss even without diabetes, but insurers may require a certain body mass index (BMI) or obesity-related condition (such as sleep apnea or high blood pressure).
- For Fatty Liver Alone: Right now, tirzepatide is not officially approved just for NAFLD or NASH. This means doctors prescribe it “off-label” if the main reason is liver health, and insurance may not cover it. Patients often need another qualifying diagnosis, like obesity or diabetes, for coverage.
This creates gaps where people without diabetes but with fatty liver may benefit medically but face challenges paying for the treatment.
Ethical and Practical Considerations
There are important questions when prescribing tirzepatide for people without diabetes:
- Fair Access: If only those with diabetes or obesity qualify for insurance coverage, people with fatty liver but normal weight or blood sugar may be left out.
- Risk–Benefit Balance: Doctors need to weigh potential liver improvements against risks such as side effects (nausea, vomiting, gallbladder problems). For some patients with early fatty liver, lifestyle therapy alone may still be the first approach.
- Equity in Health Care: Fatty liver is common across all backgrounds, but access to advanced medications often depends on income, insurance, and geography. This raises fairness issues.
What Does This Mean for Patients Without Diabetes?
For someone without diabetes who has fatty liver disease:
- Yes, tirzepatide can work. Evidence shows it lowers liver fat, improves enzymes, and may reduce inflammation.
- It is not yet an official liver drug. Doctors use it mainly for obesity or diabetes, and any liver benefit is considered a bonus.
- Coverage may be limited. Many people may need to pay out of pocket unless they meet obesity or diabetes criteria.
- Lifestyle is still key. Even with tirzepatide, diet, exercise, and alcohol reduction remain the foundation of fatty liver treatment.
People without diabetes can benefit from tirzepatide if they have fatty liver disease, especially if they are also overweight or obese. The improvements are real and supported by growing research. However, the drug is not yet officially labeled for fatty liver alone, and insurance coverage may be a major barrier. More clinical trials are underway, and in the future, tirzepatide may become a standard option for treating fatty liver disease in both diabetic and non-diabetic patients.
How Do You Monitor Progress on Tirzepatide?
When someone starts tirzepatide for fatty liver disease, it is important to know how to track progress. This does not only mean checking if the person is losing weight. It also includes checking liver health, blood work, and other signs of improvement. Careful monitoring helps both patients and doctors see if the medicine is working, if side effects are appearing, and when to adjust treatment.
Below is a step-by-step explanation of what should be done before starting, during treatment, and in follow-up.
Baseline Workup Before Starting Tirzepatide
Before beginning tirzepatide, the doctor usually performs a full health check. This gives a starting point to compare with later results. Common parts of this workup include:
- Body measurements: Weight, body mass index (BMI), and waist size are recorded. Waist size is important because central obesity (fat around the stomach) is strongly linked to fatty liver.
- Blood sugar and diabetes tests: Hemoglobin A1C, fasting glucose, or an oral glucose tolerance test may be used. Even people without known diabetes are checked because many with fatty liver have insulin resistance.
- Liver enzymes: Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are the main liver enzymes measured. High levels suggest liver irritation or inflammation.
- Lipid panel: Cholesterol and triglycerides are tested since fatty liver is closely tied to abnormal blood fats.
- Fibrosis scores: Non-invasive scores like FIB-4 or NAFLD fibrosis score can help estimate whether liver scarring is mild, moderate, or advanced.
- Imaging: In some cases, liver ultrasound, FibroScan (elastography), or MRI-PDFF (magnetic resonance imaging to measure fat fraction) may be ordered. These give a clearer picture of how much fat and stiffness is present in the liver.
This baseline evaluation helps doctors later decide if tirzepatide is having a positive effect.
Monitoring During Treatment
Once tirzepatide has started, the follow-up schedule is important. Monitoring is usually broken into early visits and long-term visits.
Early follow-up (first 3–6 months):
- Weight and waist measurements: Checked at every visit, often every 4–12 weeks, especially while the dose is being increased.
- Liver enzymes: ALT and AST are re-checked at similar intervals. A steady fall in these numbers usually shows liver stress is improving.
- Blood sugar and A1C: Especially for patients with diabetes, to ensure glucose levels are stable and safe.
- Tolerability: Questions about nausea, vomiting, constipation, or other gastrointestinal issues help guide dose adjustments.
Longer-term follow-up (6–12 months and beyond):
- Repeat imaging: If available, MRI-PDFF or elastography may be done after 6–12 months to measure changes in liver fat and stiffness. Ultrasound can also help, though it is less precise.
- Cardiometabolic health: Blood pressure, cholesterol, and triglycerides are checked, since tirzepatide also helps improve overall metabolic health.
- Medication review: Any other drugs the patient is taking (for example, statins or antihypertensives) are reviewed to avoid interactions and to see if doses can be reduced as health improves.
Defining What Counts as Progress
Progress on tirzepatide can be defined in several ways:
- Weight loss goals: Research shows that losing 7–10% of body weight can significantly reduce liver fat. Tirzepatide often achieves more than this, so meeting that threshold is a strong sign of benefit.
- Improvement in liver enzymes: ALT and AST moving back into the normal range is a good sign, though not perfect, since some people with NASH have normal enzymes despite ongoing disease.
- Non-invasive fibrosis markers: Lower scores on FIB-4 or NAFLD fibrosis score suggest less stress on the liver.
- Imaging results: A meaningful drop in liver fat percentage (for example, MRI-PDFF showing ≥30% relative reduction) is considered a marker of histological improvement in trials.
Doctors usually combine all these measures rather than relying on a single test.
When to Consider a Liver Biopsy or Specialist Referral
In most cases, patients with fatty liver can be monitored with blood tests and imaging alone. However, a liver biopsy may be considered if:
- There is uncertainty about the stage of disease.
- Non-invasive tests give conflicting results.
- The patient is not improving despite treatment.
- Clinical trials require histology as an endpoint.
Referral to a liver specialist (hepatologist) is also important if there are signs of advanced scarring, cirrhosis, or complications such as ascites, jaundice, or varices.
Monitoring progress on tirzepatide is not just about numbers on the scale. It is about a complete picture: weight changes, blood tests, imaging, and overall health. For most patients, visits every 2–3 months in the first year give enough information to guide therapy. Over time, follow-up may shift to every 6–12 months if the patient is stable and doing well.
By carefully tracking these markers, doctors can see whether tirzepatide is truly helping the liver and lowering future risk of cirrhosis and other complications. For patients, this clear structure of check-ins and tests provides reassurance and motivation to continue both the medicine and healthy lifestyle habits.
Combining Tirzepatide With Lifestyle and Cardiometabolic Care
Treating fatty liver disease, whether it is NAFLD or NASH, is not only about one medicine. Even though tirzepatide shows strong promise, the best results come when it is combined with healthy lifestyle habits and overall care for the heart and metabolism. This section explains how diet, exercise, alcohol use, sleep, and other medical treatments can work together with tirzepatide to improve liver and whole-body health.
Diet Quality and Calorie Goals
Food is the main driver of weight gain and fat buildup in the liver. Tirzepatide helps reduce appetite, but patients still need to make smart food choices. Research shows that a steady calorie deficit is needed to lose weight and reduce liver fat. Most people benefit from cutting about 500–750 calories a day, but this should be tailored to the individual.
- Balanced diet: A Mediterranean-style diet, rich in vegetables, fruits, whole grains, beans, fish, nuts, and olive oil, is strongly linked with better liver health.
- Low sugar intake: Reducing added sugars, especially from soda, fruit juices, and desserts, lowers fat made by the liver.
- Portion control: Tirzepatide may naturally reduce portion sizes, but planning meals ahead can prevent overeating.
Protein Intake and Muscle Protection
One risk during weight loss is losing muscle along with fat. Patients with fatty liver especially need to protect muscle, because muscles help control blood sugar and metabolism. Aiming for 1.0–1.5 grams of protein per kilogram of body weight per day can help preserve lean tissue. Protein sources like chicken, fish, beans, eggs, and Greek yogurt are helpful. Combining protein with resistance exercise is even more effective.
Exercise and Physical Activity
Exercise works in several ways. It burns calories, helps weight loss, and directly improves how the liver uses fat and sugar. Even without weight loss, exercise can lower liver enzymes and reduce liver fat.
- Aerobic activity: Walking, cycling, or swimming for at least 150 minutes per week is recommended.
- Resistance training: Lifting weights or using resistance bands 2–3 times a week preserves muscle mass and supports fat loss.
- Daily movement: Taking the stairs, standing more, and breaking up long sitting periods also matter.
When combined with tirzepatide, exercise can enhance weight loss and protect against muscle loss, helping the liver recover more effectively.
Alcohol and the Liver
Even moderate alcohol use can worsen fatty liver and increase the risk of inflammation and scarring. For people with NAFLD or NASH, most liver specialists recommend avoiding alcohol completely or drinking only rarely. Tirzepatide does not interact strongly with alcohol, but alcohol cancels out many of the liver benefits of weight loss and medication.
Sleep and Stress Management
Poor sleep and high stress raise insulin resistance and make it harder to lose weight. They can also raise cravings for high-calorie food. Patients using tirzepatide should aim for 7–9 hours of quality sleep per night. Stress-reducing activities like mindfulness, breathing exercises, or yoga can help improve long-term success in both weight loss and liver health.
Coordinating With Other Medications
Most people with fatty liver also have other conditions such as diabetes, high blood pressure, or high cholesterol. These increase the risk of heart disease, which is the leading cause of death in NAFLD/NASH. Tirzepatide improves blood sugar and often lowers blood pressure and cholesterol indirectly through weight loss. But it is not a replacement for other medicines.
- Statins: Remain important for cholesterol and are safe in most people with fatty liver.
- Antihypertensives: Blood pressure medicines may still be needed even after weight loss.
- Other diabetes drugs: Some may be reduced if blood sugar improves too much with tirzepatide, so monitoring is important.
Tirzepatide should be seen as part of a team approach. The medicine helps reduce weight and appetite, but diet, exercise, and lifestyle choices strengthen its effect. By adding structured nutrition, regular activity, limited alcohol, better sleep, and careful coordination with other medical care, patients can maximize liver healing and lower their risk of diabetes, heart disease, and cirrhosis.
Tirzepatide is a powerful tool, but the foundation of treatment for fatty liver remains lifestyle change. When the two are combined, the chances of reversing fatty liver and protecting long-term health are much greater.
Evidence Roundup: What the Latest Trials and Real-World Data Show
The question most patients and doctors ask is simple: Does tirzepatide really work for fatty liver disease?
To answer that, we need to look closely at the published studies and early reports. Researchers have now tested tirzepatide in people with type 2 diabetes, obesity, and fatty liver. Some trials were designed for weight loss and blood sugar control, but they also measured liver health as secondary outcomes. Others are now focused directly on fatty liver (NAFLD and NASH).
Below is a summary of what we know from clinical trials, imaging studies, and real-world experience.
Study Designs: Who Was Studied and How
Most evidence comes from phase 2 and phase 3 clinical trials. These studies usually enrolled adults with obesity and/or type 2 diabetes. Many of these people also had fatty liver, since the two conditions often go together.
- Duration: Most trials lasted between 26 and 72 weeks (about 6 months to 1.5 years). That is long enough to see changes in liver fat and enzymes, but not always enough to measure long-term outcomes like cirrhosis prevention.
- Measurements: Different tools were used. MRI-PDFF (proton density fat fraction) is the gold standard for measuring liver fat on imaging. Blood tests such as ALT and AST show liver injury. Some studies also used elastography (a type of ultrasound) to estimate stiffness, which is linked to fibrosis. A few studies even included liver biopsies, which remain the most direct way to study inflammation and fibrosis.
Liver Fat Reduction: Strong and Consistent
One of the most consistent findings is that tirzepatide reduces liver fat.
- Magnitude of reduction: Across studies, MRI-PDFF showed reductions of 8–12 percentage points in absolute liver fat content. In many cases, this translated into a 30–50% relative drop from baseline.
- Speed: Improvements in liver fat could be seen within 12–24 weeks, with greater reductions over a year.
- Dose-response relationship: Higher doses of tirzepatide (10 mg and 15 mg) led to larger drops in liver fat compared to lower doses.
This is important because a reduction of more than 30% in liver fat is usually linked with higher odds of resolving NASH.
NASH Inflammation and Resolution
Reducing fat in the liver is only part of the story. NASH also involves inflammation and ballooning (injury to liver cells).
- Early biopsy data show that a significant proportion of patients on tirzepatide had NASH resolution without worsening fibrosis.
- In some reports, up to two-thirds of patients achieved this endpoint at higher doses, compared with much lower rates on placebo.
- This suggests tirzepatide not only reduces fat, but also calms inflammation inside the liver.
These findings are encouraging, though still based on trials that were not originally designed with NASH as the primary outcome.
Fibrosis: Signs of Improvement, But More Data Needed
Fibrosis (scar tissue in the liver) is the strongest predictor of long-term outcomes, including cirrhosis and liver failure.
- Non-invasive markers such as FIB-4 score, ELF score, and elastography suggest that tirzepatide may reduce fibrosis progression and sometimes even improve fibrosis stage.
- However, biopsy-confirmed fibrosis regression is less clear. The available studies were too short or too small to prove whether tirzepatide can reverse scarring.
- Larger, ongoing phase 3 trials are now enrolling patients specifically with biopsy-proven NASH and fibrosis. Results from these studies will tell us much more.
At this point, the best summary is that tirzepatide shows a signal for fibrosis benefit, but it is not yet conclusive.
Safety and Discontinuation
Across studies, tirzepatide was generally well tolerated. The most common side effects were gastrointestinal—nausea, vomiting, and diarrhea—especially during dose increases.
- Most side effects were mild to moderate and improved with time or slower dose escalation.
- Discontinuation rates due to side effects were relatively low (often under 10%).
- Importantly, no major liver-related safety problems were reported, even in people with fatty liver.
This safety profile supports continued research in NAFLD and NASH populations.
Real-World Data
Although clinical trials provide the highest quality evidence, early real-world reports are also valuable. Doctors using tirzepatide in obesity and diabetes clinics have noticed:
- Significant weight loss (15–20% of body weight in some cases).
- Parallel improvements in liver enzymes (ALT, AST).
- Reductions in non-invasive fibrosis scores.
These real-world outcomes mirror the trial data and add confidence that benefits are not limited to tightly controlled study environments.
Pipeline and Future Trials
Several dedicated trials are ongoing:
- SURMOUNT and SURPASS programs continue to provide obesity and diabetes data with liver endpoints.
- New phase 3 studies are enrolling patients with biopsy-proven NASH and moderate to advanced fibrosis. These trials will test whether tirzepatide can achieve FDA-accepted endpoints such as “NASH resolution without worsening fibrosis” and “fibrosis improvement without worsening NASH.”
- Results from these trials are expected in the next few years and may determine whether tirzepatide becomes an approved treatment for NASH.
Comparison to Usual Care
When compared with lifestyle interventions alone, tirzepatide clearly produces larger and more consistent liver fat reductions. While weight loss of 7–10% through diet and exercise can improve NAFLD, sustaining that amount is very difficult for most people. Tirzepatide offers a pharmacologic tool that can help more patients reach and maintain these levels of weight loss, and possibly gain additional direct benefits for the liver.
Practical Algorithm: Integrating Tirzepatide Into NAFLD/NASH Care Pathways
Managing fatty liver disease is not only about one medication. It requires a careful, step-by-step approach that brings together lifestyle changes, medical therapy, and regular follow-up. Tirzepatide can play an important role, but it must be added into a broader care plan. Below is a detailed guide on how doctors and patients can work together to use tirzepatide effectively for NAFLD (non-alcoholic fatty liver disease) and NASH (non-alcoholic steatohepatitis).
Step 1: Identify the Patient’s Risk and Disease Stage
The first step is making sure the diagnosis is correct and the severity of the disease is clear. Fatty liver disease can range from mild fat build-up in the liver (steatosis) to more advanced scarring (fibrosis or cirrhosis). Doctors often start with:
- Simple blood tests: liver enzymes like ALT and AST, as well as platelet counts.
- Non-invasive scores: tools such as FIB-4 or the NAFLD fibrosis score help estimate scarring.
- Imaging: ultrasound, elastography, or MRI-PDFF can measure fat and stiffness in the liver.
- Specialist input: in unclear cases or advanced disease, a hepatologist (liver specialist) may be involved.
By staging the disease, doctors can decide if tirzepatide may be a helpful addition, and also identify people who need closer monitoring.
Step 2: Begin With Lifestyle and Weight Management
Before or alongside any medication, lifestyle therapy is essential. Evidence shows that a weight loss of at least 7–10% of body weight can improve liver fat and even reduce inflammation and scarring. Key strategies include:
- Nutrition: balanced calorie reduction with focus on whole foods, reduced refined sugars, and adequate protein intake.
- Physical activity: regular aerobic exercise and resistance training to reduce fat and preserve muscle mass.
- Sleep and stress: poor sleep and high stress worsen metabolic health, so addressing these factors supports liver recovery.
- Alcohol limits: even though NAFLD is “non-alcoholic,” alcohol can still worsen liver injury and should be minimized.
Lifestyle care is the foundation. Tirzepatide works best when combined with these healthy changes.
Step 3: Add Tirzepatide When Appropriate
If lifestyle therapy alone does not achieve enough improvement, or if the patient has high risk factors such as type 2 diabetes or obesity, tirzepatide may be considered. Practical points include:
- Start low, go slow: tirzepatide is started at the lowest dose and increased step by step every 4 weeks, as tolerated.
- Tailor to the patient: higher doses may lead to more weight loss and greater liver fat reduction, but side effects may also increase.
- Pair with ongoing care: tirzepatide is not a substitute for lifestyle; it is a partner to it.
This step is usually led by an endocrinologist, hepatologist, or primary care provider who is familiar with obesity and diabetes medications.
Step 4: Monitor Efficacy and Safety Over Time
Monitoring progress ensures that treatment is safe and effective. The plan often includes:
- Weight checks: every visit, to track progress toward a 7–10% or more weight loss goal.
- Blood tests: liver enzymes, kidney function, and glucose or A1C levels every 3–6 months.
- Non-invasive scores or imaging: FIB-4, elastography, or MRI-PDFF after 6–12 months to assess liver changes.
- Side effect management: nausea, vomiting, or constipation are common early on; dose adjustments or dietary strategies can help.
If patients are not achieving weight or liver health goals after a reasonable trial, the care team may reassess the approach.
Step 5: Referral and Specialist Collaboration
For patients with advanced fibrosis, cirrhosis, or uncertainty in diagnosis, referral to hepatology is important. Collaboration ensures:
- Advanced monitoring: such as liver biopsy or specialized imaging.
- Management of complications: like varices, ascites, or liver cancer screening in cirrhosis.
- Multidisciplinary care: involving dietitians, diabetes educators, and cardiology when needed.
This team approach maximizes safety and outcomes.
Documentation and Communication
Clear documentation helps track goals and safety. Records should note:
- Starting weight and target weight loss.
- Baseline lab results and imaging findings.
- Dose and titration schedule of tirzepatide.
- Side effects and how they were managed.
- Patient education provided (diet, exercise, follow-up).
Communicating progress regularly with the patient and, if needed, with a broader care team ensures everyone is aligned.
Integrating tirzepatide into fatty liver treatment is not a “one-step cure.” It is a structured process that begins with risk assessment, builds on lifestyle change, adds medication when appropriate, and continues with careful follow-up. When used in this way, tirzepatide may significantly improve liver health, reduce fat and inflammation, and help patients lower their overall metabolic risk.
Access, Coverage, and Health-System Considerations
Tirzepatide has shown promise in reducing liver fat and helping patients with NAFLD and NASH. But medical progress does not help unless patients can actually access the drug. Cost, insurance coverage, and health system policies all play a major role in whether someone can start and stay on tirzepatide. This section looks at the practical realities of access and the wider system challenges.
Insurance Coverage and Indications
Right now, tirzepatide is approved in many regions for type 2 diabetes and, more recently, for obesity or weight management. However, it is not yet officially approved for NAFLD or NASH. That means insurers often will only cover it if the patient meets criteria for diabetes or obesity.
- Diabetes coverage: Most insurance plans will cover tirzepatide for patients with type 2 diabetes, especially if other treatments have not been effective.
- Obesity coverage: Coverage is more variable. Some plans pay for weight loss medications, while others exclude them. Where obesity medications are covered, insurers may require a certain body mass index (BMI), usually ≥30 kg/m² or ≥27 kg/m² with weight-related conditions such as hypertension, dyslipidemia, or sleep apnea.
- NAFLD/NASH coverage: Since these are not yet approved uses, patients with only fatty liver disease but without obesity or diabetes often face barriers. Doctors may prescribe tirzepatide “off-label,” but the cost may fall entirely on the patient.
Prior Authorization and Administrative Hurdles
Even when coverage is possible, patients often face extra paperwork and delays. Insurers typically require:
- Proof of diagnosis: Documentation of type 2 diabetes, obesity, or related conditions.
- Failed prior therapies: Some insurers require evidence that the patient tried other medications first, like metformin or older weight-loss drugs.
- Weight and health records: Recent weight, BMI, and sometimes liver test results.
This process is called prior authorization. It can take days to weeks and may involve appeals if coverage is denied. Both patients and clinics need to be prepared for these steps.
Out-of-Pocket Costs
Tirzepatide is expensive. In the United States, the list price can be several hundred to over one thousand dollars per month. For people without coverage, this cost is usually unaffordable. Even with insurance, patients may face co-pays or coinsurance charges that add up quickly.
Drug makers sometimes offer patient assistance programs or discount cards, but these may not apply if the patient is using tirzepatide for fatty liver rather than an approved use. In other countries with public health systems, coverage rules vary, and many agencies wait for stronger evidence before approving a new indication.
Cost-Effectiveness and System Impact
Health systems must also consider whether tirzepatide is worth the cost at a population level. NAFLD and NASH are extremely common, affecting millions of people worldwide. If even a fraction of those patients used tirzepatide, drug spending could rise sharply.
However, untreated NASH can progress to cirrhosis, liver failure, or cancer, which are very expensive to manage. Early treatment that prevents progression could save money in the long run. For this reason, cost-effectiveness studies are underway to compare the drug’s price with potential savings from fewer hospitalizations, transplants, and complications.
Health Equity and Disparities
Another key issue is equity. NAFLD and NASH are more common in certain communities, including people with lower income, limited access to healthy food, or fewer opportunities for physical activity. Unfortunately, these same groups often face the greatest barriers to expensive new medications.
- Insurance gaps: Patients without good insurance may never be offered tirzepatide.
- Geography: In rural areas or low-resource clinics, providers may not have the capacity to navigate complex prior authorization processes.
- Language and cultural barriers: Patients may not be fully informed about treatment options if health education is not available in their language or tailored to their needs.
Health systems must address these gaps to prevent new therapies from widening health inequalities.
Practical Tips for Clinicians and Patients
- Clarify indications early: If a patient has diabetes or obesity, emphasize this in documentation, since it increases the chance of coverage.
- Prepare records: Collect weight history, A1C levels, liver enzyme tests, and notes on lifestyle attempts. Having these ready speeds prior authorization.
- Explore assistance programs: Patients should ask about manufacturer savings cards or nonprofit programs that reduce out-of-pocket costs.
- Monitor policy updates: As clinical trial evidence grows, guidelines and insurance coverage may expand to include NAFLD or NASH indications. Keeping up to date is important.
The future of access to tirzepatide for liver disease depends on regulatory approvals, trial results, and health system policies. If upcoming studies confirm that tirzepatide not only reduces liver fat but also improves fibrosis and prevents cirrhosis, insurance coverage is likely to expand. Policymakers and insurers will then face the challenge of balancing high drug costs against the long-term benefits of preventing liver-related deaths.
Limitations of the Current Evidence and Research Gaps
Tirzepatide is one of the most promising new drugs for obesity, type 2 diabetes, and possibly fatty liver disease. Early research shows it can lower liver fat and improve liver health markers. But the science is still new, and many questions remain unanswered. It is important to understand what the studies so far can and cannot tell us, so patients and doctors keep realistic expectations. Below are the main gaps and limitations in the current evidence.
Duration of Studies and Long-Term Outcomes
Most of the clinical trials of tirzepatide for fatty liver have lasted less than 1 to 2 years. This time frame is long enough to measure changes in liver fat by imaging or lab tests, but it is not long enough to show whether the drug prevents the most serious liver outcomes.
For example:
- We do not yet know if tirzepatide lowers the risk of cirrhosis (advanced scarring of the liver).
- We do not know if it prevents liver failure, liver cancer, or the need for a transplant.
- Cardiovascular and kidney benefits are better documented, but liver-specific survival data are still missing.
Because NAFLD and NASH develop slowly, long-term studies of 5 to 10 years will be needed to confirm whether tirzepatide changes the natural history of the disease.
Reliance on Imaging and Blood Markers Instead of Biopsy
Many studies use MRI-based scans, ultrasound elastography, or blood tests like ALT, AST, or fibrosis scores to measure improvement. These tools are very useful, but they do not always match perfectly with liver biopsy results, which remain the gold standard for diagnosis.
The challenge is that:
- Liver biopsies are invasive, carry risks, and are not practical for every patient.
- Non-invasive tests may overestimate or underestimate improvement in inflammation or fibrosis.
- It is still unclear how well changes in MRI liver fat percentage predict long-term clinical outcomes.
This means we need more biopsy-based studies to confirm the true effects of tirzepatide on liver inflammation and scarring.
Uncertainty About Fibrosis Reversal
The most important goal in NASH treatment is not just lowering fat but also reducing fibrosis. Fibrosis stage is the strongest predictor of who will develop cirrhosis and liver complications.
Current data suggest tirzepatide may improve some fibrosis scores and biomarkers, but hard evidence of fibrosis reversal on biopsy is still very limited. Most studies have been too short or too small to show a clear, consistent benefit. Until more data are available, we cannot say with confidence that tirzepatide reverses fibrosis in the way some other experimental drugs aim to do.
Weight Loss Versus Direct Liver Effects
One of the biggest questions is whether tirzepatide’s liver benefits are simply due to weight loss, or if the drug has direct effects on liver biology.
- Weight loss itself can improve fatty liver in many patients, sometimes even leading to remission.
- Tirzepatide causes large weight reductions, which explains much of its benefit.
- Some studies hint at liver improvements beyond what would be expected from weight loss alone, but this is not fully proven.
More research is needed to separate weight-related improvements from drug-specific liver effects.
Patient Diversity and Representation
Most clinical trials so far have focused on people with obesity and type 2 diabetes. But NAFLD and NASH also affect people without diabetes, different ethnic groups, and patients at different stages of liver disease.
Key gaps include:
- Limited data in non-diabetic patients.
- Limited data in people with advanced fibrosis or cirrhosis.
- Uncertainty about how well results apply across racial and ethnic groups, who may have different risks for liver progression.
Future trials need broader, more diverse populations to confirm tirzepatide’s benefits apply to all groups.
Combination Therapies
Fatty liver is a complex disease that may need more than one type of therapy. Some drugs target fibrosis directly, while others work on inflammation or metabolism. Right now, we do not know how tirzepatide might combine with other liver-directed therapies.
- Could tirzepatide enhance the effects of antifibrotic drugs?
- Could lower doses of several drugs work better than high doses of one?
- Are there safety concerns with drug combinations?
These are important questions that future studies must answer.
Real-World Adherence and Long-Term Tolerability
Clinical trials take place under very controlled conditions, with frequent follow-up and strong patient support. Real life is different.
- Gastrointestinal side effects may cause some patients to stop the drug.
- The cost of tirzepatide may limit long-term use for many people.
- We do not yet know what happens when patients stop the drug—whether liver fat and inflammation return quickly, as happens with weight regain after stopping treatment.
Real-world data will help clarify how effective and sustainable tirzepatide is outside of clinical trials.
Research Gaps Moving Forward
In summary, here are the key areas where research is still needed:
- Long-term outcomes on cirrhosis, liver cancer, and survival.
- More biopsy-based evidence of fibrosis reversal.
- Clear separation of weight-loss effects from drug-specific liver effects.
- Trials in non-diabetic, advanced fibrosis, and diverse ethnic groups.
- Studies testing tirzepatide in combination with other emerging liver drugs.
- Real-world adherence and outcomes data over many years.
Tirzepatide has opened a new chapter in the treatment of fatty liver disease, but it is not the final answer. While early results are very encouraging, the science is still building. Patients, doctors, and researchers must continue to follow the evidence as larger and longer studies are published. Only then will we know whether tirzepatide can truly change the future of NAFLD and NASH.
Key Takeaways for Clinicians and Patients
As research grows around tirzepatide and fatty liver disease, the amount of data can feel overwhelming. This section brings the evidence together into clear, practical points. It highlights what tirzepatide does well, what remains uncertain, and how both doctors and patients can use this knowledge today.
Tirzepatide Can Lower Liver Fat
One of the strongest and most consistent findings is that tirzepatide reduces liver fat. Studies using imaging, such as MRI scans, show that patients can lose a significant portion of fat stored in the liver within months of treatment. This matters because excess liver fat is the starting point for NAFLD and the driver of inflammation and scarring that can follow. The degree of improvement depends on the dose, the duration of treatment, and the patient’s baseline health. Larger weight loss usually means a bigger drop in liver fat, but even moderate improvements can have health benefits.
Improvements in Liver Enzymes Happen Early
Liver enzymes such as ALT and AST are simple blood markers used to track liver injury. In many patients, tirzepatide brings these numbers down within weeks to months. While liver enzymes are not perfect measures, lower levels suggest less ongoing liver stress. For patients and doctors, this is an encouraging and easy-to-monitor signal that treatment is working.
Benefits Go Beyond the Liver
Tirzepatide was first developed for type 2 diabetes and obesity. Its effects on blood sugar, weight, blood pressure, and cholesterol are already well documented. For patients with NAFLD or NASH, these “extra” effects matter. People with fatty liver disease often die from heart disease, not directly from liver complications. By improving metabolic health as a whole, tirzepatide can lower overall risks in addition to improving the liver itself.
Evidence for NASH and Fibrosis Is Promising but Incomplete
While there is strong evidence for reducing liver fat, data on NASH inflammation and fibrosis are still limited. Some studies show signals that tirzepatide may help resolve steatohepatitis (the active inflammation that defines NASH) and may slow or even improve fibrosis. However, most results come from shorter-term studies or trials that were not designed to directly prove fibrosis reversal. Larger and longer-term trials are ongoing. Until those results arrive, we should view tirzepatide as a promising but not yet proven antifibrotic therapy.
Weight Loss Is a Key Driver
The most reliable predictor of liver improvement is weight loss. With tirzepatide, patients often lose 15–20% of their body weight, which is higher than with most other available drugs. This level of weight loss is enough to change the course of fatty liver disease in many people. Still, not every effect is explained by weight loss alone. Tirzepatide also improves insulin resistance, reduces fat in tissues outside the liver, and lowers inflammation—all of which likely contribute to liver health.
Safety Profile Matches What Is Already Known
In people with fatty liver disease, the safety profile of tirzepatide looks similar to what has been seen in people with diabetes or obesity. The most common issues are gastrointestinal: nausea, diarrhea, and constipation. These usually improve with time and careful dose escalation. More serious side effects, such as gallbladder disease or pancreatitis, are uncommon but possible. Overall, most patients tolerate the drug well. Regular monitoring of weight, blood sugar, kidney function, and liver enzymes is recommended.
Not Everyone Is a Candidate
Tirzepatide is not suitable for all patients. It is generally not used in people with a history of medullary thyroid cancer, multiple endocrine neoplasia type 2, or severe gastrointestinal disease. Its safety in advanced cirrhosis is not fully established. Pregnant and breastfeeding women should not take it. For now, it is best suited for adults with obesity and/or type 2 diabetes who also have evidence of NAFLD or NASH.
Monitoring Matters
Both clinicians and patients should set clear goals and track progress. At the start, this includes weight, waist size, blood sugar, cholesterol, liver enzymes, and non-invasive fibrosis scores like FIB-4. Over time, changes in these markers show whether tirzepatide is working. Imaging tests, such as FibroScan or MRI-PDFF, can be considered every 6–12 months if available. Regular monitoring also helps detect rare safety issues early.
Lifestyle Support Remains Essential
Tirzepatide is powerful, but it is not a cure on its own. Best results come when it is combined with healthy eating, physical activity, and management of other health risks. Even modest lifestyle changes, like reducing alcohol intake, improving diet quality, and increasing activity, can multiply the benefits of medication.
Conclusion: Where Tirzepatide Stands Today in NAFLD/NASH Care
Tirzepatide has quickly gained attention not only as a powerful medicine for type 2 diabetes and weight management but also as a possible new tool for fatty liver disease. The past several years have shown that losing weight and improving metabolic health are central to reversing nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). Tirzepatide works by helping people achieve significant and sustained weight loss, but it may also have direct effects on liver fat, inflammation, and insulin resistance. Together, these changes may reduce the progression of liver disease and even lead to measurable improvements in the liver itself.
The strongest evidence we have so far shows that tirzepatide can reduce liver fat content, which can be seen on advanced imaging like MRI scans. In many studies, patients reached reductions in liver fat of 20 to 30 percent or more within several months of treatment, which is a meaningful change. This reduction is most likely the first step toward reversing fatty liver disease. Alongside fat reduction, liver enzymes such as ALT and AST often improve, suggesting less stress and injury to liver cells. These improvements are important but do not by themselves prove reversal of disease. To show true reversal, we need biopsy data demonstrating healing of inflammation and regression of scar tissue, also called fibrosis. Early biopsy results are promising, but they are still limited. Larger and longer trials are underway, and their results will be critical in confirming how much tirzepatide can achieve beyond fat reduction.
The promise of tirzepatide is not only in its direct liver effects but also in its ability to change the overall metabolic environment that drives fatty liver disease. NAFLD and NASH are not isolated liver conditions; they are part of a broader metabolic disorder linked with obesity, insulin resistance, and cardiovascular disease. By lowering blood sugar, promoting weight loss, and improving cholesterol and triglycerides, tirzepatide addresses many of the root causes of fatty liver. These whole-body improvements may translate into long-term protection against complications like cirrhosis, liver cancer, heart attack, and stroke. However, proof of these long-term benefits is still pending, and research is ongoing.
It is also important to recognize what tirzepatide cannot yet do. While it is very effective at lowering liver fat and improving liver enzymes, its ability to reverse scarring or fibrosis is not yet clear. Fibrosis is the strongest predictor of future complications, and medications that can reliably reduce fibrosis remain a major unmet need in hepatology. Current evidence suggests that tirzepatide may slow or modestly improve fibrosis in some patients, but we do not yet have enough long-term biopsy data to be certain. For this reason, doctors and researchers are cautious in calling tirzepatide a cure or definitive reversal agent for fatty liver disease. Instead, it should be seen as a promising therapy that can significantly reduce disease activity and risk while we wait for stronger evidence.
Another key point is that tirzepatide is not a standalone solution. Like all treatments for NAFLD and NASH, it works best when combined with healthy lifestyle changes. Sustained weight loss, improved diet quality, regular exercise, better sleep, and reduced alcohol intake remain the foundation of liver care. Tirzepatide can make achieving and maintaining these changes more realistic, but it does not replace them. Doctors will still recommend dietary counseling, physical activity, and regular monitoring of liver health. For patients with advanced disease, tirzepatide should be part of a broader care plan that may include specialist referral and additional testing.
Finally, access and availability remain practical challenges. Tirzepatide is approved for diabetes and obesity, not yet for fatty liver disease specifically. This means many patients with NAFLD or NASH may only gain access if they also meet criteria for obesity or diabetes treatment. Insurance coverage, cost, and health system policies will shape how widely tirzepatide can be used in liver clinics. As more trial results are published, regulatory agencies and guideline committees may expand its use to fatty liver disease, but for now, its role remains partly indirect.
In summary, tirzepatide represents a major step forward in the fight against NAFLD and NASH. It has shown strong evidence for reducing liver fat and improving metabolic health, and early signs suggest it may also help with inflammation and possibly fibrosis. Its full potential is still being studied, but the results so far are very encouraging. The best approach today is to see tirzepatide as part of a comprehensive strategy: one that combines medication with lifestyle changes and ongoing monitoring. For patients and clinicians alike, tirzepatide offers hope for better outcomes, but careful follow-up and continued research will determine exactly how far this hope will go.
Research Citations
Loomba, R., Lawitz, E., Mantry, P. S., Jayakumar, S., Calderon, G., Contreras, A., … Sanyal, A. (2024). Tirzepatide for metabolic dysfunction–associated steatohepatitis with liver fibrosis. The New England Journal of Medicine, 390(24), 2253–2266.
Gastaldelli, A., Cusi, K., Pettiti, G., Hammarstedt, A., An, Z., Liang, Y., … Sattar, N. (2022). Effect of tirzepatide versus insulin degludec on liver fat content, visceral adipose tissue, and abdominal subcutaneous adipose tissue in people with type 2 diabetes (SURPASS-3 MRI). The Lancet Diabetes & Endocrinology, 10(6), 393–406.
Hartman, M. L., Anstee, Q. M., Ratziu, V., & Harrison, S. A. (2025). Consistent improvements in liver histology across tirzepatide dose groups in SYNERGY-NASH. JHEP Reports, 7(10), 100935.
Okuma, H., Tamei, N., & Kato, M. (2025). Effects of tirzepatide on patients with type 2 diabetes and metabolic dysfunction–associated steatotic liver disease: A narrative review of clinical evidence. Primary Care Diabetes, 19, 101547.
Lonardo, A., Mantovani, A., Byrne, C. D., & Targher, G. (2025). Tirzepatide in metabolic dysfunction-associated steatotic liver disease (MASLD): Mechanisms and clinical evidence. Exploration of Digestive Diseases, 5, 1008128.
Targher, G., & Byrne, C. D. (2022). Tirzepatide adds hepatoprotection to its armoury. The Lancet Diabetes & Endocrinology, 10(6), 364–366.
Espinosa, M. A., Shoushtari, A. H., Patel, K., & Younossi, Z. (2024). Tirzepatide and MASLD: Real-world outcomes in a community gastroenterology practice. The American Journal of Gastroenterology, 119(Suppl.), S2120.
Cho, Y., Rhee, E. J., & Park, S.-E. (2024). Hepatobiliary effects and safety of tirzepatide: A systematic review and meta-analysis. Diabetes, Obesity and Metabolism, 26(10), 3337–3351.
Wadden, T. A., Bailey, T. S., Billings, L. K., Capizzi, J., Rubino, D., Schwiers, M., … Garvey, W. T. (2023). Tirzepatide after intensive lifestyle intervention in adults with obesity or overweight. Nature Medicine, 29(9), 2271–2281.
Loomba, R., & SYNERGY-NASH Investigators. (2024). Design and rationale of SYNERGY-NASH: A phase 2 study of tirzepatide for biopsy-confirmed MASH with fibrosis. Alimentary Pharmacology & Therapeutics, 59(10), 1171–1182.
Questions and Answers: Tirzepatide Fatty Liver
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. It improves glycemic control, promotes weight loss, and reduces liver fat by enhancing insulin sensitivity and decreasing lipotoxicity (Heise et al., 2022).
Clinical trials have shown that tirzepatide significantly reduces hepatic fat fraction in patients with type 2 diabetes and obesity, with some studies demonstrating reductions greater than 30% in intrahepatic triglyceride content (Hartman et al., 2022).
Preliminary evidence suggests tirzepatide may improve histologic markers of NASH, such as steatosis and inflammation, although long-term biopsy-confirmed studies are still underway (Newsome et al., 2023).
Tirzepatide may provide greater weight loss and hepatic fat reduction compared to semaglutide due to its dual GIP and GLP-1 receptor activity, although direct head-to-head trials in fatty liver disease populations remain limited (Jastreboff et al., 2022).
Current data show tirzepatide reduces liver fat and inflammation, but evidence on fibrosis improvement is limited and requires further phase 3 trials with histological endpoints (Cusi et al., 2023).
Weight loss is a major driver of tirzepatide’s beneficial effects. By reducing body weight by up to 20%, tirzepatide helps decrease hepatic fat accumulation, improve insulin resistance, and lower systemic inflammation (Jastreboff et al., 2022).
Yes, large-scale trials such as the SURPASS and SURMOUNT programs are evaluating tirzepatide’s effects on metabolic and hepatic outcomes, including dedicated trials for biopsy-confirmed NASH (Eli Lilly, 2023).
Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhea), decreased appetite, and possible gallbladder-related issues. However, most adverse effects are mild to moderate and manageable (Heise et al., 2022).
No, tirzepatide is FDA-approved for type 2 diabetes and under review for obesity management, but it is not yet specifically approved for fatty liver disease (FDA, 2022).
Given its strong effects on weight loss and hepatic fat reduction, tirzepatide holds promise as a future therapy for MASLD/NASH, pending confirmatory evidence from ongoing phase 3 clinical trials (Newsome et al., 2023).

Dr. Melissa VanSickle
Dr. Melissa Vansickle, MD is a family medicine specialist in Onsted, MI and has over 24 years of experience in the medical field. She graduated from University of Michigan Medical School in 1998. She is affiliated with medical facilities Henry Ford Allegiance Health and Promedica Charles And Virginia Hickman Hospital. Her subspecialties include General Family Medicine, Urgent Care, Complementary and Integrative Medicine in Rural Health.
