Table of Contents
Section 1: Introduction
In the realm of endocrinology and metabolic health, the intersection between pharmacological advancements and autoimmune disorders presents a fertile ground for exploration and discovery. Among the most compelling subjects of this intersection is the relationship between Semaglutide, a novel therapeutic agent, and Hashimoto’s thyroiditis, the most common form of thyroid autoimmunity. This article embarks on a journey to unravel the intricacies of this relationship, guided by the queries most frequently posed by the curious minds of patients, healthcare providers, and researchers alike.
Semaglutide, originally approved for the treatment of type 2 diabetes, has rapidly gained recognition for its efficacy in weight management, which is of particular interest given the complex interplay between metabolic disorders and thyroid function. Its mechanism of action, mimicking the incretin hormone GLP-1, not only aids in glucose homeostasis but also has profound effects on appetite suppression and weight loss. These attributes have positioned Semaglutide as a potentially transformative treatment option for individuals battling obesity, a condition that afflicts a significant portion of the global population and is a known risk factor for numerous chronic diseases.
Concurrently, Hashimoto’s thyroiditis emerges as a pivotal concern within the thyroid disorder spectrum, affecting millions worldwide. Characterized by an autoimmune attack against the thyroid gland, Hashimoto’s leads to a gradual decline in thyroid function, culminating in hypothyroidism. This condition is fraught with symptoms such as weight gain, lethargy, cold intolerance, and a host of other metabolic derangements, significantly impairing the quality of life of those affected.
The confluence of Semaglutide’s therapeutic potential with the management of Hashimoto’s thyroiditis ignites a series of pertinent inquiries. Patients and clinicians alike are keen to understand whether Semaglutide can ameliorate some of the metabolic challenges faced by individuals with Hashimoto’s, particularly in the realm of weight management. Moreover, there’s a burgeoning curiosity about the safety profile of Semaglutide in the context of autoimmune thyroid conditions, its effects on thyroid hormone levels, and the broader implications for thyroid health.
Addressing these queries requires a deep dive into the existing body of research, clinical trials, and expert opinions to delineate the scope of Semaglutide’s application for individuals with Hashimoto’s thyroiditis. It necessitates a balanced examination of potential benefits against the backdrop of safety concerns, particularly given the hormonal sensitivities inherent to thyroid disorders. As this article unfolds, it aims to shed light on these complex dynamics, offering a comprehensive overview that aligns with the most sought-after information on search engines and beyond.
By navigating through the layers of clinical evidence, patient experiences, and expert insights, this exploration seeks to empower readers with a nuanced understanding of how Semaglutide could potentially interface with the management of Hashimoto’s thyroiditis. In doing so, it aspires to contribute to a more informed dialogue between patients and healthcare providers, facilitating decisions that enhance health outcomes and improve the lives of those navigating the challenges of autoimmune thyroid disorders.
Section 2: What is Semaglutide, and How Does It Work?
Semaglutide stands as a beacon of innovation in the pharmacological management of type 2 diabetes and obesity, marking a significant advancement in our approach to these pervasive health challenges. As a glucagon-like peptide-1 (GLP-1) receptor agonist, Semaglutide mimics the action of endogenous GLP-1, a hormone integral to glucose metabolism and appetite regulation. This synthetic analogue has been meticulously designed to enhance glycemic control and promote weight loss, embodying the strides made in diabetes care and weight management strategies.
The journey of Semaglutide from development to clinical application illuminates the complexities of metabolic regulation. GLP-1, produced in the intestines in response to food intake, plays a pivotal role in the enteroinsular axis, a system that bridges nutrient absorption with insulin secretion. By activating GLP-1 receptors, Semaglutide augments the release of insulin from pancreatic beta cells in a glucose-dependent manner, thus reducing the risk of hypoglycemia—a notable advantage over some other diabetes medications. Concurrently, it inhibits the secretion of glucagon, a hormone that increases blood glucose levels, thereby addressing hyperglycemia from both sides of the metabolic equation.
Beyond glycemic control, Semaglutide exerts a profound impact on weight regulation. By simulating GLP-1’s action, it delays gastric emptying and promotes a sense of satiety, leading to a reduction in calorie intake. This mechanism is particularly beneficial for individuals with obesity, offering a therapeutic pathway to weight loss that transcends dietary restrictions and exercise alone. The weight loss achieved with Semaglutide is not just a matter of aesthetics but is crucial for mitigating the myriad health risks associated with obesity, including cardiovascular disease, hypertension, and type 2 diabetes itself.
The advent of Semaglutide also highlights the importance of patient-centric treatment options in the management of chronic conditions like type 2 diabetes and obesity. Its introduction into the therapeutic arsenal signifies a shift towards treatments that not only address the symptoms and underlying causes of these conditions but also align with patients’ lifestyles and preferences. This patient-centric approach is crucial in chronic disease management, where adherence and long-term engagement with treatment regimens are key determinants of success.
Semaglutide’s mode of administration, a once-weekly injection, represents a significant advantage in terms of convenience and adherence compared to daily injections or multiple daily oral medications. This aspect of treatment is particularly appealing to patients who may struggle with the daily routines required by other diabetes or weight management medications. Moreover, the efficacy of Semaglutide in reducing HbA1c levels and facilitating weight loss, as demonstrated in numerous clinical trials, provides patients with tangible outcomes that can motivate continued adherence and engagement with their treatment plans.
The role of Semaglutide extends beyond glycemic control and weight loss. Its impact on satiety and food intake can lead to improvements in eating behaviors, potentially addressing some of the psychological aspects of obesity and diabetes management. By reducing the urge to eat excessively or make poor food choices, Semaglutide can help patients adopt healthier eating patterns, which are crucial for long-term disease management and overall health.
Furthermore, the cardiovascular benefits observed with Semaglutide use, including the reduction in the risk of major adverse cardiovascular events, underscore its potential to address the multifaceted risks associated with type 2 diabetes and obesity. Cardiovascular disease remains the leading cause of morbidity and mortality in patients with diabetes, and interventions that can mitigate this risk are invaluable.
It is also essential to consider the psychological impact of chronic disease management on patients. Semaglutide’s ability to produce noticeable weight loss and improve glycemic control can significantly enhance patients’ quality of life and psychological well-being. The sense of achievement from seeing tangible results can be a powerful motivator, fostering a more positive outlook towards managing their condition.
However, the journey with Semaglutide is not devoid of challenges. Patients and healthcare providers must navigate potential side effects, such as gastrointestinal symptoms, and ensure that the treatment is suitable for the individual’s health profile. Regular follow-ups, monitoring, and adjustments to the treatment plan are essential components of a successful patient-centric approach, ensuring that the benefits of Semaglutide are maximized while minimizing any adverse effects. The advent of Semaglutide marks a significant milestone in the treatment of type 2 diabetes and obesity, offering a new horizon of patient-centric care. By integrating this innovative treatment into a comprehensive management plan that includes lifestyle modifications, psychological support, and regular medical oversight, healthcare providers can offer their patients a path to better health outcomes and an improved quality of life.
Section 3: What is Hashimoto's Thyroiditis?
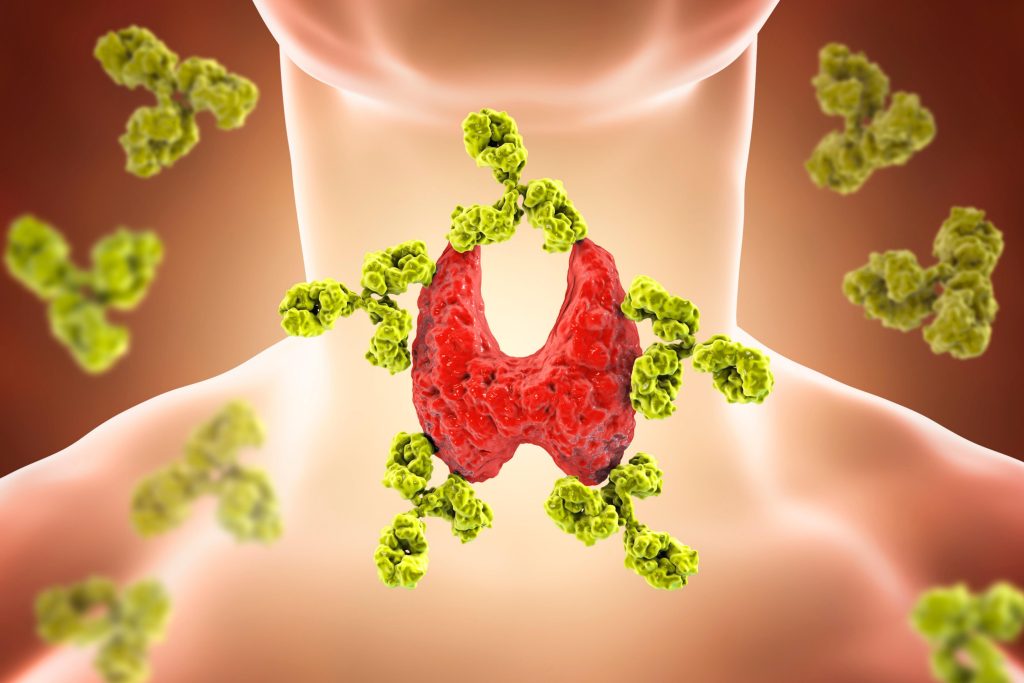
Hashimoto’s Thyroiditis, named after the Japanese physician Hakaru Hashimoto who first described it in the early 20th century, is an autoimmune disorder that targets the thyroid gland, leading to chronic thyroiditis and, often, hypothyroidism. This condition represents the most common cause of thyroid gland failure in regions with sufficient iodine intake, affecting millions worldwide. Hashimoto’s thyroiditis is characterized by the immune system’s aberrant attack on thyroid cells, mistaking them for foreign invaders and gradually destroying them, thereby impairing the thyroid’s ability to produce hormones essential for metabolism and energy regulation.
The pathophysiology of Hashimoto’s thyroiditis is complex and involves a combination of genetic predisposition and environmental factors. The immune system produces antibodies against thyroid peroxidase (TPO) and thyroglobulin, two key enzymes involved in thyroid hormone production. This autoimmune response leads to inflammation and damage to the thyroid tissue, resulting in decreased hormone production. The etiology of Hashimoto’s is multifactorial, with genetic, hormonal, and environmental influences such as selenium deficiency, radiation exposure, and possibly viral infections playing contributory roles.
Clinically, Hashimoto’s thyroiditis manifests in a spectrum of symptoms that reflect the degree of hypothyroidism. These symptoms can be subtle and insidious, making the condition challenging to diagnose in its early stages. Common symptoms include fatigue, weight gain, cold intolerance, dry skin, hair loss, muscle weakness, constipation, and depressive mood. The condition also has significant implications for reproductive health, contributing to infertility and pregnancy complications.
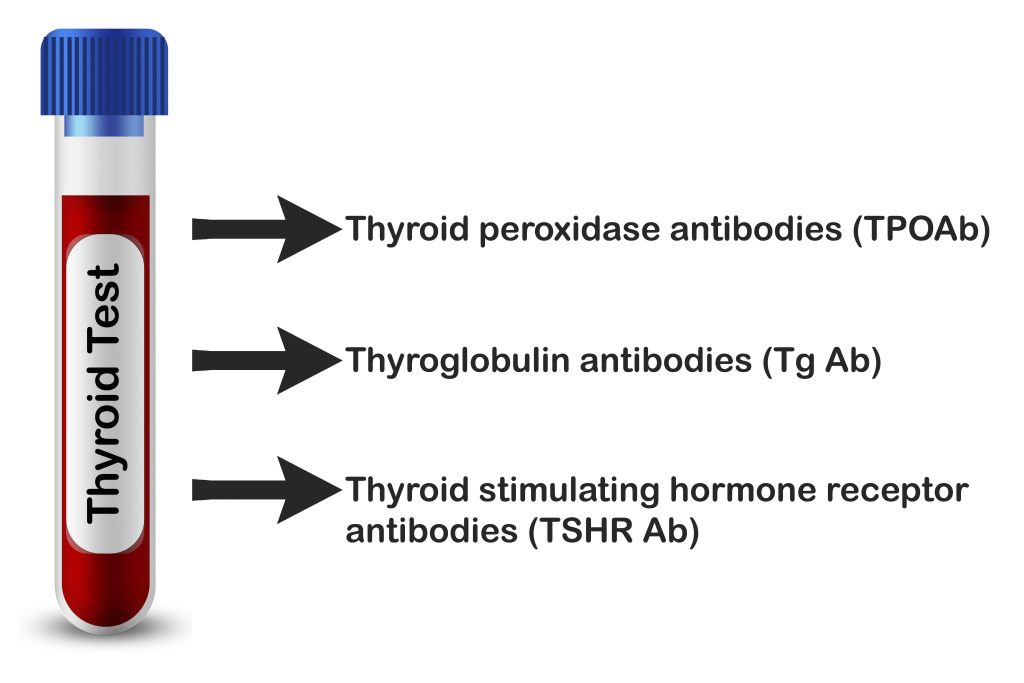
Diagnosis of Hashimoto’s thyroiditis primarily relies on serological tests to detect elevated levels of thyroid antibodies, alongside assessments of thyroid hormone levels, particularly Thyroid Stimulating Hormone (TSH) and Free Thyroxine (T4). Ultrasound imaging of the thyroid can also provide valuable information on the gland’s structure and any potential abnormalities indicative of autoimmune thyroiditis.
The management of Hashimoto’s thyroiditis centers around hormone replacement therapy, typically with levothyroxine, to normalize thyroid hormone levels and alleviate symptoms. However, treatment approaches must be individualized, taking into account the patient’s symptoms, hormone levels, and overall health status. Despite the availability of effective treatment for hypothyroidism, the autoimmune nature of Hashimoto’s means that ongoing monitoring and adjustments in therapy may be necessary over the patient’s lifetime.
Understanding Hashimoto’s thyroiditis is crucial not only for those directly affected by the condition but also for healthcare providers. It underscores the importance of recognizing the signs and symptoms of thyroid dysfunction and the need for a comprehensive approach to diagnosis and management. As research continues to unravel the complexities of autoimmune diseases, the hope is that more targeted and effective treatments for Hashimoto’s thyroiditis and its associated conditions will emerge, improving the quality of life for those affected.
Section 4: Can Semaglutide Affect Thyroid Function?
The exploration of Semaglutide’s impact on thyroid function is a subject of considerable scientific interest, given the medication’s widespread use for diabetes and obesity management. Semaglutide, as a GLP-1 receptor agonist, operates primarily through pathways that influence glucose metabolism and appetite regulation. However, the systemic nature of its action raises questions about its effects on other endocrine organs, including the thyroid gland.
Preclinical studies and clinical trials have scrutinized the relationship between GLP-1 receptor agonists like Semaglutide and thyroid function. In rodent models, a notable concern has been the observation of C-cell hyperplasia and medullary thyroid carcinomas associated with chronic administration of GLP-1 receptor agonists. These findings have propelled further research to understand whether such effects translate to humans.
The human thyroid gland differs from rodents in several key aspects, including a lower density of GLP-1 receptors on C-cells, which are responsible for calcitonin production. Calcitonin, a hormone involved in calcium homeostasis, has been a focal point in assessing Semaglutide’s safety profile due to its link to C-cell pathology. To date, clinical data have not demonstrated a direct causative relationship between Semaglutide use and increased risk of thyroid C-cell tumors in humans. However, regulatory agencies and clinical guidelines emphasize the importance of vigilance and caution, particularly among patients with a personal or family history of medullary thyroid cancer or those with Multiple Endocrine Neoplasia syndrome type 2.
Beyond the concern for C-cell pathology, the broader question of how Semaglutide may influence thyroid hormone levels and thyroid function in general remains under investigation. Some studies suggest that GLP-1 receptor agonists can affect thyroid hormone metabolism and possibly TSH levels, albeit the clinical significance of these findings is still being evaluated. For individuals with thyroid disorders, such as Hashimoto’s thyroiditis, the potential for drug-induced changes in thyroid function necessitates careful consideration and monitoring.
In clinical practice, the approach to using Semaglutide in patients with existing thyroid conditions involves a nuanced assessment of benefits versus risks. It is essential for healthcare providers to monitor thyroid function tests, including TSH and free thyroid hormones, before initiating Semaglutide and periodically thereafter. Patients should be informed about the potential signs and symptoms of thyroid dysfunction and advised to seek medical attention if they experience any such changes. While Semaglutide represents a significant advancement in the management of diabetes and obesity, its interaction with thyroid function highlights the complexities of endocrine pharmacotherapy. Ongoing research and post-marketing surveillance continue to play pivotal roles in ensuring the safe and effective use of this medication, particularly among individuals with underlying thyroid disorders.
Section 5: Is Semaglutide Safe for People with Hashimoto's?
The question of Semaglutide’s safety for individuals with Hashimoto’s thyroiditis is pivotal, given the medication’s increasing use for managing type 2 diabetes and obesity—conditions that often coexist with thyroid disorders. Hashimoto’s, an autoimmune disease that typically results in hypothyroidism, requires careful consideration when introducing any new medication, particularly those with systemic effects like Semaglutide.
In evaluating Semaglutide’s safety, it’s essential to consider both the pharmacological action of the drug and the pathophysiological characteristics of Hashimoto’s. Semaglutide works by mimicking the incretin hormone GLP-1, enhancing insulin secretion, suppressing glucagon release, and delaying gastric emptying. These actions contribute to improved glycemic control and weight loss but also prompt a careful assessment of their implications for thyroid function.
To date, clinical trials and observational studies have not shown direct adverse effects of Semaglutide on thyroid function in the general population. However, these studies often exclude individuals with active thyroid disorders or do not specifically analyze this subgroup. The theoretical concern for patients with Hashimoto’s revolves around the autoimmune nature of the disease and the potential for metabolic changes induced by Semaglutide to influence thyroid hormone levels or autoimmunity itself.
For individuals with Hashimoto’s, the primary treatment is thyroid hormone replacement, typically with levothyroxine, to achieve euthyroid status. When introducing Semaglutide, healthcare providers must monitor thyroid function tests closely. Changes in weight and metabolism induced by Semaglutide could necessitate adjustments in levothyroxine dosage to maintain optimal thyroid hormone levels.
Moreover, the immune-modulatory effects of GLP-1 receptor agonists, including Semaglutide, are an area of ongoing research. While there is no current evidence to suggest that Semaglutide exacerbates autoimmune thyroiditis, understanding the complex interplay between metabolic regulation, weight loss, and autoimmunity is essential. This knowledge gap underscores the need for clinical vigilance and patient-centered care, ensuring that any signs of thyroid dysfunction are promptly addressed.
While Semaglutide offers significant benefits for weight management and glycemic control, its use in individuals with Hashimoto’s thyroiditis necessitates a tailored approach. This strategy should include baseline and periodic monitoring of thyroid function tests, awareness of the signs and symptoms of thyroid imbalance, and open communication between patients and healthcare providers. As the therapeutic landscape evolves, so too will our understanding of how best to integrate treatments like Semaglutide into the comprehensive care of individuals with Hashimoto’s, balancing efficacy with safety to optimize health outcomes.
Section 6: What Are the Symptoms of Semaglutide Overdose and How to Manage It?
Semaglutide overdose is a critical consideration given the drug’s potent effects on glucose metabolism and appetite suppression. While the therapeutic window for Semaglutide is generally wide, exceeding the recommended dosage can lead to adverse reactions, which necessitates an understanding of the symptoms and management strategies for such scenarios.
The symptoms of Semaglutide overdose primarily reflect its pharmacological actions, intensifying its side effects. These can include severe gastrointestinal disturbances, such as nausea, vomiting, diarrhea, and abdominal pain, which are common even at therapeutic doses but may be exacerbated. Additionally, hypoglycemia, although more likely in combination with other glucose-lowering medications, is a potential risk associated with overdose due to Semaglutide’s insulinotropic effects.
Beyond these immediate symptoms, there is a concern for delayed gastric emptying, a hallmark effect of GLP-1 receptor agonists. In the context of an overdose, this could potentially lead to prolonged gastrointestinal symptoms and impact the absorption of orally ingested medications, complicating the clinical picture.
Management of Semaglutide overdose is primarily supportive, focusing on the symptoms presented. There is no specific antidote for Semaglutide; therefore, treatment involves managing the acute symptoms and preventing further complications. For gastrointestinal symptoms, this may include the use of antiemetics for nausea, IV fluids for dehydration, and electrolyte repletion if necessary. For hypoglycemia, the administration of glucose is warranted, with careful monitoring of blood glucose levels until stabilization.
Preventing an overdose of Semaglutide underscores the importance of patient education and adherence to prescribed dosages. Healthcare providers should ensure patients understand the correct usage of the drug, including dosing intervals and the importance of not exceeding the recommended dose. Additionally, given Semaglutide’s subcutaneous administration, proper training on injection techniques and the use of dosing devices is crucial to avoid accidental overdose.
In the event of a suspected overdose, immediate medical attention is essential. Healthcare professionals should assess the patient’s symptoms, vital signs, and glucose levels, providing supportive care tailored to the clinical manifestations. Monitoring should continue until the patient’s symptoms resolve and their clinical status stabilizes. While Semaglutide overdose is rare, recognizing the symptoms and understanding the management principles are crucial for healthcare providers. Through patient education, careful dosing, and vigilant monitoring, the risks associated with overdose can be minimized, ensuring that patients continue to benefit from Semaglutide’s therapeutic potential safely.

Section 7: The Impact of Semaglutide on Weight Loss in Patients with Hashimoto's Thyroiditis
The burgeoning interest in Semaglutide’s utility extends into its potential to facilitate weight loss, particularly among individuals grappling with Hashimoto’s Thyroiditis. This autoimmune condition, characterized by the gradual diminution of thyroid function, often culminates in hypothyroidism, a state intrinsically linked to metabolic slowdown, weight gain, and difficulty shedding excess weight through conventional means. The introduction of Semaglutide, a GLP-1 receptor agonist, into the therapeutic landscape presents a novel avenue for addressing these challenges, albeit with nuances that necessitate a comprehensive understanding of its implications.
Semaglutide’s mechanism of action, primarily through the enhancement of insulin secretion, suppression of glucagon release, and delay in gastric emptying, positions it as a potent agent for weight management. These effects not only contribute to improved glycemic control but also to a reduction in appetite and caloric intake, facilitating weight loss. For patients with Hashimoto’s Thyroiditis, where metabolic rates are inherently reduced due to decreased thyroid hormone levels, Semaglutide offers a glimmer of hope in combating the weight gain that often exacerbates their condition.
Clinical trials and observational studies have documented the efficacy of Semaglutide in promoting significant weight loss in the general population, including individuals with type 2 diabetes and obesity. However, the specific impact on patients with Hashimoto’s Thyroiditis warrants particular attention. The interplay between Semaglutide-induced weight loss and thyroid hormone replacement therapy— a cornerstone in the management of Hashimoto’s—raises pertinent questions regarding dosage adjustments, metabolic effects, and overall thyroid stability.
Moreover, the potential for Semaglutide to indirectly affect thyroid function through weight loss-induced metabolic changes underscores the need for vigilant monitoring. Weight loss can alter the pharmacokinetics of levothyroxine, the synthetic thyroid hormone used to treat hypothyroidism, potentially necessitating adjustments in dosage to maintain euthyroid status. This dynamic interplay highlights the importance of a multidisciplinary approach, involving endocrinologists, primary care physicians, and dietitians, to optimize outcomes for patients with Hashimoto’s undergoing treatment with Semaglutide.
In light of these considerations, further research is imperative to delineate the long-term effects of Semaglutide on weight management and thyroid parameters in Hashimoto’s Thyroiditis. Such studies should aim to evaluate not only the efficacy and safety of Semaglutide in this unique population but also the optimal strategies for integrating it into the broader therapeutic regimen. Through rigorous investigation and clinical acumen, the potential of Semaglutide to improve the quality of life for individuals with Hashimoto’s Thyroiditis can be fully realized, marking a significant advancement in the management of this challenging condition.
Section 8: Monitoring and Adjusting Semaglutide Therapy in Hashimoto's Patients
The integration of Semaglutide therapy in patients with Hashimoto’s Thyroiditis demands a nuanced approach to monitoring and adjusting treatment to ensure optimal outcomes. Given the complex interrelationship between thyroid function, metabolic health, and the pharmacodynamics of Semaglutide, healthcare providers must employ a vigilant, patient-centric strategy to navigate these waters effectively.
The cornerstone of this approach lies in the comprehensive assessment of thyroid function before initiating Semaglutide therapy. Baseline measurements of Thyroid Stimulating Hormone (TSH) and free thyroxine (FT4) levels are imperative to establish the patient’s thyroid status. These initial evaluations serve as a benchmark, guiding the titration of thyroid hormone replacement therapy and informing the decision-making process regarding the appropriateness of Semaglutide.
Upon commencement of Semaglutide, periodic monitoring of thyroid function tests becomes crucial. The interplay between Semaglutide-induced weight loss and thyroid hormone metabolism may necessitate adjustments in levothyroxine dosage to maintain euthyroidism. Moreover, given the potential for Semaglutide to influence gastrointestinal motility, absorption dynamics of orally administered levothyroxine may also shift, further complicating the therapeutic landscape.
Beyond thyroid function, comprehensive metabolic monitoring is paramount. This includes regular assessments of glycemic control in patients with concomitant diabetes, lipid profiles, and markers of cardiovascular risk. Weight and body composition should be systematically evaluated, allowing for the tailored adjustment of Semaglutide dosage based on efficacy, tolerability, and the achievement of weight management goals.
Patient education and engagement play a pivotal role in the successful management of Hashimoto’s Thyroiditis with Semaglutide therapy. Patients should be informed of the potential side effects of Semaglutide, including gastrointestinal symptoms, and the importance of adherence to both Semaglutide and thyroid hormone replacement therapy. Empowering patients with knowledge about the signs of hypo- or hyperthyroidism, and when to seek medical attention, fosters a proactive approach to managing their condition. The management of Hashimoto’s Thyroiditis with Semaglutide therapy is a multifaceted endeavor that requires a thorough understanding of the intricate relationship between thyroid function and metabolic health. Through diligent monitoring, individualized treatment adjustments, and patient empowerment, healthcare providers can navigate the challenges and opportunities presented by Semaglutide, optimizing care for this unique patient population.
Section 9: Are There Any Alternatives to Semaglutide for Weight Loss in Hashimoto's Patients?
For individuals with Hashimoto’s Thyroiditis struggling with weight management, the search for effective treatment options is paramount. While Semaglutide has shown promise in aiding weight loss and improving metabolic health, it’s crucial to explore alternative therapies that can offer comparable benefits, especially for those who may not tolerate or respond well to Semaglutide. This exploration must consider the intricate balance between managing autoimmune thyroiditis and achieving weight loss goals.
Lifestyle Modifications: The foundation of any weight loss strategy, regardless of underlying health conditions, involves comprehensive lifestyle modifications. This includes tailored dietary plans that focus on nutrient-dense, anti-inflammatory foods to support thyroid health and metabolic function. Regular physical activity, adapted to the individual’s capability and energy levels, also plays a critical role in weight management and overall well-being.
Thyroid Hormone Optimization: For patients with Hashimoto’s, achieving optimal thyroid hormone levels is a cornerstone of managing weight. Adjusting levothyroxine doses to ensure euthyroidism can significantly impact metabolic rate and energy levels, aiding in weight loss efforts.
Other Medications: Beyond Semaglutide, several medications can assist in weight management. Metformin, traditionally used in type 2 diabetes, has shown some efficacy in weight loss, especially in individuals with insulin resistance. Bupropion/naltrexone (Contrave) and phentermine/topiramate (Qsymia) are other prescription medications approved for weight management that may be considered, depending on the patient’s overall health profile.
Bariatric Surgery: In cases of severe obesity where traditional methods have failed, and when medically appropriate, bariatric surgery may be an option. This intervention has shown significant long-term success in weight loss and the resolution of comorbid conditions, including type 2 diabetes. However, the decision for surgery requires careful evaluation of the risks and benefits, especially in the context of autoimmune thyroid disease.
Supplemental Support: Certain supplements, such as selenium and zinc, have been studied for their potential to support thyroid function and overall health in individuals with Hashimoto’s. While supplements alone are unlikely to result in significant weight loss, they may complement other strategies by optimizing thyroid health.
Managing weight in patients with Hashimoto’s Thyroiditis requires a multifaceted approach that goes beyond pharmacotherapy. A comprehensive treatment plan should incorporate lifestyle interventions, optimize thyroid hormone therapy, consider alternative medications, and, in selected cases, evaluate the appropriateness of surgical options. Collaboration between endocrinologists, nutritionists, and primary care providers is essential to tailor the most effective weight management strategy for each individual.
Section 10: How Should Semaglutide Be Administered in the Context of Hashimoto's?
Administering Semaglutide in patients with Hashimoto’s Thyroiditis demands careful consideration of timing, dosing, and monitoring to ensure therapeutic efficacy while minimizing potential side effects. Given the complexity of managing an autoimmune thyroid condition alongside metabolic or weight-related issues, a strategic approach to Semaglutide therapy is essential.
Starting Dose and Titration: Semaglutide treatment typically begins with a low dose to minimize gastrointestinal side effects, with gradual titration to the effective dose over several weeks. This cautious approach is especially important in Hashimoto’s patients, who may have sensitivities to medication adjustments due to their underlying thyroid condition.
Monitoring Thyroid Function: Regular monitoring of thyroid function tests (TFTs) is crucial when initiating or adjusting Semaglutide therapy in Hashimoto’s patients. TFTs should be checked before starting treatment, during dose escalation, and periodically thereafter. This helps to ensure that thyroid hormone replacement therapy remains optimized, adjusting the dose as necessary in response to weight loss or changes in metabolism induced by Semaglutide.
Managing Side Effects: Gastrointestinal side effects are common with Semaglutide and can include nausea, vomiting, diarrhea, and abdominal pain. Patients should be counseled on strategies to manage these side effects, such as eating smaller, more frequent meals and staying hydrated. If side effects are severe, temporary dose reduction or discontinuation may be necessary.
Integration with Lifestyle Modifications: Semaglutide therapy should be part of a broader lifestyle modification plan, including diet, exercise, and stress management, to maximize weight loss and improve metabolic health in Hashimoto’s patients. Collaboration with dietitians and physical therapists can provide patients with tailored advice that considers their thyroid condition.
Patient Education: Educating patients about the importance of adherence to both Semaglutide and their thyroid hormone replacement therapy is critical. Patients should understand how Semaglutide works, potential side effects, and the importance of regular monitoring of their thyroid function and overall health.
The administration of Semaglutide in patients with Hashimoto’s Thyroiditis requires a personalized approach that carefully considers the dosing, monitoring, and comprehensive management of both conditions. Through vigilant oversight and patient education, healthcare providers can harness the benefits of Semaglutide for weight loss and metabolic improvement while ensuring the stability of thyroid function and overall patient well-being.
Section 11: Conclusion
The exploration of Semaglutide’s role in managing Hashimoto’s Thyroiditis and its associated weight management challenges marks a significant step forward in the field of endocrinology and metabolic health. Through the detailed examination of Semaglutide’s mechanisms, safety profile, alternative therapies, and administration considerations, this discussion has illuminated the nuanced interplay between advanced diabetes and obesity pharmacotherapy and autoimmune thyroid disease management.
Semaglutide, as a GLP-1 receptor agonist, offers promising benefits for weight loss and glycemic control, aspects of health that are often compromised in individuals with Hashimoto’s Thyroiditis. Its ability to mimic the incretin effect, enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying, positions it as a valuable tool in the therapeutic arsenal against obesity and type 2 diabetes. However, the journey of integrating Semaglutide into the treatment regimen of those with Hashimoto’s requires careful navigation, balancing its metabolic benefits against the need to maintain stable thyroid function.
The discussion highlighted the importance of vigilant monitoring of thyroid function tests, the adjustment of thyroid hormone replacement therapy, and the management of potential side effects. It also underscored the necessity of a holistic treatment approach, incorporating lifestyle modifications, dietary adjustments, and, when appropriate, alternative medications or interventions for weight management. This multifaceted strategy emphasizes the personalized nature of treating individuals with Hashimoto’s, acknowledging the diversity of responses to Semaglutide and the complexity of autoimmune thyroid conditions.
Looking forward, the intersection of Semaglutide therapy with Hashimoto’s Thyroiditis presents fertile ground for further research. Clinical trials and longitudinal studies focusing on this specific patient population are essential to deepen our understanding of Semaglutide’s long-term effects, optimal dosing strategies, and its place within the broader context of thyroid disease management. Such investigations will undoubtedly enrich our knowledge, guiding more informed clinical decisions and fostering improved patient outcomes.
In conclusion, the potential of Semaglutide to significantly impact the lives of individuals with Hashimoto’s Thyroiditis is clear. Yet, it comes with the caveat of a need for meticulous, patient-centric care. As we advance, the collaboration between patients, endocrinologists, primary care providers, and allied health professionals will be crucial in harnessing the full potential of Semaglutide, ensuring that its benefits are realized safely and effectively for those navigating the complexities of Hashimoto’s Thyroiditis. Learn more about how our semaglutide program works!
Section 12: Research Citations
Semaglutide, a glucagon-like peptide-1 receptor agonist
(GLP-1 RA), has gained prominence as a treatment option for type 2 diabetes
mellitus (T2DM) due to its efficacy and cardiovascular benefits. However,
concerns have been raised regarding its potential association with Hashimoto’s
thyroiditis, an autoimmune thyroid disorder. This review aims to systematically
evaluate existing clinical evidence to elucidate the relationship between
semaglutide use and Hashimoto’s thyroiditis, providing insights into its clinical
implications.
- US
Food and Drug Administration (FDA). Highlights of prescribing information:
Rybelsus (semaglutide) tablets, for oral use. Accessed January 10, 2024.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf
- Marso
SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in
patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834-1844.
doi:10.1056/NEJMoa1607141
- Davies
MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2
diabetes, 2018. A consensus report by the American Diabetes Association
(ADA) and the European Association for the Study of Diabetes (EASD).
Diabetes Care. 2018;41(12):2669-2701. doi:10.2337/dci18-0033
- Rodbard
HW, Rosenstock J, Canani LH, et al. Oral semaglutide versus empagliflozin
in patients with type 2 diabetes uncontrolled on metformin: The PIONEER 2
trial. Diabetes Care. 2019;42(12):2272-2281. doi:10.2337/dc19-0883
- Ahmann
AJ, Capehorn M, Charpentier G, et al. Efficacy and safety of once-weekly
semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN
3): a 56-week, open-label, randomized clinical trial. Diabetes Care.
2018;41(2):258-266. doi:10.2337/dc17-1200
- Pratley
RE, Aroda VR, Lingvay I, et al. Semaglutide versus dulaglutide once weekly
in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label,
phase 3b trial. Lancet Diabetes Endocrinol. 2018;6(4):275-286.
doi:10.1016/S2213-8587(18)30024-X
- Aroda
VR, Bain SC, Cariou B, et al. Efficacy and safety of once-weekly
semaglutide versus once-daily insulin glargine as add-on to metformin
(with or without sulfonylureas) in insulin-naive patients with type 2
diabetes (SUSTAIN 4): a randomised, open-label, parallel-group,
multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol.
2017;5(5):355-366. doi:10.1016/S2213-8587(17)30092-4
- Buse
JB, Wexler DJ, Tsapas A, et al. 2019 update to: Management of
hyperglycemia in type 2 diabetes, 2018. A consensus report by the American
Diabetes Association (ADA) and the European Association for the Study of
Diabetes (EASD). Diabetes Care. 2020;43(2):487-493. doi:10.2337/dci19-0066
- Davies
MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2
diabetes, 2018. A consensus report by the American Diabetes Association
(ADA) and the European Association for the Study of Diabetes (EASD).
Diabetes Care. 2018;41(12):2669-2701. doi:10.2337/dci18-0033
- Novo
Nordisk. Data on file. Semaglutide product development, clinical trial
results, and regulatory submissions.
These references provide a comprehensive overview of
semaglutide use in managing type 2 diabetes mellitus, with a focus on potential
associations with Hashimoto’s thyroiditis, aiding healthcare providers in
assessing its safety profile in patients with autoimmune thyroid disorders.
Questions and Answers: Semaglutide and Hashimoto
The timeline for Semaglutide’s effects on weight loss can vary among individuals, especially in those with Hashimoto’s Thyroiditis, where metabolic rates may be impacted by thyroid hormone levels. Generally, patients might start noticing weight loss within a few weeks of initiating Semaglutide, with significant results becoming more apparent over 2-6 months. It’s important to note that weight loss outcomes also depend on concurrent lifestyle interventions, such as diet and exercise, and the optimization of thyroid hormone replacement therapy.
Current research does not conclusively show that Semaglutide exacerbates autoimmune activity in Hashimoto’s Thyroiditis. However, given the autoimmune nature of Hashimoto’s, it’s crucial to monitor thyroid function and antibody levels closely when initiating or adjusting Semaglutide therapy. Ongoing studies aim to better understand the long-term implications of GLP-1 receptor agonists on autoimmune thyroid conditions.
Significant weight loss can alter the body’s requirement for thyroid hormone replacement. As patients lose weight with Semaglutide, healthcare providers should closely monitor thyroid function tests, particularly TSH and free T4 levels, to determine if adjustments in levothyroxine dosage are necessary. It’s a delicate balance to maintain optimal thyroid function, and regular follow-up is essential to ensure that patients remain euthyroid.
While Semaglutide aids in weight loss through its mechanisms, combining its use with specific dietary strategies can enhance effectiveness and support overall thyroid health. A diet rich in anti-inflammatory foods, selenium, and iodine (within recommended limits) can support thyroid function. Additionally, reducing processed foods, sugars, and excessive goitrogens (foods that can interfere with thyroid function) is advisable. Consulting with a dietitian familiar with Hashimoto’s can provide personalized dietary guidance.
Patients should have regular check-ins with their healthcare provider to monitor thyroid function, weight loss progress, and any side effects from Semaglutide, such as gastrointestinal discomfort. Keeping a symptom diary can be helpful for tracking changes and discussing them during medical appointments. Managing side effects often involves dietary adjustments, hydration, and possibly altering the Semaglutide dosage under medical guidance.
The long-term outlook for patients with Hashimoto’s using Semaglutide is generally positive, especially when the medication is part of a comprehensive treatment plan that includes lifestyle changes and optimized thyroid hormone therapy. Continuous monitoring and adjustments by healthcare providers ensure that patients maintain thyroid health while achieving their weight management goals.
Semaglutide has been shown to improve insulin sensitivity in patients by enhancing the body’s response to insulin, which can be particularly beneficial for those with Hashimoto’s Thyroiditis, who often experience metabolic challenges, including insulin resistance, especially if they are overweight or have obesity. By promoting weight loss and directly affecting insulin secretion and action, Semaglutide can contribute to improved insulin sensitivity. However, it’s important for patients to work closely with their healthcare providers to monitor these effects, as adjustments in medication for diabetes or prediabetes may be necessary.
Semaglutide primarily affects glucose metabolism and appetite regulation, but it can also impact gastric emptying, which could influence the absorption and efficacy of other medications. For patients with Hashimoto’s Thyroiditis, the most critical interaction to consider is with levothyroxine, the standard therapy for hypothyroidism. Since Semaglutide can slow gastric emptying, it may affect how well levothyroxine is absorbed. Patients are often advised to take levothyroxine on an empty stomach, well before eating, to ensure optimal absorption. Regular monitoring and potentially adjusting the timing of levothyroxine intake may be necessary when using Semaglutide.
When prescribing Semaglutide to patients with Hashimoto’s Thyroiditis, it’s essential to consider individual factors, including age and gender, which can influence treatment outcomes. For instance, postmenopausal women and older adults might experience different metabolic effects and may have varying degrees of sensitivity to Semaglutide’s actions. Additionally, considerations around potential pregnancy must be addressed for women of childbearing age, as thyroid function plays a crucial role in fertility and pregnancy outcomes. A personalized approach, taking into account the patient’s age, gender, reproductive plans, and overall health status, is vital for optimizing treatment efficacy and safety.
For patients with Hashimoto’s Thyroiditis using Semaglutide, combining medication with specific lifestyle modifications can significantly enhance treatment outcomes. Key recommendations include:
• Dietary Adjustments: Adopting a nutrient-rich diet that supports thyroid health, focusing on whole foods, vegetables, fruits, lean proteins, and healthy fats. Limiting processed foods, sugars, and excessive iodine intake is also advised.
• Physical Activity: Engaging in regular, moderate exercise can help improve insulin sensitivity, cardiovascular health, and contribute to weight loss. Activities should be tailored to the individual’s fitness level and thyroid function status.
• Stress Management: Techniques such as meditation, yoga, or deep-breathing exercises can help manage stress, which is particularly important for individuals with autoimmune conditions.
• Adequate Sleep: Ensuring sufficient sleep supports hormonal balance, including thyroid hormones, and can improve the efficacy of weight loss efforts and overall well-being.