Table of Contents
Introduction
In the vast landscape of pharmacological treatments, the discovery and development of drugs like semaglutide and prednisone represent significant milestones in modern medicine. These medications, though distinct in their chemical nature and therapeutic applications, play pivotal roles in managing a variety of conditions, from chronic diseases like diabetes to acute inflammatory reactions. This article aims to delve into the intricacies of both semaglutide and prednisone, shedding light on their mechanisms, benefits, and the critical considerations necessary for their use.
Semaglutide is a relatively recent addition to the pharmacopeia, primarily used in the treatment of type 2 diabetes. As a GLP-1 receptor agonist, it enhances the secretion of insulin, the hormone responsible for regulating blood glucose levels. Its role, however, extends beyond merely controlling blood sugar; recent studies have shown promising results in weight management and cardiovascular risk reduction among diabetic patients. The significance of semaglutide in today’s treatment regimens reflects a broader shift towards medications that not only treat conditions but also improve overall quality of life and long-term health outcomes.
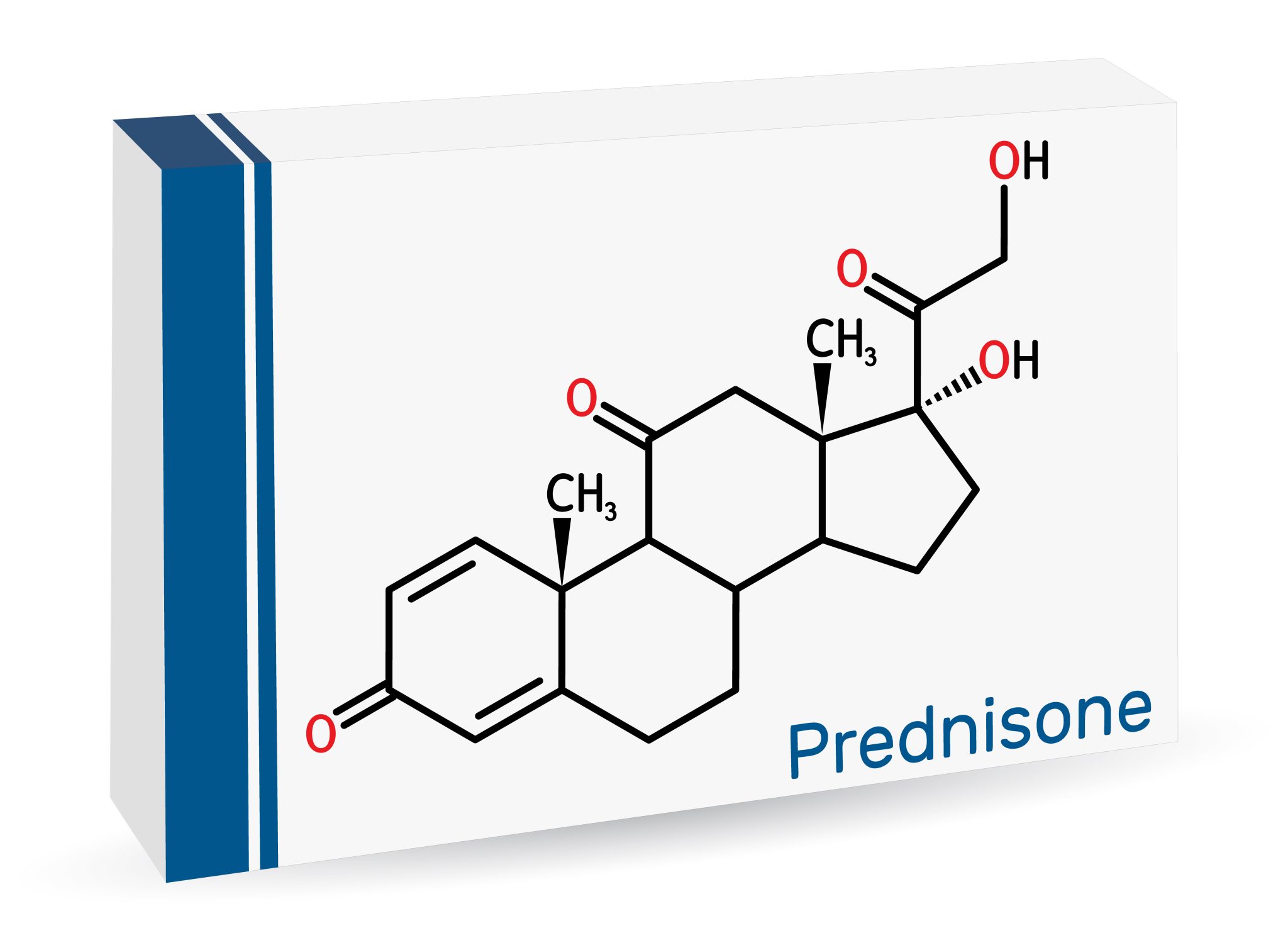
Prednisone, on the other hand, is a well-established corticosteroid used extensively to suppress the immune system and decrease inflammation. Its applications range from treating autoimmune diseases like rheumatoid arthritis and lupus to managing severe allergic reactions and acute flare-ups of chronic conditions such as asthma and COPD. The ability of prednisone to rapidly alleviate symptoms makes it invaluable in acute medical settings, yet its potent effects and the potential for significant side effects necessitate careful management and monitoring.
The mechanisms of action of these drugs, while vastly different, underscore the complexity and precision of current medical therapies. Semaglutide’s mechanism involves mimicking the incretin hormones, which are naturally occurring substances in the body that help to increase insulin secretion in response to meals. This not only helps in regulating blood sugar levels but also slows gastric emptying and reduces appetite, contributing to weight loss in patients.
Prednisone works by mimicking the effects of cortisol, a steroid hormone produced by the adrenal glands, which is vital in managing stress, metabolism, and inflammatory responses. By acting as a synthetic cortisol, prednisone can effectively control inflammation by suppressing the migration of white blood cells to the site of inflammation and the further release of inflammatory substances in the body.
Understanding these mechanisms is critical for healthcare providers as they tailor treatments to individual patient needs, considering factors such as the severity of the condition, the presence of co-morbidities, and the potential for adverse effects. It is equally important for patients, as it impacts their adherence to treatment and their understanding of how these drugs are helping them manage their health conditions.
The evolution of treatment strategies involving semaglutide and prednisone also reflects broader trends in healthcare, particularly the move towards more personalized medicine. With advancements in genetic testing and biomarkers, treatments can often be tailored to enhance efficacy and minimize risks for individual patients. This is especially relevant given the range of potential side effects associated with these drugs, from mild nausea and headaches with semaglutide to more severe implications like osteoporosis and immune suppression with long-term prednisone use.
As we explore these medications further in the following sections, we will discuss their clinical benefits, the therapeutic challenges they pose, and the cutting-edge research that continues to uncover their full potential. This discussion will not only highlight the significant role that semaglutide and prednisone play in modern medical treatments but also their impact on patient care protocols and the ongoing efforts to improve health outcomes while minimizing adverse effects.
Thus, this article will serve as a comprehensive guide to both semaglutide and prednisone, providing insights into their uses, effects, and the critical health considerations necessary for patients and healthcare providers alike. Through a detailed examination of their roles in treatment, potential interactions, and patient management strategies, we aim to equip readers with a thorough understanding of these powerful medications.
What is Semaglutide?
Semaglutide represents a significant advancement in the pharmacological management of type 2 diabetes, offering a novel approach to a disease that affects millions worldwide. This medication is classified as a glucagon-like peptide-1 (GLP-1) receptor agonist, a class of drugs that mimic the action of the naturally occurring hormone GLP-1, which is integral to glucose metabolism.
Origin and Development
Developed through years of research and clinical trials, semaglutide was designed to improve glycemic control in adults with type 2 diabetes by enhancing the body’s own ability to lower blood sugar levels. Unlike traditional insulin therapy, which directly supplements insulin levels, GLP-1 receptor agonists like semaglutide enhance the body’s natural secretion of insulin in response to increased blood glucose levels. This not only helps in reducing the risk of hypoglycemia—a common side effect of diabetes treatments—but also aligns more closely with the body’s own regulatory mechanisms.
Mechanism of Action
The primary mechanism through which semaglutide operates is the stimulation of insulin release from the pancreatic beta cells in the presence of elevated glucose levels. However, its actions extend beyond just enhancing insulin secretion. Semaglutide also suppresses the secretion of glucagon, another hormone produced by the pancreas that typically raises blood glucose levels. By reducing glucagon levels, semaglutide helps lower the amount of glucose released into the bloodstream, particularly from the liver.
Furthermore, semaglutide slows gastric emptying, the process by which food exits the stomach and enters the small intestine. This slowing allows for a more gradual absorption of glucose into the bloodstream, which helps mitigate spikes in blood sugar levels after meals, a common challenge for individuals managing diabetes.
Clinical Benefits
One of the most compelling aspects of semaglutide is its multifaceted benefit profile. Primarily, it improves glycemic control, but it also assists with weight loss. For many patients with type 2 diabetes, weight management is a significant part of disease management. Excess body weight can impair the body’s ability to use insulin effectively, leading to increased insulin resistance. By facilitating weight loss, semaglutide not only helps in controlling blood sugar levels but also addresses one of the underlying risk factors for the progression of diabetes.
In clinical trials, semaglutide has shown to significantly reduce HbA1c levels—a measure of blood sugar management over two to three months. Moreover, studies have demonstrated its effectiveness in reducing the risk of major cardiovascular events, a frequent concern for those with type 2 diabetes, as the condition is often associated with increased cardiovascular risk.
Administration and Dosage
Semaglutide is administered via injection, typically once weekly, which offers convenience compared to medications requiring daily dosing. This mode of administration has been shown to improve patient compliance and satisfaction. The dosage of semaglutide may vary based on individual patient needs, the response to treatment, and the specific goals of therapy. It is crucial that treatment with semaglutide is initiated under the guidance of a healthcare provider who can tailor the dosage to the patient’s specific conditions.
Recent Developments and Future Directions
The therapeutic potential of semaglutide continues to expand as ongoing research explores its benefits beyond diabetes. Recent studies are investigating its use in the treatment of obesity, non-alcoholic steatohepatitis (NASH), and even Alzheimer’s disease, suggesting that the impact of this drug could reach well beyond its current applications.
As we continue to uncover the full spectrum of benefits and applications for semaglutide, it becomes increasingly clear that this medication represents a cornerstone in the evolving landscape of diabetes management. Its development not only highlights the progress in treating chronic conditions like diabetes but also underscores the critical role of innovative pharmacological therapy in improving patient outcomes and quality of life.
What is Prednisone?
Prednisone is a synthetic corticosteroid drug that is commonly prescribed for a wide range of inflammatory and autoimmune conditions. Its extensive use in the medical field is a testament to its effectiveness in managing symptoms associated with severe inflammation and the body’s immune response. Prednisone mimics the effects of hormones that are naturally produced by the adrenal glands and has been a cornerstone in the treatment protocols for various diseases due to its potent anti-inflammatory and immunosuppressive properties.
Historical Context and Development
Developed in the 1950s, prednisone was one of the first corticosteroids to be used extensively in clinical practice. Its introduction marked a significant breakthrough in medical science, offering new treatment options for conditions that were previously challenging to manage, such as rheumatoid arthritis, lupus, and asthma. The development of prednisone was part of a broader search for anti-inflammatory substances that could control the immune system without the severe side effects associated with earlier treatments.
Mechanism of Action
The mechanism by which prednisone works is complex and multifaceted. At its core, prednisone functions by preventing the release of substances in the body that cause inflammation. It does this by entering cells and binding to glucocorticoid receptors, which then migrate to the cell nucleus where they act on the DNA to alter the expression of genes that are involved in the inflammatory process.
This leads to a decrease in the production of inflammatory mediators and an increase in the production of anti-inflammatory proteins. Additionally, prednisone inhibits the function of white blood cells and other components of the immune system, which plays a crucial role in reducing the autoimmune activity that can damage tissues and organs in diseases like lupus and multiple sclerosis.
Clinical Uses
Prednisone is versatile in its clinical applications. It is most commonly prescribed for:
- Autoimmune diseases: Conditions like rheumatoid arthritis, lupus, and inflammatory bowel disease (IBD), where the immune system mistakenly attacks its own tissues.
- Allergic reactions: Severe allergies that require rapid control of symptoms.
- Asthma and COPD: To reduce inflammation in the airways that causes swelling and airway constriction.
- Organ transplantation: To prevent the body’s immune system from rejecting a transplanted organ.
The ability of prednisone to reduce immune activity can be life-saving in situations where inflammation needs to be brought under rapid control. However, the breadth of its use also reflects the need to carefully manage and monitor its administration due to potential side effects.
Dosage and Administration
The dosage of prednisone can vary significantly depending on the medical condition being treated, the severity of the condition, and the individual patient’s response to the medication. It is generally started at a higher dose, which is then tapered down under medical supervision to the lowest possible dose that maintains disease control. This tapering is crucial to reduce the risk of adrenal insufficiency, a condition where the body cannot produce adequate amounts of natural steroids because the adrenal glands have been suppressed by the prednisone.
Challenges and Considerations
Despite its efficacy, the use of prednisone is not without challenges. Long-term use of prednisone can lead to several side effects, including osteoporosis, increased risk of infections, hypertension, diabetes, and cataracts, among others. These potential risks require that the use of prednisone be carefully balanced against the benefits in each case.
Patients on prednisone typically require regular follow-ups and monitoring to manage these risks effectively. Lifestyle adjustments and supplementary treatments may also be necessary to mitigate side effects, such as taking calcium and vitamin D supplements to counteract bone density loss.
Future Directions
As research continues, there is ongoing work to develop new corticosteroids that retain the anti-inflammatory and immunosuppressive effectiveness of prednisone but with fewer side effects. This research is critical, as it aims to enhance the quality of life for patients requiring long-term corticosteroid treatment.
Prednisone remains a vital tool in the treatment of numerous inflammatory and autoimmune conditions. Its ability to quickly and effectively reduce inflammation and modulate the immune system makes it indispensable, despite the challenges associated with its use. As medical science advances, the hope is to improve upon this foundational therapy to maximize benefits and minimize risks for patients around the world.

Comparative Pharmacology of Semaglutide and Prednisone
While semaglutide and prednisone are used in vastly different medical contexts, understanding their pharmacological profiles provides invaluable insights into their roles in modern medicine. Semaglutide, a GLP-1 receptor agonist, and prednisone, a corticosteroid, differ significantly in their chemical structure, mechanism of action, therapeutic uses, and side effects. This comparative analysis explores these differences and similarities, offering a deeper understanding of how these drugs function and are utilized in clinical practice.
Chemical Structure and Classification
Semaglutide is a synthetic analogue of the human glucagon-like peptide-1 (GLP-1), a hormone involved in the regulation of glucose metabolism. It is specifically designed to have a longer half-life than natural GLP-1, allowing for once-weekly dosing. The molecular design of semaglutide includes modifications that protect it from enzymatic degradation by dipeptidyl peptidase-4 (DPP-4) and enhance its binding affinity to the GLP-1 receptor, which is pivotal for its prolonged action.
Prednisone, on the other hand, is a synthetic corticosteroid, mimicking the effects of cortisol, a steroid hormone produced by the adrenal cortex. It is a prodrug that is converted by liver enzymes into prednisolone, the active form. Prednisone’s structure allows it to interact with glucocorticoid receptors, influencing gene expression and thereby modulating inflammation and immune response.
Mechanism of Action
The mechanism of action of semaglutide involves binding to the GLP-1 receptors on pancreatic beta cells, which stimulates insulin release in a glucose-dependent manner. This means that insulin is released only when blood glucose levels are high, thereby reducing the risk of hypoglycemia. Semaglutide also inhibits glucagon secretion and slows gastric emptying, which helps in reducing appetite and promoting weight loss.
Prednisone works by binding to glucocorticoid receptors in cytoplasmic cells, forming a complex that enters the nucleus and acts on DNA to alter the expression of genes involved in inflammatory responses. It suppresses the immune system by reducing the production of inflammatory cytokines and inhibiting the migration of macrophages and leukocytes to areas of inflammation. This broad anti-inflammatory effect is crucial in treating autoimmune and inflammatory conditions.
Pharmacokinetics
Semaglutide exhibits a slow absorption and a long elimination half-life, which supports its once-weekly administration. Its pharmacokinetics are characterized by stable plasma concentrations over time, contributing to its efficacy and patient compliance.
Prednisone has a rapid onset of action, with its effects being felt within hours of administration. It is metabolized in the liver to prednisolone, which is then excreted primarily through the kidneys. The dosing of prednisone can vary widely depending on the severity and type of condition being treated, often requiring adjustments to minimize side effects and achieve optimal therapeutic outcomes.
Therapeutic Uses
The therapeutic uses of semaglutide are primarily focused on type 2 diabetes and, more recently, obesity. It is praised for its ability to control blood sugar levels while promoting weight loss, factors that can significantly impact the management of diabetes and its complications.
Prednisone is utilized in a broad spectrum of conditions that involve inflammation and immune dysregulation, including but not limited to asthma, rheumatoid arthritis, inflammatory bowel disease, and multiple sclerosis. It is often used as a part of induction therapy to quickly suppress immune activity and inflammation.
Side Effects and Safety
While both medications are effective in their respective areas, they come with potential side effects. Semaglutide can cause gastrointestinal issues such as nausea, vomiting, and diarrhea, especially when treatment is initiated. It may also increase the risk of developing pancreatitis.
Prednisone, used in the short term, can lead to increased blood pressure, blood sugar levels, and potential mood swings. Long-term use is associated with more serious effects, including osteoporosis, adrenal suppression, and increased susceptibility to infections.
Understanding the comparative pharmacology of semaglutide and prednisone highlights the complexity of drug effects and interactions in the human body. Each medication, while distinct in application and action, provides essential benefits that improve patient outcomes in the face of challenging medical conditions. As pharmacology continues to evolve, the ongoing study of such drugs will remain crucial for developing safer, more effective therapies tailored to individual patient needs.
Clinical Benefits of Semaglutide
Semaglutide has revolutionized the treatment landscape for type 2 diabetes and obesity, offering substantial benefits that extend beyond basic glycemic control. Its impact on weight management, cardiovascular health, and overall metabolic function has marked it as a significant advancement in diabetes care. This section delves into the clinical benefits of semaglutide, supported by robust research findings and clinical trial data.
Improved Glycemic Control
The primary use of semaglutide is to enhance glycemic control in adults with type 2 diabetes. Semaglutide’s mechanism, which mimics the natural hormone GLP-1, helps regulate insulin secretion in a glucose-dependent manner, thus minimizing the risk of hypoglycemia—a common side effect associated with many diabetes treatments. Clinical studies have consistently shown that semaglutide significantly reduces hemoglobin A1c (HbA1c) levels, a marker of average blood sugar management over two to three months. For many patients, these reductions are profound enough to bring their blood sugar levels within non-diabetic ranges, which is a critical goal in diabetes management.
Weight Loss and Obesity Management
One of the most notable benefits of semaglutide is its effect on body weight. Semaglutide induces weight loss by slowing gastric emptying and reducing appetite, which are mediated through its action on brain centers that control satiety and hunger. Clinical trials, such as the STEP trials, have demonstrated significant weight reduction in patients with obesity, with some losing more than 15% of their initial body weight. This weight loss is particularly beneficial because it directly impacts insulin sensitivity and reduces the burden of other metabolic risk factors associated with obesity, such as hypertension and dyslipidemia.
Cardiovascular Benefits
Type 2 diabetes is often associated with an increased risk of cardiovascular diseases, including heart attack, stroke, and heart failure. Semaglutide has shown promise in not only managing diabetes but also in reducing cardiovascular risk. The landmark cardiovascular outcome trial, SUSTAIN-6, reported that semaglutide led to a marked reduction in major adverse cardiovascular events, such as non-fatal stroke and non-fatal myocardial infarction, among individuals with type 2 diabetes at high cardiovascular risk. This benefit is particularly important as cardiovascular disease remains the leading cause of death in diabetes patients, and improving cardiovascular outcomes is a pivotal aspect of diabetes treatment.
Reduction in Renal Complications
Diabetes can lead to various renal complications, including nephropathy, which can progress to kidney failure if not adequately managed. Semaglutide’s ability to improve glycemic control and blood pressure indirectly benefits renal function. Additionally, emerging evidence suggests that GLP-1 receptor agonists like semaglutide may offer direct renal protection by reducing albuminuria and stabilizing kidney function, although more research is needed to fully understand these effects.
Broadening Therapeutic Applications
The benefits of semaglutide are expanding into areas beyond diabetes and obesity. Recent studies are exploring its potential in treating neurodegenerative diseases, such as Alzheimer’s disease, given its effects on brain function and protection. Additionally, semaglutide is being investigated for its use in non-alcoholic steatohepatitis (NASH), a liver condition that shares many metabolic pathways with type 2 diabetes.
Safety and Tolerability
Semaglutide is generally well-tolerated, with the most common side effects being gastrointestinal in nature, such as nausea, vomiting, and diarrhea. These effects are usually transient and manageable, often decreasing in severity as treatment continues. Importantly, the risk of hypoglycemia with semaglutide is low, particularly when used without concomitant sulfonylurea drugs or insulin.
The clinical benefits of semaglutide extend well beyond its primary use in diabetes management, touching upon significant areas such as weight management, cardiovascular health, and potentially broader therapeutic applications. Its role in improving long-term health outcomes makes semaglutide a valuable component of modern therapeutic strategies for managing complex metabolic diseases. The ongoing research and development into new uses of semaglutide continue to highlight its potential as a transformative medical treatment, making it a cornerstone of innovative pharmacological advancements.
Clinical Benefits of Prednisone
Prednisone, a well-established corticosteroid, plays a pivotal role in the treatment of numerous autoimmune and inflammatory conditions. Its ability to modulate the immune response and reduce inflammation has made it an indispensable tool in modern medicine. This section explores the diverse clinical benefits of prednisone, underscoring its importance in both acute and chronic disease management.
Managing Autoimmune Diseases
Autoimmune diseases, such as rheumatoid arthritis, lupus, and inflammatory bowel disease, involve the immune system mistakenly attacking the body’s own tissues. Prednisone is particularly effective in these conditions because of its potent immunosuppressive properties. By inhibiting the immune response, prednisone can decrease the severity of symptoms and potentially halt disease progression. For instance, in rheumatoid arthritis, prednisone can reduce joint inflammation and pain, improve joint function, and slow damage to bones and joints, thereby enhancing the quality of life for patients.
Treatment of Allergic Reactions
Prednisone is also crucial in the management of severe allergic reactions, including anaphylaxis and angioedema, where rapid immune suppression is necessary. Allergies occur when the body’s immune system reacts to a normally harmless substance. Prednisone can prevent or mitigate these reactions by reducing the immune system’s response to the allergen, thus providing quick relief from symptoms such as swelling, redness, and severe itching.
Controlling Asthma and COPD
Chronic respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD) benefit significantly from prednisone’s anti-inflammatory effects. In these diseases, inflammation leads to narrowed airways and difficulty breathing. Prednisone can be used during exacerbations of asthma or COPD to quickly reduce airway inflammation, improve airflow, and relieve symptoms such as wheezing and shortness of breath. This makes it an essential component of emergency asthma and COPD care, although its use in long-term management is usually limited due to potential side effects.
Role in Organ Transplantation
In the context of organ transplantation, prednisone is used to prevent the body’s immune system from rejecting the transplanted organ. It is part of the standard immunosuppressive regimen used to maintain the viability of transplanted organs such as the kidney, liver, and heart. Prednisone helps reduce the immune system’s ability to recognize and attack the foreign tissue, thereby increasing the success rate of organ transplants and prolonging the life of the transplant.
Treatment of Severe Infections and Other Conditions
Prednisone is sometimes employed in the treatment of severe and life-threatening infections that cause inflammation, such as severe tuberculosis. It is used to control the inflammatory response that can cause tissue damage and complicate recovery. Additionally, prednisone is used in the treatment of certain types of blood disorders, such as leukemia and lymphoma, where it helps kill certain types of cancer cells or reduces the immune system’s attack on the blood cells.
Benefits in Dermatology
In dermatology, prednisone is used to treat severe skin conditions like psoriasis and eczema. These conditions, which cause severe itching, redness, and discomfort, can often be effectively managed with prednisone, reducing symptoms and improving skin appearance. However, due to the risk of side effects, its use is typically reserved for severe cases or as a short-term solution while other treatments are being explored.
Considerations and Cautions
While the benefits of prednisone are vast, its use must be carefully managed to balance effectiveness with the potential for side effects. Long-term use of prednisone can lead to complications such as osteoporosis, increased risk of infections, hypertension, diabetes, and adrenal insufficiency. Therefore, it is typically prescribed at the lowest effective dose for the shortest duration necessary to achieve the desired therapeutic outcome.
The clinical utility of prednisone across a spectrum of diseases underscores its importance in medicine. From autoimmune diseases and severe allergies to asthma management and organ transplantation, prednisone continues to be a cornerstone of therapy in many medical specialties. Its powerful anti-inflammatory and immunosuppressive properties make it essential, but they also necessitate judicious use to minimize potential side effects, underscoring the need for careful patient management and monitoring.

Potential Risks and Side Effects of Semaglutide and Prednisone
While both semaglutide and prednisone offer substantial clinical benefits in their respective fields, their potent effects also come with potential risks and side effects. Understanding these is crucial for healthcare providers and patients to manage and mitigate these risks effectively. This section explores the side effects associated with semaglutide and prednisone, highlighting the importance of monitoring and managing these effects in clinical practice.
Side Effects of Semaglutide
Semaglutide, primarily used for the treatment of type 2 diabetes and obesity, is generally well-tolerated, but it can cause several side effects, particularly gastrointestinal symptoms. The most common include:
- Nausea and Vomiting: These are the most frequently reported side effects, particularly when beginning treatment. These symptoms are generally transient and tend to decrease over time as the body adapts to the medication.
- Diarrhea and Constipation: Changes in bowel habits are common, potentially impacting a patient’s quality of life if persistent.
- Appetite Suppression: While beneficial for weight loss, excessive appetite suppression can lead to inadequate nutrient intake if not carefully managed.
- Risk of Pancreatitis: There is a noted, albeit low, risk of developing pancreatitis, which is a serious condition that requires immediate medical attention. Patients are advised to report any severe abdominal pain promptly.
- Thyroid Tumors: In animal studies, semaglutide has been associated with thyroid C-cell tumors. Although it is not confirmed in humans, it’s recommended to avoid in patients with a personal or family history of medullary thyroid carcinoma or those who have Multiple Endocrine Neoplasia syndrome type 2.
Side Effects of Prednisone
Prednisone, widely used for its anti-inflammatory and immunosuppressive properties, can cause a range of side effects that vary in severity depending on the duration of use, the dose, and individual patient factors. Some of the more common and significant side effects include:
- Increased Susceptibility to Infections: By suppressing the immune system, prednisone increases the risk of bacterial, viral, and fungal infections. Patients on prednisone should be monitored closely for signs of infection.
- Osteoporosis and Bone Loss: Long-term use of prednisone can lead to bone thinning or osteoporosis, significantly increasing the risk of fractures. Calcium and vitamin D supplementation, along with other medications, may be recommended to mitigate this risk.
- Weight Gain and Fluid Retention: Prednisone can cause an increase in appetite, leading to weight gain, and may also cause the body to retain more fluid, leading to swelling.
- Mood Swings and Psychological Effects: Patients may experience mood swings, anxiety, and other psychological effects. In some cases, serious mental health issues like depression or mania can occur.
- Hyperglycemia and Diabetes: Prednisone can increase blood sugar levels, which may necessitate adjustments in the management of diabetes or sometimes lead to the onset of steroid-induced diabetes.
- Hypertension: An increase in blood pressure is a common side effect and must be monitored and managed during treatment with prednisone.
Managing Side Effects
The management of side effects for both medications involves a combination of patient education, monitoring, and sometimes medication adjustment. For semaglutide, starting with a lower dose and gradually increasing may help mitigate gastrointestinal symptoms. Patients should also be educated on the signs of pancreatitis and encouraged to report symptoms early.
For prednisone, regular monitoring of bone density, blood pressure, blood sugar levels, and eye health is crucial, especially in long-term use. Lifestyle modifications, including a balanced diet, regular exercise, and smoking cessation, are also recommended to minimize the risk of adverse effects.
While the side effects of semaglutide and prednisone can be challenging, with careful management, they can often be mitigated, allowing patients to benefit from the significant clinical advantages these medications offer. Ongoing communication between the patient and healthcare provider is essential to adjust treatment plans as needed and to ensure that the benefits of therapy outweigh the risks.
Interactions and Contraindications of Semaglutide and Prednisone
Understanding the interactions and contraindications of medications like semaglutide and prednisone is crucial for ensuring patient safety and the effectiveness of treatments. Both drugs, widely used in clinical practice, have specific considerations that healthcare providers must be aware of to prevent adverse effects and optimize therapeutic outcomes. This section explores the potential drug interactions and contraindications associated with semaglutide and prednisone, highlighting the necessary precautions and considerations.
Semaglutide Interactions and Contraindications
Interactions:
- Antidiabetic Medications: Semaglutide can potentiate the hypoglycemic effects of insulin and sulfonylureas. This requires careful monitoring of blood glucose levels and potential adjustments in dosing to avoid hypoglycemia.
- Oral Medications: Due to its action on gastric emptying, semaglutide can affect the absorption rate of oral medications. This is particularly important for medications where timing and plasma concentration are critical, such as oral contraceptives or antibiotics. It is advised that patients take oral medications at least an hour before or after semaglutide administration.
- Warfarin: There have been reports of changes in INR (international normalized ratio) levels in patients taking warfarin concomitantly with semaglutide, suggesting that more frequent monitoring may be necessary.
Contraindications:
- Personal or Family History of Medullary Thyroid Carcinoma: Due to findings in rodent studies indicating a potential risk of thyroid C-cell tumors, semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma.
- Multiple Endocrine Neoplasia Syndrome Type 2 (MEN 2): This is a genetic condition that can increase the risk of thyroid cancer, and patients with MEN 2 should not use semaglutide.
- Gastroparesis: Because semaglutide slows gastric emptying, it is not recommended for use in patients with gastroparesis as it could worsen their condition.
Prednisone Interactions and Contraindications
Interactions:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): The concurrent use of NSAIDs and prednisone increases the risk of gastrointestinal ulcers and bleeding. Patients using both should be closely monitored for signs of gastrointestinal distress.
- Diuretics: Prednisone can cause potassium loss, and this effect can be compounded when taken with certain diuretics, increasing the risk of hypokalemia (low potassium levels).
- Vaccines: Live vaccines should generally not be given to individuals taking prednisone at immunosuppressive doses due to the risk of activating the vaccine virus, which can lead to severe infections.
- CYP3A4 Inducers and Inhibitors: Drugs that affect the CYP3A4 enzyme can alter prednisone metabolism. For example, CYP3A4 inducers (like some anticonvulsants and antibiotics) can decrease prednisone levels, potentially reducing its efficacy, while inhibitors can increase prednisone levels, leading to toxicity.
Contraindications:
- Systemic Fungal Infections: Prednisone can exacerbate existing fungal infections by suppressing the immune system, so it is contraindicated in patients with systemic fungal infections.
- Hypersensitivity: Any patient with a known hypersensitivity to prednisone or any of its components should not use the medication.
- Administration of Live Vaccines: Due to immunosuppression, patients taking prednisone should not receive live vaccines.
Managing Drug Interactions and Contraindications
The management of potential interactions and contraindications involves a thorough patient history and ongoing monitoring. Healthcare providers should:
- Review all medications a patient is taking before prescribing semaglutide or prednisone.
- Monitor for symptoms of adverse effects or changes in disease symptoms that might suggest an interaction.
- Adjust dosages as necessary and provide guidelines for patients on timing the administration of their medications.
Both semaglutide and prednisone require careful consideration of their interactions and contraindications to safely integrate them into a patient’s treatment plan. Awareness and management of these factors are essential to maximize therapeutic benefits while minimizing risks, ensuring patient safety, and enhancing overall treatment efficacy. Through diligent patient education and monitoring, healthcare providers can navigate the complexities of these interactions and contraindications effectively.
Patient Management Strategies for Semaglutide and Prednisone
Effectively managing patients who are prescribed semaglutide and prednisone involves more than just administering the medication. It requires a comprehensive approach that includes patient education, monitoring for side effects, and adjusting treatment as necessary to maximize benefits and minimize risks. This section outlines strategies for managing patients on these medications, ensuring that their treatment is as safe and effective as possible.
Managing Patients on Semaglutide
Initial Consultation and Education:
- Understanding the Medication: Patients starting semaglutide should be thoroughly educated about its benefits, potential side effects, and its role in their overall treatment plan, especially regarding its effects on blood sugar levels and weight.
- Injection Training: Since semaglutide is administered via injection, proper technique is crucial. Patients should be trained on how to administer the injection themselves, including site rotation and hygiene practices to prevent infection.
Monitoring and Adjustment:
- Regular Follow-Ups: Regular appointments should be scheduled to monitor the patient’s response to semaglutide, particularly during the initial months of treatment. This allows for adjustments in dosage and addresses any side effects or concerns the patient may have.
- Blood Glucose Monitoring: Patients should be instructed on how to monitor their blood glucose levels at home, especially if they are at risk of hypoglycemia. This is crucial for patients who are also taking insulin or sulfonylureas.
Lifestyle Integration:
- Diet and Exercise: Patients should be encouraged to maintain a healthy diet and regular exercise routine, which synergizes with semaglutide’s weight management benefits. A dietitian consultation may be beneficial.
- Weight Monitoring: Regular monitoring of weight is important to assess the effectiveness of the treatment and to motivate patients by showing tangible results.
Managing Patients on Prednisone
Initial Consultation and Education:
- Understanding Prednisone: It’s important that patients understand why prednisone has been prescribed, its significant potential side effects, and the importance of adherence to the prescribed dose and duration.
- Duration and Dosage: Patients should be made aware that the dosage of prednisone may be changed based on their response to the medication and that long-term use can lead to additional health risks.
Monitoring and Management of Side Effects:
- Routine Tests: Regular monitoring through blood tests, bone density scans, and eye exams should be scheduled if the patient is on long-term prednisone to detect early signs of complications like osteoporosis, high blood sugar, or increased eye pressure.
- Infection Watch: Patients should be informed about the increased risk of infection and advised on how to recognize signs of infection and when to seek medical help.
Adjusting Treatment as Needed:
- Tapering the Dose: Unlike many medications, prednisone must often be tapered down rather than stopped abruptly to avoid adrenal insufficiency. The tapering schedule should be clearly communicated to the patient.
- Managing Chronic Use: If a patient is on prednisone long-term, strategies to minimize side effects should be implemented, which may include supplemental therapies such as calcium and vitamin D for bone protection or insulin sensitizers if diabetes develops.
Lifestyle Adjustments:
- Dietary Changes: Patients should be advised on dietary changes to counteract side effects such as hypertension and weight gain. Limiting sodium intake and avoiding excessive calories can be particularly important.
- Physical Activity: Encouraging regular, weight-bearing exercises can help mitigate bone density loss due to long-term prednisone use.
- Managing patients on semaglutide and prednisone requires a proactive, informed approach that considers both the pharmacological effects of the medications and the lifestyle of the patient. Regular monitoring, patient education, and an openness to adjusting treatment plans as necessary are crucial components of effective patient management. By understanding the specific needs and potential risks associated with each medication, healthcare providers can optimize treatment outcomes and enhance patient safety and satisfaction. This integrated approach ensures that the therapeutic benefits of semaglutide and prednisone are fully realized while minimizing their potential adverse effects.

Emerging Research and Future Directions for Semaglutide and Prednisone
As the medical community continues to explore and understand the complexities of diseases and their treatments, both semaglutide and prednisone stand at the forefront of significant emerging research. These drugs, pivotal in treating chronic and acute conditions, are also the focus of studies aiming to expand their therapeutic applications and improve their efficacy and safety profiles. This section discusses the ongoing research and potential future directions in the utilization of semaglutide and prednisone.
Emerging Research on Semaglutide
Broader Applications in Metabolic Diseases:
- Non-Alcoholic Steatohepatitis (NASH): Recent studies are investigating the effectiveness of semaglutide in treating NASH, a liver disease often associated with obesity and type 2 diabetes. Preliminary results suggest that semaglutide can significantly reduce liver fat and inflammation, which are key factors in the progression of NASH.
- Cardiovascular Disease Prevention: Beyond its role in glycemic control and weight loss, semaglutide is being studied for its potential to reduce major adverse cardiovascular events. Ongoing trials aim to understand the full extent of its cardiovascular benefits in populations at high risk of heart disease.
Innovative Delivery Systems:
- Oral Formulations: Although currently administered via injection, research into oral formulations of semaglutide is advancing. An oral version could dramatically improve patient adherence and widen its use, making it a more convenient option for diabetes management.
- Longer-Acting Formulations: Efforts to develop even longer-acting versions of semaglutide that could be administered less frequently than once weekly are underway, which could further improve patient compliance and quality of life.
Future Directions for Prednisone
Reducing Side Effects:
- Selective Glucocorticoid Receptor Agonists (SEGRAs): Researchers are developing newer types of glucocorticoids that aim to retain the anti-inflammatory benefits of prednisone while minimizing its side effects. These drugs, known as SEGRAs or ‘dissociated glucocorticoids,’ are designed to elicit fewer metabolic effects, such as weight gain and bone loss.
- Targeted Delivery Systems: Another area of development is the creation of formulations that can target inflamed tissues directly, potentially reducing the systemic exposure to prednisone and thereby its broad immunosuppressive and metabolic effects.
Enhanced Treatment Protocols:
- Combination Therapies: Ongoing research focuses on the effectiveness of combining prednisone with other medications to enhance its benefits or diminish its side effects. For instance, combining prednisone with drugs that protect against bone density loss could mitigate one of its most significant long-term risks.
- Precision Medicine Approaches: As the field of genetic medicine evolves, there is potential for more personalized approaches in prescribing prednisone. Understanding individual genetic predispositions to side effects could allow clinicians to tailor treatment plans more effectively.
Integrating Technology and Treatment
Digital Health Tools:
- Patient Monitoring: Both drugs could benefit from the integration of digital health tools, such as apps that track symptoms, medication adherence, and side effects. For semaglutide, this could help patients manage their weight loss and diabetes symptoms more effectively. For prednisone, it could monitor signs of complication that require immediate medical attention.
- Telemedicine: Ongoing management for patients on these medications might also evolve through the use of telemedicine, which can provide continuous support and guidance, particularly for patients in remote areas or those who have difficulties with frequent healthcare visits.
- The future of semaglutide and prednisone looks promising with the potential for expanded uses, improved formulations, and integration with technology that could transform patient outcomes. Continued research and innovation are likely to not only extend the benefits of these medications to a broader population but also enhance their safety and effectiveness. As new findings emerge, they will guide adjustments in clinical practices, potentially setting new standards in the treatment of complex diseases such as diabetes, autoimmune disorders, and beyond. By staying at the cutting edge of these developments, the medical community can better serve patients and lead the way in chronic and acute disease management.
Conclusion
The exploration of semaglutide and prednisone throughout this article reveals the intricate balance of benefits and challenges that these medications present in the field of medicine. Both drugs play crucial roles in managing complex diseases—semaglutide in the treatment of type 2 diabetes and obesity, and prednisone in the management of inflammatory and autoimmune conditions. As we conclude, let us summarize the key points discussed and reflect on the future implications of these therapeutic agents.
Summary of Key Points
Semaglutide has demonstrated significant efficacy in improving glycemic control and promoting weight loss in individuals with type 2 diabetes. Its benefits extend beyond diabetes management, showing promise in cardiovascular health and potentially in the treatment of non-alcoholic steatohepatitis (NASH) and other metabolic disorders. The drug’s ability to mimic natural hormonal interactions in the body allows for a physiological approach to diabetes management that aligns with the body’s natural systems, thereby minimizing risks such as hypoglycemia and promoting overall health improvements.
Prednisone, a potent corticosteroid, is indispensable in acute and chronic management of autoimmune and inflammatory conditions. Its rapid action in suppressing inflammation and modulating the immune response makes it a cornerstone in the treatment of conditions like asthma, rheumatoid arthritis, and lupus. However, the broad and potent effects of prednisone come with a significant burden of side effects, particularly with long-term use, which necessitates careful management and monitoring to balance efficacy with safety.
Future Implications
The ongoing developments in the pharmacology of semaglutide and the therapeutic management with prednisone highlight the dynamic nature of medical treatment and the continuous improvement in patient care protocols. As research progresses, we anticipate further refinements in how these drugs are used, including:
- Improved formulations that could potentially offer better control, greater efficacy, and fewer side effects.
- New therapeutic indications as ongoing clinical trials explore broader applications for these drugs.
- Enhanced patient management strategies that incorporate digital tools for monitoring and real-time data analysis to better tailor treatments to individual patient needs.
The incorporation of semaglutide and prednisone into patient care also underscores the importance of a holistic approach to treatment—one that considers not only the pharmacological actions of the drugs but also the lifestyle, dietary, and psychosocial aspects of the patient’s health. Educating patients about their conditions and treatments, encouraging adherence to therapy, and regularly monitoring for adverse effects are all critical components that healthcare providers must consider to ensure optimal treatment outcomes.
Patient Education and Advocacy
Educating patients about the effects, potential side effects, and management strategies related to semaglutide and prednisone is essential. Patients should be encouraged to maintain an open line of communication with their healthcare providers, reporting any side effects or concerns that arise during their treatment. Patient advocacy groups and resources can also play a supportive role, providing additional information and community support for individuals navigating these treatments.
Encouraging Ongoing Research and Development
Finally, the medical community must continue to support research and development in the field of pharmacotherapy. Ongoing studies and clinical trials are crucial for uncovering new applications for these drugs, improving formulations, and ultimately enhancing patient care. As we learn more about the molecular and cellular pathways affected by semaglutide and prednisone, new opportunities for targeted therapies and personalized medicine will emerge, potentially revolutionizing the way we manage chronic diseases.
In conclusion, semaglutide and prednisone represent significant achievements in medical science, each playing a unique role in enhancing the quality of life for patients with chronic conditions. By continuing to explore and understand these medications, the medical community can better serve the diverse needs of patients, ensuring that the therapies not only manage the diseases but also contribute positively to comprehensive health outcomes. Click to learn more about the price of semaglutide with BMI Doctors.
References
Semaglutide:
Aroda, V. R., Ahmann, A., Cariou, B., Chow, F., Davies, M. J., Jódar, E., … & Lingvay, I. (2017). Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. The Lancet Diabetes & Endocrinology, 5(6), 355-366.
Pratley, R., Aroda, V., Lingvay, I., Lüdemann, J., Andreassen, C., Navarria, A., … & Garber, A. (2018). Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. New England Journal of Medicine, 379, 1837-1847.
Prednisone:
Hoes, J. N., Jacobs, J. W., Boers, M., Boumpas, D., Buttgereit, F., Caeyers, N., … & Kirwan, J. R. (2007). EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases. Annals of the Rheumatic Diseases, 66(12), 1560-1567. DOI:
Strehl, C., Bijlsma, J. W., de Wit, M., Boers, M., Caeyers, N., Cutolo, M., … & Buttgereit, F. (2016). Defining conditions where long-term glucocorticoid treatment has an acceptably low level of harm to facilitate implementation of existing recommendations: viewpoints from an EULAR task force. Annals of the Rheumatic Diseases, 75(6), 952-957.
General Pharmacology and Clinical Practices:
Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition. Editors: Brunton, L., Hilal-Dandan, R., & Knollmann, B. C. (2018). McGraw-Hill Education.
Koda-Kimble and Young’s Applied Therapeutics: The Clinical Use of Drugs. 11th Edition. Editors: Alldredge, B. K., Corelli, R. L., Ernst, M. E., Guglielmo, B. J., Jacobson, P. A., Kradjan, W. A., & Williams, B. R. (2018). Wolters Kluwer Health.
Questions and Answers: Semaglutide and Prednisone
Semaglutide is primarily prescribed for the treatment of type 2 diabetes. It is used to improve blood sugar control and is also beneficial for weight loss, which can be a significant adjunct benefit for many diabetic patients. Additionally, its cardiovascular benefits make it a preferred choice for diabetic patients at risk of heart disease. Prednisone is frequently prescribed for its powerful anti-inflammatory and immunosuppressive properties. It is used to treat a wide array of conditions, including autoimmune diseases like rheumatoid arthritis and lupus, severe allergic reactions, asthma, and other respiratory disorders. It is also used in the management of acute flare-ups of chronic conditions and to prevent organ rejection in transplant patients.
Patients often respond positively to semaglutide with improved glycemic control and weight reduction. The drug’s effects on blood sugar levels are usually apparent within a few weeks of treatment initiation. Weight loss may continue progressively over several months. Prednisone responses can vary depending on the condition being treated but typically, patients experience rapid relief from inflammation and a decrease in symptoms associated with their condition. However, the response to prednisone can also come with a variety of side effects, which must be managed carefully.
Taking semaglutide and prednisone together does not typically present a direct risk of drug interaction since their mechanisms of action and treated conditions are quite different. However, patients taking both may need to be monitored for overall effects such as changes in blood sugar levels, as prednisone can increase blood glucose levels, potentially counteracting the glucose-lowering effect of semaglutide.
Semaglutide is generally not recommended during pregnancy as there is limited data on its safety in pregnant women. It should be used only if the potential benefit justifies the potential risk to the fetus. Prednisone may be used during pregnancy when necessary, as the benefits might outweigh the risks, especially in severe autoimmune diseases. However, it should be used under strict medical supervision.
Patients experiencing severe side effects from either semaglutide or prednisone should contact their healthcare provider immediately. It’s crucial not to discontinue prednisone abruptly due to the risk of adrenal insufficiency. Any adjustments to dosage should be done under medical guidance.
Lifestyle choices can significantly impact the effectiveness of both medications. For semaglutide, a healthy diet and regular exercise enhance its blood sugar-lowering and weight management benefits. For prednisone, maintaining a balanced diet with limited salt intake and healthy weight can help mitigate side effects such as bone loss, high blood pressure, and weight gain.
For semaglutide, patients are generally advised to follow a diet low in calories and carbohydrates to enhance the drug’s effects on weight and glycemic control. For prednisone, a low-salt, high-potassium diet is often recommended to manage fluid retention and prevent hypokalemia. Calcium and vitamin D supplementation might also be recommended to protect against bone loss.
There are several alternatives to semaglutide for diabetes management, including other GLP-1 receptor agonists, insulin therapies, and oral antidiabetic drugs. For prednisone, alternative treatments may include other corticosteroids with potentially fewer side effects or different immunosuppressive agents, depending on the specific condition being treated.
Semaglutide is often used long-term for chronic management of diabetes. The duration depends on the patient’s response and the progression of their condition. Prednisone is ideally used for the shortest duration possible to minimize side effects, although some conditions may require long-term use under close medical supervision.
Advancements in treatments involving semaglutide include ongoing research into its use in non-diabetic obesity, NASH, and cardiovascular diseases. For prednisone, newer, more targeted therapies that reduce side effects are being developed, along with improved formulations that could offer better control of inflammatory diseases with fewer systemic effects.