Table of Contents
Introduction: Brief on PCOS and Weight Gain
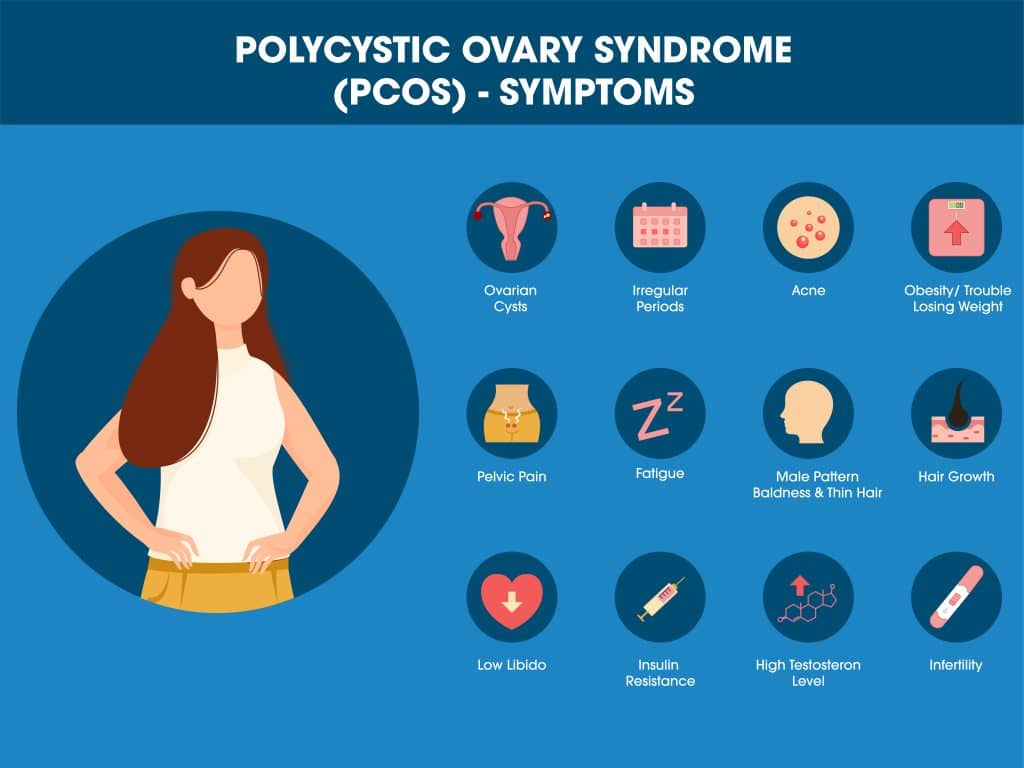
Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder affecting millions of women worldwide. Beyond irregular menstrual cycles, acne, and excessive hair growth, PCOS is a complex metabolic condition impacting overall health. One of the most distressing symptoms of PCOS is weight gain, which often exacerbates other symptoms, creating a vicious cycle. The emotional toll further complicates the condition, necessitating a comprehensive, multi-faceted treatment approach.
This article explores the intricate relationship between PCOS and weight gain. Unlike typical weight issues, weight gain in PCOS stems from physiological, hormonal, and psychological imbalances, making management challenging. We will delve into how hormonal imbalances, insulin resistance, metabolic syndrome, emotional well-being, and lifestyle choices contribute to this issue. Additionally, we will discuss treatment options, including lifestyle changes, medications, and psychological support.
Addressing weight gain is crucial because it can worsen other PCOS symptoms, such as menstrual irregularities and fertility issues, and increase the risk of diabetes, cardiovascular diseases, and certain cancers. Moreover, weight gain impacts self-esteem and mental health, highlighting the need for holistic management.
Understanding the mechanisms behind weight gain in PCOS is vital for effective treatment. Each woman’s experience with PCOS is unique, necessitating tailored treatment plans that address root causes rather than symptoms. This personalized approach promotes sustainable weight management and enhances physical and emotional well-being.
In summary, this article provides a comprehensive understanding of weight gain in PCOS. It aims to be a resource for women with PCOS, healthcare providers, and anyone interested in this disorder’s impact on body weight. By dissecting contributing factors, we offer strategies for managing weight gain, giving women with PCOS hope for a healthier, more balanced life.
What is PCOS? A Comprehensive Overview
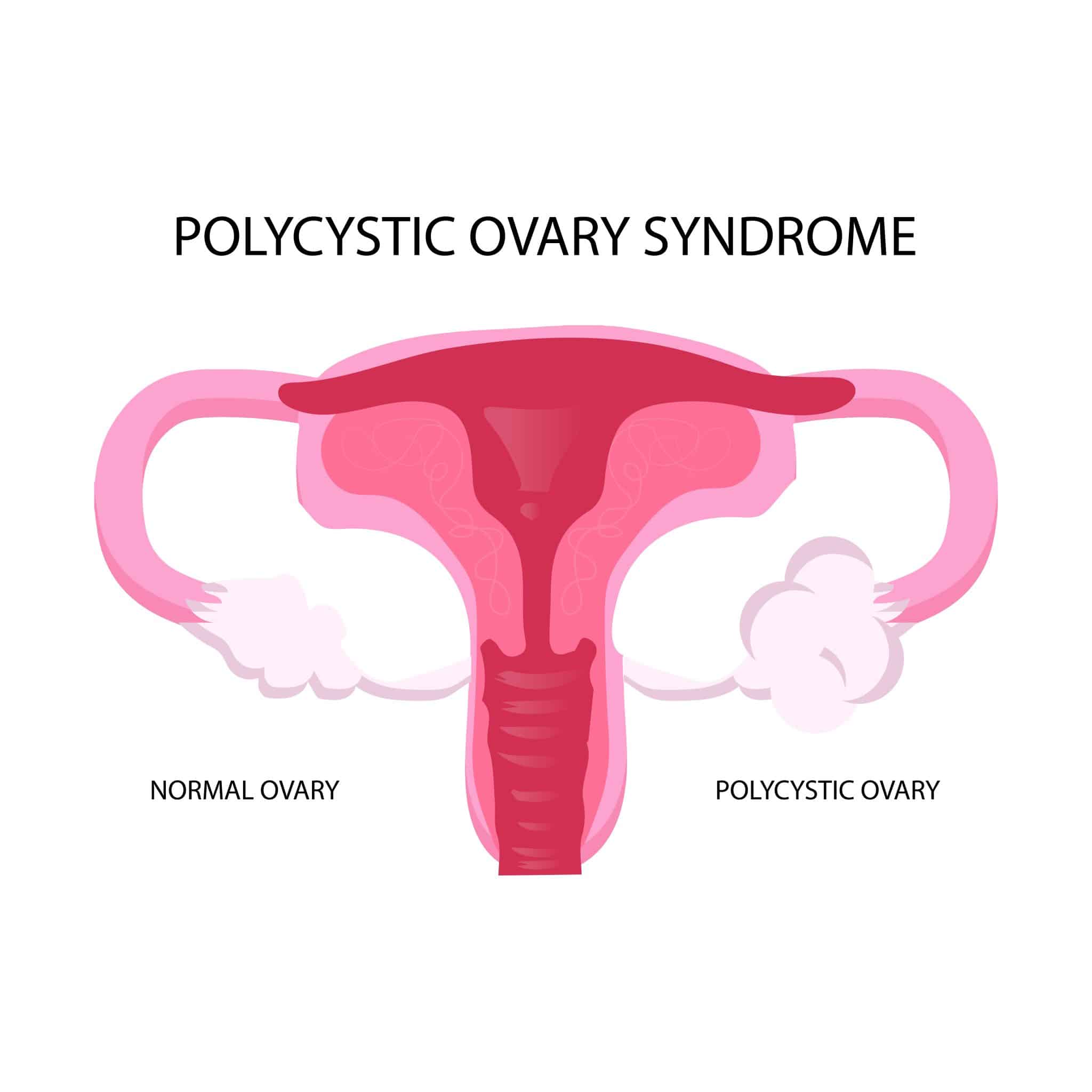
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder affecting 6-10% of women of reproductive age globally. Despite its prevalence, PCOS is frequently misunderstood and underdiagnosed. Symptoms range from irregular menstrual cycles, excessive body or facial hair (hirsutism), severe acne, and infertility to unexplained weight gain—a particularly distressing symptom we will explore in detail.
Diagnosing PCOS
PCOS is diagnosed using the Rotterdam criteria, requiring at least two of the following:
- Irregular or absent menstrual cycles.
- Clinical or biochemical signs of hyperandrogenism (elevated male hormones like testosterone).
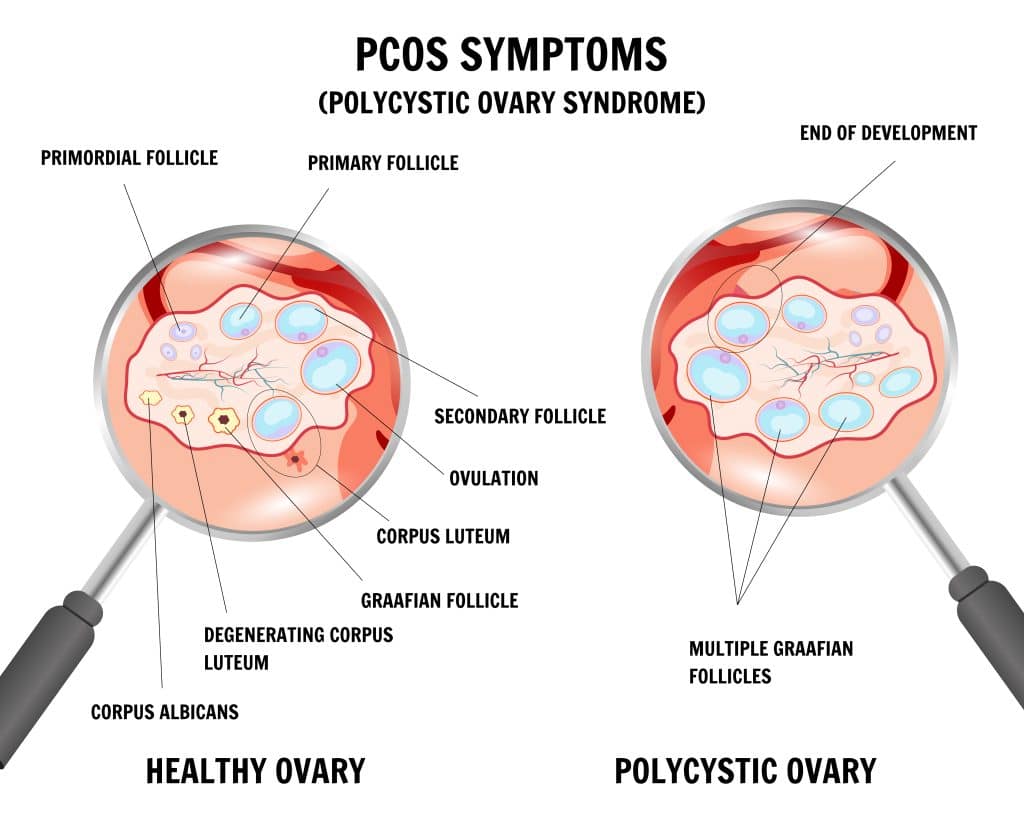
- Polycystic ovaries visible on an ultrasound.
Not all women with PCOS have polycystic ovaries or visible signs of hyperandrogenism, adding to the diagnostic challenge.
The Hormonal Imbalance
PCOS stems from a hormonal imbalance. Elevated androgens (male hormones present in both sexes) disrupt menstrual regulation, leading to irregularities, hirsutism, and acne.
Genetic and Environmental Factors
The exact cause of PCOS is unknown, but genetics and environment play significant roles. Many women with PCOS have a family history of the condition, indicating a genetic predisposition. Lifestyle factors, such as diet and physical activity, influence symptom severity. Researchers are also examining environmental factors, like exposure to endocrine-disrupting chemicals, for their impact on PCOS.
Beyond Reproductive Health
PCOS affects more than reproductive health. It often leads to insulin resistance, increasing the risk of Type 2 diabetes. Women with PCOS are more prone to metabolic syndrome, sleep apnea, and certain cancers. Managing PCOS requires a multidisciplinary approach involving gynecologists, endocrinologists, dermatologists, and nutritionists.
Understanding PCOS is crucial for effective management. If you suspect you have PCOS, seek medical advice for proper diagnosis and treatment. Lifestyle changes, such as a balanced diet and regular exercise, can help manage symptoms. Advocate for yourself and collaborate with healthcare providers to develop a comprehensive care plan tailored to your needs.
Emotional and Psychological Impact
PCOS doesn’t just affect the body; it deeply impacts mental health and overall quality of life. Women with PCOS are more likely to experience anxiety, depression, and other mood disorders. Physical symptoms such as weight gain, acne, and hirsutism can devastate self-esteem, creating a cycle of emotional distress that worsens PCOS symptoms.
PCOS is a complex disorder with diverse symptoms that vary greatly between individuals. This complexity can make diagnosis and management challenging, necessitating a holistic approach that considers both physical and emotional aspects.
Understanding the interplay of hormonal imbalances, metabolic factors, and emotional well-being is crucial for managing PCOS effectively. Addressing these elements comprehensively can break the cycle of distress and lead to better outcomes. Take charge of your health by seeking a multidisciplinary approach that targets both your body and mind.
The Physiology of Weight Gain: A Primer
Understanding weight gain starts with the basic energy equation: calories in versus calories out. Simply put, consuming more calories than you burn results in weight gain. However, this balance is influenced by complex physiological factors such as metabolism, hormones, and genetics.
The “set point” theory suggests that each person has a genetically determined weight range that their body strives to maintain. Deviations from this range trigger hormonal and metabolic responses to restore balance. Hormones like leptin and ghrelin, which control hunger and satiety, are key players in this regulation.
In conditions like PCOS, these regulatory pathways are often disrupted due to hormonal imbalances, making weight management even more challenging. Understanding these physiological intricacies can help in developing effective strategies for weight control.
Hormonal Imbalances in PCOS
Hormonal imbalances, especially elevated androgens, are key characteristics of PCOS. These “male hormones” can cause symptoms like excessive hair growth, acne, and irregular menstrual cycles. But how do they contribute to weight gain?
Hormones act as chemical messengers, regulating metabolism, hunger, and fat storage. In PCOS, hormonal imbalances disrupt these processes, leading to weight gain. Elevated androgens, for example, can cause insulin resistance, making weight loss difficult and creating a cycle of weight gain and hormonal imbalance.
Disrupted menstrual cycles add to the complexity. A regular cycle reflects a balance of hormones like estrogen and progesterone. In PCOS, this balance is lost, affecting metabolic processes and contributing to weight gain.
Insulin Resistance and PCOS
Insulin, produced in the pancreas, regulates blood sugar by allowing cells to absorb glucose for energy. Insulin resistance occurs when cells become less responsive to insulin, leading to higher blood sugar and insulin levels.
Insulin resistance plays a significant role in PCOS-related weight gain. Elevated insulin levels increase fat storage, especially in the abdomen. This relationship is bidirectional: PCOS can cause insulin resistance, and insulin resistance can worsen PCOS symptoms. About 50-70% of women with PCOS have some degree of insulin resistance, regardless of their weight.
Understanding insulin resistance is crucial. It not only contributes to weight gain but is also a precursor to Type 2 diabetes, heart disease, and certain cancers. Managing insulin levels is vital for weight control and overall health in women with PCOS.
Action Steps
- Monitor Hormones: Regularly check hormone levels with your doctor.
- Healthy Diet: Focus on a balanced diet low in processed sugars to manage insulin levels.
- Exercise Regularly: Physical activity helps regulate hormones and improve insulin sensitivity.
- Medication: Consider medications that target insulin resistance and hormonal imbalances.
- Regular Check-ups: Stay on top of your health with regular medical consultations to manage and mitigate PCOS symptoms.
The Metabolic Syndrome Connection
Metabolic syndrome, a cluster of conditions such as high blood sugar, increased blood pressure, excess abdominal fat, and abnormal cholesterol levels, significantly raises the risk of heart disease, stroke, and Type 2 diabetes. Alarmingly, women with PCOS are disproportionately affected, with up to 40% meeting the criteria for metabolic syndrome.
The link between these conditions is complex but crucial to understand. High insulin levels in both metabolic syndrome and PCOS drive increased androgen production in the ovaries, which in turn exacerbates insulin resistance, creating a vicious cycle. Each component of metabolic syndrome—high triglycerides, low HDL cholesterol, and high blood pressure—further contributes to weight gain and complicates weight loss efforts.
This intricate relationship necessitates a holistic approach to weight management in women with PCOS. Addressing just one aspect, like elevated blood sugar, is insufficient for long-term success. A comprehensive strategy is essential for effectively managing both conditions and improving overall health.
Emotional and Psychological Factors in PCOS Weight Management
Understanding weight gain in PCOS involves not only hormonal and metabolic factors but also emotional and psychological elements. Women with PCOS frequently experience higher stress, depression, and anxiety levels, which significantly contribute to weight gain.
When stressed, the body releases cortisol, the “stress hormone,” which promotes fat storage, particularly around the abdomen, complicating weight management. Additionally, stress and depression often lead to “emotional eating” of high-calorie, sugary, or fatty foods, further increasing weight.
The emotional burden of PCOS symptoms such as infertility, acne, or hirsutism heightens stress, creating a vicious cycle of emotional distress and weight gain. This bidirectional relationship means that emotional stress leads to weight gain, and the physical and emotional impact of excess weight increases psychological distress.
To effectively manage PCOS, a multi-faceted approach is essential, focusing on emotional well-being alongside hormonal and metabolic treatment. Addressing the psychological aspects is crucial for breaking the cycle of stress and weight gain, leading to more effective and sustainable weight management.
Action Steps:
- Seek Support: Engage in therapy or counseling to manage stress and emotional distress.
- Practice Mindfulness: Incorporate mindfulness and relaxation techniques to reduce cortisol levels.
- Healthy Coping Mechanisms: Replace emotional eating with healthier stress-relief methods like exercise or hobbies.
- Holistic Approach: Work with healthcare providers to address both the emotional and physical aspects of PCOS.
Compounding Effects of Lifestyle Choices
Lifestyle choices are crucial in weight management, especially for those with PCOS. Poor diet and lack of exercise can severely impact weight due to the metabolic and hormonal imbalances in PCOS. High intake of processed foods, sugars, and unhealthy fats worsens insulin resistance, fueling weight gain. Sedentary behavior exacerbates this problem, as physical inactivity reduces insulin sensitivity, leading to further weight gain and health issues like cardiovascular disease.
The good news: lifestyle interventions are highly effective. Research shows that even a modest weight loss of 5-10% significantly improves insulin sensitivity, menstrual regularity, and fertility. In short, adopting healthier habits not only aids weight loss but also alleviates other PCOS symptoms.
Take action now: Choose a balanced diet, rich in whole foods, lean proteins, and healthy fats. Incorporate regular physical activity into your routine. These changes will help you manage weight and improve overall health, particularly if you have PCOS.
Management and Treatment Options for Weight Gain in PCOS
Effectively managing weight gain in PCOS requires a comprehensive, multi-disciplinary approach due to its complexity involving hormonal imbalances, insulin resistance, emotional factors, and lifestyle choices. This approach often includes lifestyle interventions, pharmacotherapy, and psychological support.
Lifestyle Interventions
Lifestyle modification is the foundation of weight management in PCOS. A balanced diet rich in fruits, vegetables, lean proteins, and healthy fats is essential. Diets like the Mediterranean or low-glycemic index have proven effective in managing PCOS symptoms. Equally important is regular physical exercise, which not only aids in calorie burning but also improves insulin sensitivity and mental well-being. Tailoring these interventions to individual needs, such as opting for low-impact exercises like swimming or cycling for those with joint pain, enhances their effectiveness.
Pharmacotherapy
Medications play a crucial role in managing weight and other PCOS symptoms. Metformin, commonly used for Type 2 diabetes, can reduce insulin resistance and support weight loss when combined with lifestyle changes, though it may cause side effects like gastrointestinal distress.
Semaglutide is an emerging and promising option for weight management in PCOS. Originally developed for Type 2 diabetes, it mimics the hormone GLP-1 to regulate appetite, helping reduce caloric intake and promoting weight loss. Preliminary studies, including one published in The Lancet Diabetes & Endocrinology, show significant weight loss in adults with obesity. While further research specific to PCOS is needed, early results are encouraging.
Psychological Support
The emotional and psychological aspects of PCOS significantly impact weight management. Issues like emotional eating, body image concerns, and chronic stress are common and can hinder weight loss efforts. Cognitive-behavioral therapy (CBT) effectively addresses these issues by helping women understand and change negative behavior patterns. Support groups and counseling also provide emotional support, making the weight loss journey less isolating.
Integrated Approach
Given PCOS’s multifaceted nature, an integrated approach is often the most effective. This involves a team of healthcare providers, including a gynecologist, endocrinologist, dietitian, and psychologist, working together to offer comprehensive care. Such a strategy allows for simultaneous targeting of various contributing factors like insulin resistance, hormonal imbalance, and emotional eating. A holistic, customized approach not only makes weight management more achievable but also improves other PCOS symptoms and overall well-being.
By adopting this integrated, tailored strategy, women with PCOS can effectively manage their weight, enhance their health, and improve their quality of life.
Conclusion: A Multi-Faceted Approach to Managing Weight Gain in PCOS
Managing weight gain in PCOS is a complex challenge, involving physiological barriers, hormonal imbalances, psychological burdens, and significant lifestyle changes. Understanding this complexity is the first step toward effective management. By addressing each contributing factor, we can create tailored interventions that target root causes, not just symptoms, leading to a more holistic treatment approach.
Weight gain in PCOS is closely linked to other symptoms like menstrual irregularities, infertility, and mental health issues such as depression and anxiety. Successful weight management can improve the overall quality of life for women with PCOS by reducing insulin resistance, improving menstrual regularity, and enhancing fertility.
PCOS manifests differently in each individual, necessitating personalized treatment plans. Healthcare providers must consider various factors, including lifestyle, existing medical conditions, emotional well-being, and personal preferences. While medications like Metformin or semaglutide can be beneficial for some, others might respond better to lifestyle interventions alone.
The field of PCOS treatment is evolving. As our understanding of the condition deepens, newer treatment options, such as semaglutide originally designed for Type 2 diabetes, are showing promise in managing weight and other metabolic aspects of PCOS. Ongoing research offers hope for more effective and targeted treatments.
Emotional and psychological well-being are crucial in managing PCOS. Stress, depression, and anxiety can contribute to weight gain and hinder weight loss. Incorporating psychological support through counseling or cognitive-behavioral therapy (CBT) can provide women with tools to break the cycle of emotional eating or stress-induced weight gain, essential for long-term success.
The relationship between PCOS and weight gain is multi-dimensional, influenced by physiological, hormonal, and psychological factors. Managing this condition requires a multi-faceted approach. While pharmacotherapy offers new treatment avenues, lifestyle modifications remain essential. Combined with the right medication and emotional support, women can manage their weight and aspire to a healthier, more balanced life. Start your journey today to manage PCOS-related weight gain effectively.
Research Citations
Here are some research citations discussing how PCOS (Polycystic Ovary Syndrome) can cause weight gain:
- Lim SS, Davies MJ, Norman RJ, Moran LJ. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(6):618-637. doi:10.1093/humupd/dms030
- Teede HJ, Joham AE, Paul E, et al. Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity (Silver Spring). 2013;21(8):1526-1532. doi:10.1002/oby.20441
- Cassar S, Misso ML, Hopkins WG, Shaw CS, Teede HJ, Stepto NK. Insulin resistance in polycystic ovary syndrome: a systematic review and meta-analysis of euglycaemic-hyperinsulinaemic clamp studies. Hum Reprod. 2016;31(11):2619-2631. doi:10.1093/humrep/dew243
- Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific statement on the diagnostic criteria, epidemiology, pathophysiology, and molecular genetics of polycystic ovary syndrome. Endocr Rev. 2015;36(5):487-525. doi:10.1210/er.2015-1018
- Barber TM, McCarthy MI, Wass JA, Franks S. Obesity and polycystic ovary syndrome. Clin Endocrinol (Oxf). 2006;65(2):137-145. doi:10.1111/j.1365-2265.2006.02586.x
- Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011;(7):CD007506. doi:10.1002/14651858.CD007506.pub2
- Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(5):748-758. doi:10.1093/humupd/dmu012
- Lim SS, Kakoly NS, Tan JWJ, et al. Metabolic syndrome in polycystic ovary syndrome: a systematic review, meta-analysis and meta-regression. Obes Rev. 2019;20(2):339-352. doi:10.1111/obr.12776
- Legro RS, Arslanian SA, Ehrmann DA, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565-4592. doi:10.1210/jc.2013-2350
- Hirschberg AL. Polycystic ovary syndrome, obesity and reproductive implications. Womens Health (Lond). 2009;5(5):529-540. doi:10.2217/whe.09.34
These studies provide insights into the mechanisms underlying weight gain in women with PCOS, including insulin resistance, hormonal imbalances, and lifestyle factors, highlighting the complex interplay between metabolic disturbances and reproductive health in PCOS.
Questions and Answers: PCOS and Weight Gain
Women with PCOS often gain weight due to a combination of hormonal imbalances and insulin resistance. Elevated levels of androgens (male hormones) and insulin can disrupt normal metabolic processes, leading to increased fat storage, especially in the abdominal area.
Yes, it can be more challenging. The hormonal imbalances and insulin resistance associated with PCOS can slow down metabolism and increase cravings, making it harder to lose weight through conventional diet and exercise alone.
Yes. While diet plays a role in weight management, PCOS-related weight gain can occur even without overeating. Hormonal imbalances and insulin resistance can lead to weight gain by altering the way the body processes and stores fat.
Yes, treating PCOS can aid in weight loss. Effective treatment, which may include lifestyle changes, medication, and hormonal therapy, can help regulate menstrual cycles, improve insulin sensitivity, and balance hormone levels, all of which can contribute to weight loss.
Diets that focus on whole foods, low-glycemic index carbohydrates, and are rich in fiber, such as the Mediterranean diet, have been found beneficial. Reducing processed foods and sugars can also improve insulin sensitivity and aid in weight loss.
Absolutely. Regular exercise, especially a combination of aerobic and resistance training, can improve insulin sensitivity, boost metabolism, and help with weight management in PCOS.
Insulin resistance in PCOS causes the body’s cells to be less responsive to insulin, leading to higher insulin levels. High insulin levels promote fat storage and can increase hunger and cravings, contributing to weight gain.
Yes, certain medications like Metformin, which improves insulin sensitivity, and newer drugs like semaglutide, can assist in weight management. However, these should be used as part of a broader treatment plan under medical supervision.
Yes, women with PCOS often experience more fat storage around their abdomen, known as visceral fat, which is linked to insulin resistance and can increase the risk of other health issues like heart disease and diabetes.
Definitely. Even a modest weight loss of 5-10% of body weight can lead to significant improvements in PCOS symptoms, including menstrual regularity, reduced androgen levels, and improved chances of conception for those seeking to become pregnant.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.