Table of Contents
1. Introduction to A1C
The A1C test, also known as the HbA1c, glycosylated hemoglobin, or hemoglobin A1C test, is a crucial blood test used to measure the average level of glucose (sugar) attached to hemoglobin in the blood over the past two to three months. This test is a cornerstone in the management of diabetes, providing a long-term overview of an individual’s blood sugar levels, which daily testing cannot offer.
Understanding Hemoglobin and Blood Sugar Levels
Hemoglobin is a protein in red blood cells that carries oxygen throughout the body. In individuals with elevated blood sugar levels, glucose binds to hemoglobin, forming what is known as glycated hemoglobin. The A1C test measures the percentage of hemoglobin that is coated with sugar. The higher the A1C level, the poorer the blood sugar control and the higher the risk of diabetes complications.
A1C: A Key Indicator in Diabetes Management
Diabetes is a chronic condition characterized by high levels of sugar in the blood, primarily due to either the body’s inability to produce insulin (Type 1 diabetes) or resistance to insulin (Type 2 diabetes). Monitoring and managing blood sugar levels are crucial in reducing the risk of diabetes-related complications such as heart disease, kidney failure, and nerve damage. The A1C test serves as a key indicator in this management process, helping both patients and healthcare providers understand how well blood sugar levels are being controlled over time.
Why A1C Matters
The significance of the A1C test cannot be overstated. It provides an aggregate picture of blood sugar control, unlike daily glucose tests, which only provide a snapshot at a single point in time. This comprehensive view is essential for making informed decisions about the management of diabetes, including adjustments in medication, diet, and physical activity. The test is also used for diagnosing prediabetes and diabetes, making it an invaluable tool in early intervention and prevention strategies.
A1C Goals and Diabetes Management
The American Diabetes Association (ADA) recommends an A1C goal of less than 7% for most adults with diabetes, but this target can vary depending on individual circumstances, such as age, comorbidities, and risk of hypoglycemia. Achieving and maintaining the target A1C level is associated with a significant reduction in the risk of diabetes-related complications.
The Evolving Role of A1C Testing
Over the years, the role of A1C testing in diabetes management has evolved. It is now not only a tool for monitoring long-term glycemic control but also a benchmark for adjusting therapeutic strategies. The test’s ability to provide a historical perspective on blood sugar levels makes it indispensable in the ongoing fight against diabetes and its complications.
The A1C test is a vital component in the management and treatment of diabetes. It offers a comprehensive view of an individual’s blood sugar levels over an extended period, aiding in the early diagnosis of diabetes, monitoring ongoing control, and adjusting treatment plans. Understanding A1C levels is crucial for anyone affected by, or at risk of, diabetes, empowering them to take control of their health and reduce the risk of long-term complications.
2. What is A1C and How is it Measured?
The A1C test, a critical tool in the management of diabetes, measures the percentage of glycated hemoglobin (HbA1c) in the blood. Understanding the science behind this test and its measurement process is key to appreciating its role in diabetes care.
The Science of Glycation
Hemoglobin, a protein in red blood cells, carries oxygen from the lungs to the rest of the body. When blood sugar levels are elevated, glucose molecules in the blood bind to hemoglobin in a process called glycation. The resulting compound is known as glycated hemoglobin or HbA1c. The percentage of glycated hemoglobin in the blood correlates with the average blood glucose levels over the previous two to three months, the typical lifespan of a red blood cell.
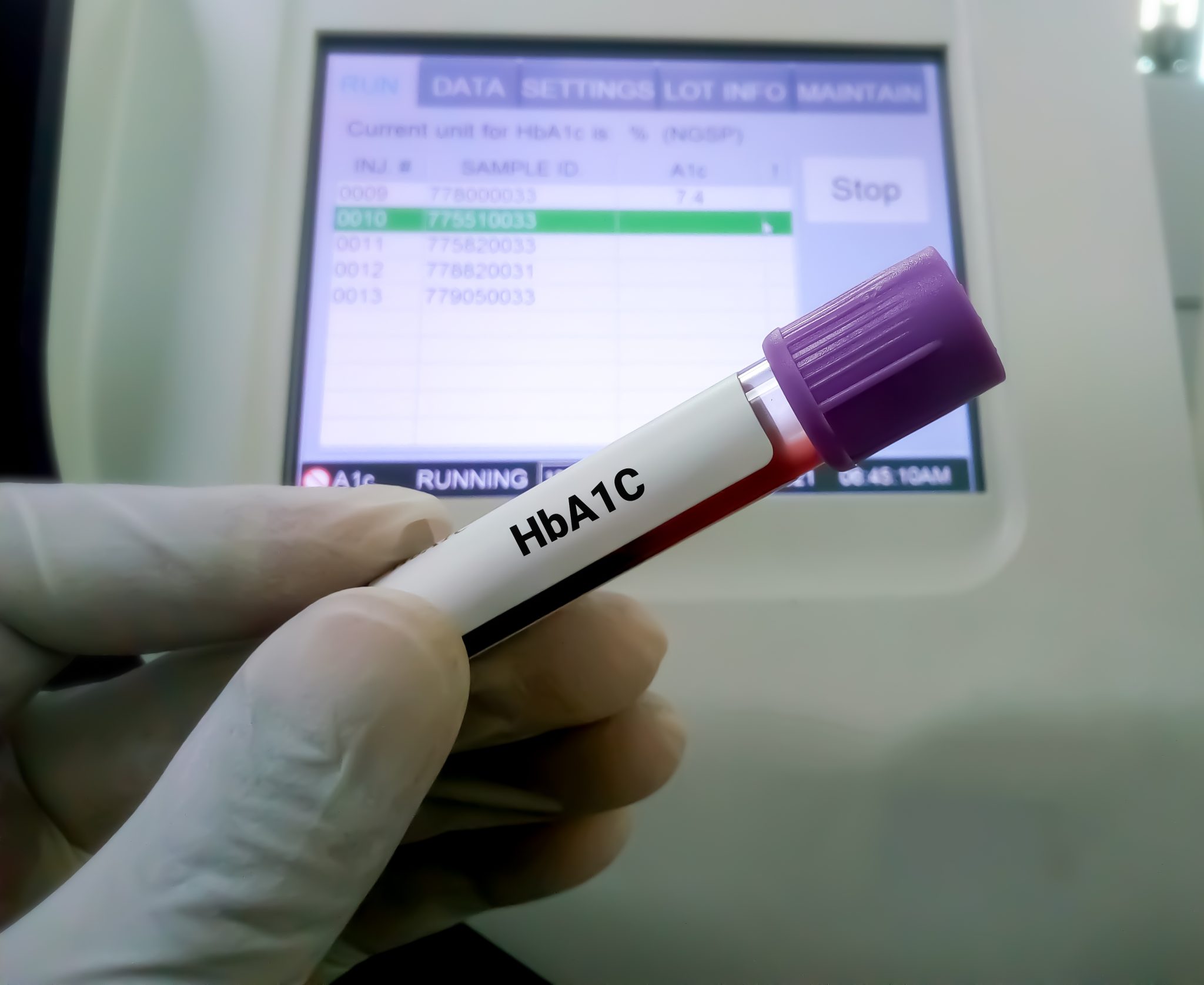
Measuring A1C: The Procedure
The A1C test is a simple blood test that can be performed in a lab or a healthcare provider’s office. Unlike the fasting blood glucose test, the A1C test does not require fasting and can be taken at any time of the day.
During the test, a small sample of blood is drawn from a vein in the arm or, less commonly, from a fingertip prick. The sample is then analyzed to determine the percentage of glycated hemoglobin. This percentage indicates the average blood glucose level over the past few months.
Interpreting the Numbers
The results of the A1C test are expressed as a percentage. For instance, an A1C level of 6% means that 6% of the hemoglobin in your blood is glycated. The American Diabetes Association provides general guidelines for interpreting these percentages:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or higher on two separate tests
It’s important to note that these are general guidelines, and individual targets may vary based on personal health profiles.
Accuracy and Factors Influencing A1C Levels
While the A1C test is a valuable tool, certain factors can influence its accuracy. These include:
- Variations in hemoglobin type, particularly in people of African, Mediterranean, or Southeast Asian descent.
- Conditions affecting red blood cell turnover, such as anemia or hemolysis.
- Certain medications, including those affecting hemoglobin, such as erythropoietin.
It’s essential for healthcare providers to consider these factors when interpreting A1C test results.
The Role of A1C in Diabetes Diagnosis
The A1C test is also used in the diagnosis of diabetes. An A1C level of 6.5% or higher, confirmed by a second test, typically indicates diabetes. This criterion for diagnosis has been widely adopted due to its convenience and the test’s representation of long-term glycemic control.
The A1C test is a cornerstone in the management of diabetes, providing a longer-term view of blood sugar control than daily blood glucose monitoring. Understanding how it is measured and what the results mean is crucial for anyone living with diabetes or at risk of developing it. By regularly monitoring A1C levels, individuals and healthcare providers can better manage diabetes and reduce the risk of complications associated with the disease.
3. Interpreting A1C Test Results
Interpreting A1C test results is fundamental in understanding one’s diabetes management and overall health. The A1C test provides a snapshot of the average blood glucose levels over approximately the last three months, reflecting the long-term effectiveness of diabetes management strategies.
Understanding A1C Levels
A1C levels are reported as a percentage. This percentage correlates directly to the average blood glucose levels over the lifespan of red blood cells (about 120 days). The higher the percentage, the higher the average blood glucose levels have been during this period. The American Diabetes Association (ADA) provides general guidelines for interpreting A1C levels:
- Normal (Non-Diabetic Range): An A1C level below 5.7% is considered within the normal range. This indicates that there is a minimal amount of glucose attached to the hemoglobin in the blood.
- Prediabetes: An A1C level between 5.7% and 6.4% is indicative of prediabetes. This is a warning sign that the blood sugar levels are higher than normal but not high enough to be classified as diabetes.
- Diabetes: An A1C level of 6.5% or higher on two separate tests is diagnostic of diabetes. This shows that blood sugar levels have been consistently elevated.
A1C Goals for Diabetes Management
For people with diabetes, maintaining an A1C level within a target range is crucial. The ADA generally recommends a target A1C level of less than 7% for most adults with diabetes. However, A1C targets should be personalized. Some individuals may have slightly higher or lower targets depending on factors such as age, duration of diabetes, presence of other health conditions, and risk of hypoglycemia.
A1C and Estimated Average Glucose (eAG)
Some laboratories also report an Estimated Average Glucose (eAG) along with the A1C percentage. The eAG translates the A1C percentages into the same units as everyday blood glucose meters (mg/dL or mmol/L). For example, an A1C of 7% corresponds to an eAG of approximately 154 mg/dL (8.6 mmol/L). This conversion helps in correlating the A1C results with daily glucose monitoring values.
Factors Influencing A1C Results
It’s important to understand that certain conditions can affect the accuracy of A1C test results. These include:
- Variations in red blood cell turnover, such as anemia or recent blood loss.
- Hemoglobin variants, more common in certain ethnic groups.
- Kidney or liver disease, which can affect the lifespan of red blood cells.
A1C in Special Populations
The interpretation of A1C results may vary in special populations. For example, pregnant women, people with certain types of anemia, or those with hemoglobinopathies may need a different approach to interpret their A1C levels. A1C test results provide invaluable information for managing diabetes. Understanding what the numbers indicate can empower individuals to take proactive steps in their diabetes care and make informed decisions about lifestyle and treatment options. Regular monitoring and understanding of A1C levels are key to effective diabetes management and reducing the risk of long-term complications.

4. The Role of A1C in Diabetes Management
The role of the A1C test in diabetes management is multifaceted, extending beyond mere monitoring to influencing treatment strategies and assessing the risk of complications. This section delves into the various aspects of how A1C impacts the management of diabetes.
A1C as a Management Tool
A1C serves as a critical tool in managing both Type 1 and Type 2 diabetes. It provides a comprehensive picture of an individual’s blood sugar control over a period of two to three months, offering a more extended view than daily blood glucose testing. This long-term perspective is essential for evaluating the effectiveness of a diabetes management plan, including diet, physical activity, and medications.
Setting Individualized A1C Targets
One of the key aspects of diabetes management is the individualization of A1C targets. The American Diabetes Association recommends a general target of less than 7% for most adults with diabetes. However, this target may be adjusted based on individual factors such as age, duration of diabetes, comorbid conditions, and the risk of hypoglycemia. For instance, a more stringent target (such as less than 6.5%) may be set for younger individuals or those with a shorter duration of diabetes. Conversely, a less stringent target (perhaps 8% or higher) may be more appropriate for older adults, those with significant comorbidities, or those at risk of hypoglycemia.
Monitoring and Adjusting Treatment
Regular A1C testing helps in making informed decisions about treatment adjustments. If A1C levels are higher than the target, it may indicate the need for changes in the treatment regimen, such as adjusting medication dosages, introducing new medications, or intensifying lifestyle interventions. Conversely, if A1C levels are consistently lower than the target, it might prompt a reduction in medication to avoid hypoglycemia.
Predicting Diabetes Complications
High A1C levels over time are associated with an increased risk of diabetes-related complications, such as neuropathy, nephropathy, retinopathy, and cardiovascular diseases. Regular A1C testing allows healthcare providers to assess the risk of these complications and take proactive measures to mitigate them.
A1C in Special Populations
The management of diabetes using A1C levels in special populations, such as pregnant women, children, and the elderly, requires careful consideration. For instance, pregnant women with pre-existing diabetes are often advised to maintain lower A1C levels to reduce the risk of fetal complications.
Education and Patient Involvement
Educating patients about the importance of A1C in managing their diabetes is vital. Understanding A1C levels enables individuals to take an active role in their diabetes care, making lifestyle changes and adhering to treatment plans more effectively.
The A1C test is not just a diagnostic tool; it is integral to the ongoing management of diabetes. By providing a clear picture of long-term blood glucose control, it guides treatment decisions, helps in setting personalized goals, and plays a crucial role in preventing complications. As such, A1C testing is an essential component of comprehensive diabetes care.
5. Frequency of A1C Testing
The frequency of A1C testing is a critical component of diabetes management. It is tailored to individual needs and can vary depending on various factors, including the type of diabetes, the stability of blood glucose levels, and the specific treatment goals for each patient.
General Guidelines for A1C Testing
The American Diabetes Association (ADA) offers general guidelines for the frequency of A1C testing:
- For Non-Diabetic Individuals: A1C testing is not regularly required. It may be performed as part of a health checkup or if there is a suspicion of diabetes.
- For Individuals with Type 2 Diabetes: If blood glucose levels are stable and the diabetes management goals are being met, A1C testing might be recommended twice a year. This frequency ensures that any significant changes in glucose control are detected in a timely manner.
- For Individuals with Type 1 Diabetes or Unstable Type 2 Diabetes: More frequent testing is advised, typically every three months. This frequency is particularly important for those whose treatment has changed or who are not meeting their glycemic goals.
Adjusting Testing Frequency Based on Individual Needs
The testing frequency can be adjusted based on several factors:
- Change in Treatment: If there is a change in the diabetes management plan, such as the introduction of a new medication or insulin therapy, more frequent A1C testing might be needed to assess the effectiveness of the change.
- Pregnancy: Pregnant women with pre-existing diabetes are typically monitored more closely with frequent A1C tests to ensure optimal glycemic control to reduce risks to the fetus and mother.
- Presence of Diabetes Complications: If there are complications related to diabetes, such as kidney disease or cardiovascular issues, more frequent monitoring may be required to manage these conditions effectively.
The Role of Patient-Provider Communication
Effective communication between patients and healthcare providers is crucial in determining the appropriate frequency of A1C testing. Patients should be encouraged to discuss their treatment goals, lifestyle changes, and any concerns they may have regarding their diabetes management.
A1C Testing in Conjunction with Daily Monitoring
While A1C testing provides a long-term view of blood glucose control, it is not a substitute for daily blood glucose monitoring, especially for individuals using insulin or those with type 1 diabetes. Daily monitoring helps in making immediate adjustments to diet, exercise, and medication.
The frequency of A1C testing is an essential aspect of personalized diabetes care. Regular monitoring through A1C tests helps in evaluating the effectiveness of the management plan, making necessary adjustments, and reducing the risk of long-term complications. Patients should work closely with their healthcare providers to determine the optimal testing frequency based on their individual health status and diabetes management goals.
6. Factors Affecting A1C Accuracy
The accuracy of the A1C test, while generally reliable, can be affected by various factors. Understanding these influencing elements is crucial for interpreting A1C results accurately and ensuring effective diabetes management.
1. Hemoglobin Variants
The presence of hemoglobin variants is a significant factor that can impact A1C accuracy. Hemoglobin variants are alterations in the hemoglobin molecule that occur more frequently in certain ethnic populations. For example, individuals of African, Mediterranean, or Southeast Asian descent may have hemoglobin variants that affect the A1C test result, leading to either falsely high or low readings.
2. Red Blood Cell Turnover
Conditions that affect the lifespan of red blood cells can alter A1C levels. For instance:
- Anemia: Certain types of anemia can lead to a quicker turnover of red blood cells, potentially resulting in falsely low A1C levels.
- Hemolysis: Conditions causing increased breakdown of red blood cells can also affect A1C results.
- Recent Blood Transfusions: Blood transfusions can introduce red blood cells with different lifespans, impacting the A1C measurement.
3. Kidney and Liver Diseases
Chronic kidney disease and liver disorders can influence A1C test accuracy. These conditions can affect the production and lifespan of red blood cells, leading to skewed A1C results. Therefore, individuals with these conditions may require alternative methods for monitoring blood glucose levels.
4. Iron-Deficiency Anemia
Iron-deficiency anemia can cause a falsely elevated A1C result. This is because iron deficiency affects hemoglobin synthesis, leading to an increased binding of glucose to the available hemoglobin.
5. Age and Gender
Age and gender can also play a role in A1C levels. Generally, older adults may have slightly higher A1C levels compared to younger individuals. There is also some evidence suggesting that A1C levels might slightly vary between males and females, although the clinical significance of this variation is not fully understood.
6. Pregnancy
Pregnancy can affect A1C levels due to changes in red blood cell turnover and glucose metabolism. Pregnant women, especially those with gestational diabetes or pre-existing diabetes, might require more frequent monitoring with adjusted target A1C levels.
7. Glycation Rate
Individual variations in the rate at which glucose binds to hemoglobin – the glycation rate – can also affect A1C levels. This rate can be influenced by genetic factors and is not directly related to blood glucose levels.
8. Other Health Conditions
Other health conditions, such as hyperglycemia, hypothyroidism, and certain infectious diseases, can influence the accuracy of A1C tests. Given these factors, healthcare providers often consider the entire clinical picture, including A1C results, daily blood glucose monitoring, and the presence of any conditions that might affect A1C accuracy. In some cases, additional tests or alternative methods of monitoring blood glucose levels may be necessary to ensure accurate and effective diabetes management.

7. A1C vs. Daily Blood Glucose Monitoring
Understanding the differences between A1C testing and daily blood glucose monitoring is essential in diabetes management. While both are critical, they serve distinct roles and provide different types of information.
A1C Testing: A Long-term Overview
A1C testing gives a broad overview of glucose control over the past two to three months. It measures the percentage of glycated hemoglobin in the blood, reflecting the average blood glucose levels over the lifespan of red blood cells.
- Pros of A1C Testing:
- Provides a long-term view of blood sugar control.
- Helps predict the risk of diabetes complications.
- Useful in assessing the effectiveness of diabetes management strategies.
- Cons of A1C Testing:
- Does not provide daily fluctuations in blood glucose.
- Can be influenced by factors unrelated to daily glucose levels (such as hemoglobin variants or conditions affecting red blood cell turnover).
Daily Blood Glucose Monitoring: Immediate Insights
Daily blood glucose monitoring involves checking blood sugar levels at various times throughout the day using a glucose meter. It gives immediate insights into how factors like diet, exercise, and medication affect blood sugar levels.
- Pros of Daily Monitoring:
- Offers real-time information about blood glucose levels.
- Helps in making immediate decisions about diet, physical activity, and medication.
- Essential for detecting and preventing hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar).
- Cons of Daily Monitoring:
- Only provides a snapshot of glucose levels at a specific moment.
- Requires frequent, sometimes invasive, testing.
Combining A1C and Daily Monitoring for Comprehensive Management
For comprehensive diabetes management, both A1C and daily glucose monitoring are important. A1C gives a summary of long-term glucose control, while daily testing provides immediate feedback and helps manage day-to-day activities and treatment decisions.
- For Type 1 Diabetes: Individuals with type 1 diabetes typically rely heavily on daily glucose monitoring to manage insulin therapy effectively. A1C testing complements this by providing an overview of how well their regimen is working over time.
- For Type 2 Diabetes: Those with type 2 diabetes may not need to monitor their blood glucose as frequently, especially if not on insulin or if their blood sugar levels are generally stable. However, A1C testing is still crucial for assessing long-term control.
- Adjusting Diabetes Care Plan: Both A1C and daily blood glucose readings can influence adjustments in the diabetes care plan. For instance, an unexplained rise in A1C levels might prompt more intensive daily monitoring to identify and address the causes.
In diabetes management, A1C and daily blood glucose monitoring serve as complementary tools. While A1C provides a long-term overview, daily monitoring offers immediate insights. Together, they enable a comprehensive approach to managing diabetes, helping to balance immediate needs with long-term goals.
8. Managing A1C Levels Through Lifestyle
Managing A1C levels through lifestyle changes is a cornerstone in the treatment of diabetes. Effective lifestyle modifications can significantly impact A1C levels, complementing medication and other medical interventions. This section explores various lifestyle strategies that can help in managing A1C levels.
Dietary Changes
A well-planned diet is crucial in managing blood glucose levels and, consequently, A1C levels. Key dietary strategies include:
- Carbohydrate Management: Understanding and managing carbohydrate intake is essential, as carbohydrates have the most immediate effect on blood glucose levels. This includes not only limiting the amount of carbohydrates but also focusing on the quality, opting for complex carbohydrates with a low glycemic index.
- Portion Control: Eating moderate portions can help regulate blood sugar levels.
- Balanced Meals: Incorporating a balance of carbohydrates, proteins, and fats in each meal can help stabilize blood glucose levels.
- Dietary Fiber: High-fiber foods can slow the absorption of sugar and help improve blood sugar levels.
Physical Activity
Regular physical activity is another key component in managing diabetes and A1C levels. Exercise can increase insulin sensitivity and help muscles use glucose more effectively. Recommendations include:
- Regular Exercise: Aim for at least 150 minutes of moderate aerobic activity per week, such as brisk walking, swimming, or cycling.
- Strength Training: Incorporate strength training exercises at least two days a week.
- Consistency: Regular, daily physical activity is more effective than sporadic high-intensity workouts.
Weight Management
Maintaining a healthy weight is beneficial for controlling A1C levels, especially in Type 2 diabetes. Even a small amount of weight loss can have a significant impact on glucose control.
- Individualized Weight Loss Plans: Tailor weight loss strategies to individual preferences and health conditions.
- Sustainable Practices: Focus on sustainable lifestyle changes rather than quick fixes.
Stress Management
Stress can affect blood glucose levels and diabetes management. Strategies for stress management include:
- Relaxation Techniques: Practices like meditation, deep breathing exercises, and yoga can help reduce stress.
- Regular Exercise: Physical activity is also effective in reducing stress.
- Adequate Sleep: Ensure regular, quality sleep as poor sleep can affect blood glucose control.
Avoiding Tobacco and Limiting Alcohol
Smoking cessation and moderating alcohol intake are important in managing diabetes. Smoking can increase blood sugar levels and lead to insulin resistance, while excessive alcohol can lead to unpredictable changes in blood sugar levels.
Regular Monitoring and Consultation
Regularly monitoring blood glucose levels and consulting with healthcare professionals can help in tailoring these lifestyle changes effectively.
Lifestyle modifications play a crucial role in managing A1C levels and overall diabetes care. Adopting a healthy diet, engaging in regular physical activity, maintaining a healthy weight, managing stress, and avoiding tobacco and excessive alcohol are all strategies that can significantly improve blood glucose control and reduce the risk of diabetes-related complications.
9. A1C in Special Populations
The interpretation and management of A1C levels can vary significantly across different populations. Age, pregnancy, and the presence of certain medical conditions can influence how A1C levels are assessed and managed. This section delves into the nuances of interpreting A1C levels in these special populations.
A1C in Children and Adolescents
Managing diabetes in children and adolescents requires a careful approach, as their bodies are still developing. The American Diabetes Association suggests the following A1C goals for younger people:
- Children (under 6 years old): The goal is less stringent, typically under 8.5%, to minimize hypoglycemia risks while still managing high blood sugar levels.
- Children (6–12 years old): An A1C goal of less than 8% is often recommended, balancing glycemic control and the risk of hypoglycemia.
- Teenagers (13–18 years old): The target is generally under 7.5%, as they can often manage their diabetes more independently.
A1C During Pregnancy
Pregnancy presents unique challenges in diabetes management, with hormonal changes affecting blood glucose levels. Pregnant women with diabetes (Type 1, Type 2, or gestational diabetes) typically aim for lower A1C levels to reduce the risk of complications for the baby and the mother. The target is usually less than 6.5%, but this can vary based on individual health profiles and the risk of hypoglycemia.
Elderly Populations
In older adults, particularly those with significant comorbidities, frailty, or limited life expectancy, A1C goals may be adjusted to be less stringent. The focus is often on quality of life and preventing hypoglycemia, with A1C targets set above the standard 7%. However, individualized care is essential, considering each person’s health status, functional capacity, and risk of hypoglycemia.
Racial and Ethnic Variations
Racial and ethnic differences can influence A1C levels due to variations in red blood cell turnover rates and the prevalence of certain hemoglobin variants. For example, African Americans often have higher A1C levels at a given glucose concentration compared to Caucasians. These differences necessitate a tailored approach to interpreting A1C results.
Individuals with Hemoglobinopathies or Anemia
Conditions such as sickle cell disease or other hemoglobinopathies can affect the accuracy of A1C tests. Similarly, anemia can lead to misleading A1C values. In such cases, alternative methods of assessing blood glucose control may be necessary. A1C management in special populations requires a personalized approach, considering various factors such as age, pregnancy status, comorbidities, and racial or ethnic background. Understanding these nuances is crucial for providing effective diabetes care and ensuring that treatment plans are tailored to meet the unique needs of everyone.
10. Future of A1C Testing
Advancements in medical technology and research are continually shaping the future of A1C testing. These innovations aim to enhance the accuracy, ease, and applicability of A1C tests, making diabetes management more efficient and patient friendly.
1. Non-Invasive Testing Methods
One of the most anticipated advancements in A1C testing is the development of non-invasive methods. Current research is exploring ways to measure A1C levels without the need for blood samples, such as using saliva or tears. These methods would be particularly beneficial for children and individuals who require frequent testing.
2. Personalized Diabetes Management
The future of A1C testing is likely to emphasize personalized medicine. This approach would consider individual variations in hemoglobin glycation rates, genetic factors, and the presence of hemoglobin variants. Tailoring A1C targets based on these personal factors could provide a more accurate assessment of diabetes control for each individual.
3. Improved Hemoglobin Variant Detection
Advancements in detecting and accounting for hemoglobin variants in A1C tests are underway. Improved methodologies would allow for more accurate A1C readings in populations with a high prevalence of hemoglobin variants, such as those of African, Mediterranean, or Southeast Asian descent.
4. Integration with Continuous Glucose Monitoring (CGM)
Systems
The integration of A1C testing with continuous glucose monitoring (CGM) systems represents a significant advancement in diabetes management. CGMs provide real-time data on glucose levels, and combining this information with A1C results could offer a comprehensive overview of an individual’s glucose control.
5. AI and Machine Learning in A1C Interpretation
Artificial intelligence (AI) and machine learning are expected to play a role in interpreting A1C test results. By analyzing large datasets, AI can help identify patterns and predict outcomes more accurately, aiding in personalized treatment plans.
6. Wearable Technology
Wearable technology that can monitor A1C levels continuously is another area of ongoing research. Such devices would allow for constant monitoring of glucose control, potentially alerting individuals to changes in their A1C levels in real-time.
7. Enhanced Patient Education and Engagement
Future developments in A1C testing technology are likely to be accompanied by enhanced patient education tools. Digital platforms and apps could provide patients with more insights into their A1C levels and how lifestyle factors affect their diabetes control.
The future of A1C testing is poised to bring significant improvements in the accuracy, convenience, and personalization of diabetes management. These advancements will not only aid in better glycemic control but also enhance the overall quality of life for individuals living with diabetes. As research and technology continue to evolve, the hope is that managing diabetes will become less burdensome and more precise, leading to improved health outcomes for patients worldwide.
11. Conclusion
The comprehensive exploration of A1C and its critical role in diabetes management underscores its importance as a key indicator for both patients and healthcare professionals. From understanding what A1C is and how it’s measured to recognizing its implications in various populations, the journey through the A1C landscape is intricate and multifaceted.
The Central Role of A1C in Diabetes Care
A1C testing stands as a central pillar in diabetes management. It transcends beyond being a mere diagnostic tool, offering a longitudinal view of an individual’s glucose control. This perspective is invaluable for guiding treatment plans, adjusting medications, and making lifestyle recommendations. It also plays a crucial role in preventing the onset and progression of diabetes-related complications by providing targets for glycemic control.
Personalization and Adaptation in Diabetes Management
One of the critical takeaways from this exploration is the need for personalization in diabetes care. As we have seen, A1C goals and management strategies must be tailored to individual needs, considering factors like age, comorbidities, and specific health conditions. This approach ensures that each person receives the most appropriate and effective care for their unique situation.
The Importance of Patient Involvement and Education
Another important aspect is the role of patient involvement and education. Understanding A1C and its implications empowers patients to take an active role in their health care. This knowledge enables them to make informed decisions about their lifestyle and treatment, fostering a collaborative approach to diabetes management.
The Evolving Landscape of A1C Testing
Looking ahead, the evolving landscape of A1C testing, with advancements in technology and personalized medicine, promises to further refine and enhance diabetes management. Innovations such as non-invasive testing methods, AI integration, and continuous monitoring technologies are set to revolutionize how A1C is used in diabetes care.
A Call to Action for Continuous Learning and Adaptation
The journey through the world of A1C testing is one of continuous learning and adaptation. For healthcare professionals, staying abreast of the latest advancements and research is vital for providing the best care. For patients, engaging actively in their health care journey and staying informed are key to managing their condition effectively. As the field of diabetes care continues to evolve, so too must our approaches to understanding and utilizing A1C as a tool for better health outcomes.
12. References
In compiling this comprehensive guide on A1C and its implications in diabetes management, various reputable sources have been consulted to ensure the accuracy and reliability of the information provided. These sources include medical journals, guidelines from health organizations, and educational materials from diabetes associations. Below is a list of key references that have been instrumental in shaping the content of this guide:
- American Diabetes Association (ADA): The ADA provides extensive resources and guidelines on diabetes management, including recommendations on A1C testing and interpretation. Their publications are crucial for understanding diabetes care and are frequently updated to reflect the latest research and clinical practices.
- ADA Standards of Medical Care in Diabetes
- Centers for Disease Control and Prevention (CDC): The CDC offers valuable information on diabetes, including detailed explanations of A1C and its role in monitoring diabetes. They also provide insights into lifestyle management for diabetes control.
- CDC’s Diabetes Basics
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): NIDDK’s resources are pivotal in understanding the medical and scientific aspects of A1C testing and diabetes management. They offer in-depth research-based information.
- NIDDK’s A1C Test and Diabetes
- Mayo Clinic: Renowned for its medical expertise, Mayo Clinic provides comprehensive information on A1C tests, including how they are conducted, interpreted, and their significance in diabetes care.
- Mayo Clinic’s A1C Test
- Cleveland Clinic: As a leading healthcare provider, Cleveland Clinic offers insights into A1C testing and its role in diabetes management, highlighting practical aspects and patient care considerations.
- Cleveland Clinic on A1C
- Journal Articles and Medical Research: Various peer-reviewed medical journals and research articles have been referenced for the latest studies and findings related to A1C, diabetes management, and emerging technologies in diabetes care. These include publications in journals like ‘Diabetes Care’, ‘The Journal of Clinical Endocrinology & Metabolism’, and others.
- Diabetes Education Materials: Various diabetes associations and organizations provide educational materials that are useful for both patients and healthcare providers. These materials offer practical advice, lifestyle management tips, and patient care strategies.
These references represent a fraction of the vast amount of information available on A1C and diabetes management. They provide a solid foundation for understanding the complexities of diabetes care and the importance of A1C testing in this context. For more detailed information and to stay updated with the latest in diabetes care, consulting these sources regularly is highly recommended.
Questions and Answers: A1C test
A1C, also known as glycated hemoglobin, is a blood test that measures the average amount of glucose attached to hemoglobin over the past 2-3 months. It is crucial for diagnosing prediabetes and diabetes and for monitoring blood sugar control in individuals with diabetes. By reflecting long-term blood sugar levels, A1C helps in assessing the risk of diabetes complications and the effectiveness of management strategies.
The A1C test is typically performed via a blood draw from a vein in the arm. It does not require fasting and can be done at any time of the day. The blood sample is then analyzed in a lab to measure the percentage of glycated hemoglobin.
An A1C level of 6.5% or higher usually indicates diabetes. It signifies that, on average, about 6.5% of your hemoglobin has been glycated due to high blood sugar levels. This level is used as a diagnostic criterion for diabetes.
Yes, very low A1C levels (typically below 4%) might suggest issues such as insufficient glucose in the blood (hypoglycemia) or an underlying health condition. It’s important to discuss such low readings with a healthcare provider to understand the cause and implications.
Typically, individuals with diabetes are advised to get their A1C tested every three months, especially if they are not meeting their glycemic goals or if their treatment plan has changed recently. For those with stable diabetes management, testing might be recommended twice a year.
Yes, conditions like anemia, kidney disease, and certain genetic hemoglobin variants can affect A1C accuracy. These conditions might lead to falsely high or low A1C results, necessitating alternative methods for assessing blood glucose control.
While the A1C test is used similarly for monitoring both Type 1 and Type 2 diabetes, individual target A1C levels might differ based on the treatment plan, risk of hypoglycemia, and other personal health factors.
Absolutely. Healthy lifestyle changes such as diet modification, regular exercise, weight management, and stress reduction can significantly influence blood sugar levels and, consequently, A1C levels.
The A1C test might not be accurate in people with certain conditions like anemia or hemoglobinopathies. Also, it does not provide information on daily fluctuations in blood glucose levels or hypoglycemic episodes.
Emerging developments in A1C testing include non-invasive testing methods, personalized targets based on individual health profiles, and integration with continuous glucose monitoring systems. These advancements aim to make A1C testing more precise and patient friendly.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.