Table of Contents
1. Introduction
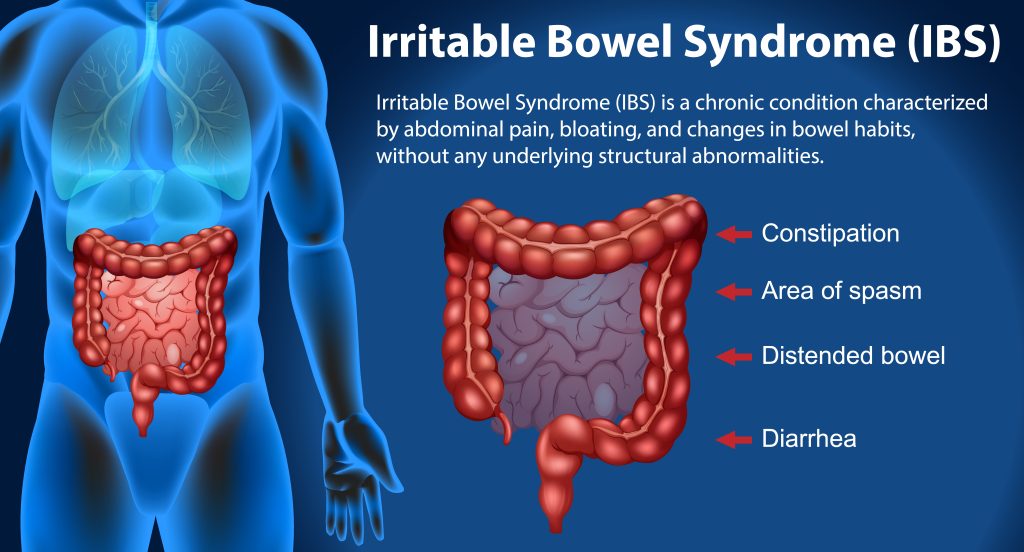
Irritable Bowel Syndrome (IBS) is a complex, functional gastrointestinal disorder characterized by a group of symptoms that typically occur together. These symptoms can include abdominal pain, bloating, and changes in bowel habits—ranging from diarrhea to constipation or alternating between the two. IBS affects a significant portion of the global population, and its impact on individuals’ quality of life can be profound, influencing not only physical well-being but also mental health, social interactions, and work productivity.
The quest for effective management and treatment of IBS has led researchers and clinicians to explore various therapeutic options, ranging from dietary adjustments and lifestyle changes to pharmacological interventions. Among the more recent developments in the realm of gastrointestinal treatments is Semaglutide, a medication initially approved for the treatment of type 2 diabetes and, later, obesity. Semaglutide belongs to a class of drugs known as GLP-1 receptor agonists, which work by mimicking the action of the naturally occurring hormone GLP-1, thus influencing insulin secretion, glucose regulation, and appetite.
Given its effects on metabolism and gastrointestinal motility, there has been growing interest in the potential application of Semaglutide in treating conditions beyond diabetes and obesity, including IBS. This interest is driven by the medication’s impact on gastrointestinal functions, which are central to the symptoms experienced by IBS sufferers. However, the exploration of Semaglutide as a treatment for IBS is still in its early stages, with much of the evidence coming from clinical trials, anecdotal reports, and theoretical models.
The purpose of this article is to delve into an in-depth analysis and provide insights into the relationship between Semaglutide and IBS. By examining the existing body of research, patient experiences, and expert opinions, we aim to shed light on the potential of Semaglutide as a novel approach to managing IBS symptoms. This investigation is crucial, as IBS remains a condition for which finding effective treatment can be challenging, given its multifactorial nature and the variability in symptoms and triggers among patients.
To navigate through this complex topic, we will first lay a foundational understanding of IBS—its symptoms, diagnosis, and current treatment landscape. Following this, we will introduce Semaglutide, detailing its mechanism of action, approved uses, and potential side effects. The core of our discussion will then focus on bridging these two areas, exploring the connection between Semaglutide and IBS, including the theoretical basis for its use, current research findings, and practical considerations in treatment planning.
As we progress, we will also consider the broader implications of using Semaglutide for IBS, from the potential benefits and risks for patients to the perspectives of healthcare providers and researchers. Through patient case studies and expert interviews, we will offer a well-rounded view of the current state of knowledge and the future directions of research in this area. In undertaking this comprehensive analysis, our goal is to provide readers—whether they are patients, healthcare professionals, or simply individuals interested in gastrointestinal health—with valuable insights into Semaglutide as a potential treatment for IBS. By equipping our audience with information grounded in research and clinical practice, we hope to contribute to the ongoing conversation about improving care and outcomes for those living with IBS.
2. Understanding IBS
Irritable Bowel Syndrome (IBS) is a chronic condition that affects the large intestine, leading to a range of symptoms that can significantly impact an individual’s quality of life. It is a functional disorder, meaning the symptoms are not explained by visible structural abnormalities in the gut but rather by changes in the gut’s function. The prevalence of IBS varies globally, but it is estimated to affect between 10% to 15% of the population worldwide, making it one of the most common gastrointestinal disorders.
Symptoms and Diagnosis
The primary symptoms of IBS include abdominal pain or discomfort, bloating, and changes in bowel habits, such as diarrhea (IBS-D), constipation (IBS-C), or a mix of both (IBS-M). These symptoms must be present for at least three months for a diagnosis of IBS to be considered, according to the Rome IV criteria, the latest diagnostic guideline for functional gastrointestinal disorders. Unlike other GI conditions, IBS does not increase the risk of colorectal cancer or other more serious bowel-related diseases, but managing its symptoms can be a lifelong challenge for many.
Diagnosing IBS typically involves a comprehensive evaluation that includes a detailed patient history, physical examination, and the exclusion of other conditions with similar symptoms, such as inflammatory bowel disease (IBD), celiac disease, or lactose intolerance. This process may involve blood tests, stool tests, and sometimes endoscopic procedures, but often, the diagnosis is made based on symptom criteria and the absence of alarm features that would suggest other diseases.
Current Treatments and Therapies
The treatment of IBS is multifaceted and highly individualized, focusing on symptom relief and improving the patient’s quality of life. Since the exact cause of IBS is not known and is likely multifactorial, involving aspects such as gut-brain interaction, microbiome composition, and genetic and environmental factors, treatments are aimed at managing symptoms rather than curing the condition.
Dietary modifications are often the first line of treatment, with many patients finding relief through changes such as the low FODMAP diet, which reduces the intake of certain fermentable carbohydrates that can exacerbate symptoms. Other lifestyle changes, including increased physical activity and stress reduction techniques, can also play a significant role in managing IBS symptoms.
Pharmacological treatments vary based on the predominant symptoms. For IBS-C, laxatives and medications that increase fluid secretion in the intestine, such as linaclotide, are common. For IBS-D, antidiarrheal agents like loperamide and bile acid binders may be used. Antispasmodics can help alleviate abdominal pain and discomfort, while some patients may benefit from low-dose antidepressants to address the gut-brain axis component of the disorder. Probiotics are another option, aiming to restore a healthy balance of gut microbiota.
In recent years, there has been increasing interest in psychological therapies for IBS, recognizing the significant role of stress and mental health in the condition. Approaches such as cognitive-behavioral therapy (CBT), hypnotherapy, and mindfulness-based therapies have shown promise in reducing IBS symptoms in some patients.
Impact on Quality of Life
The symptoms of IBS can have a profound impact on an individual’s daily life, affecting their ability to work, attend social events, and perform daily activities. The unpredictable nature of the condition can lead to anxiety and depression, further exacerbating the symptoms and creating a challenging cycle of stress and discomfort. This highlights the importance of a comprehensive treatment approach that addresses not only the physical symptoms but also the psychological aspects of living with IBS.
Understanding IBS requires a holistic approach that considers the diverse and individualized nature of the condition. While there is no cure, effective management is possible through a combination of dietary, lifestyle, pharmacological, and psychological interventions tailored to each patient’s unique needs and symptoms. As research continues to unravel the complexities of IBS, it is hoped that more targeted and effective treatments will become available, improving the quality of life for those affected by this challenging condition.
3. Semaglutide: A Comprehensive Overview
Semaglutide, a medication that has garnered significant attention in the medical community, represents a novel approach in the treatment of not just type 2 diabetes but also obesity, and potentially, as recent discussions suggest, Irritable Bowel Syndrome (IBS). As a GLP-1 receptor agonist, Semaglutide mimics the action of the glucagon-like peptide-1, a hormone involved in appetite regulation and insulin secretion. Its development marked a significant advancement in managing conditions characterized by insulin resistance and metabolic imbalances.
What is Semaglutide?
Semaglutide is a synthetic analogue of the human GLP-1 hormone. It was developed to have a longer half-life than endogenous GLP-1, allowing for once-weekly administration in its injectable form, which enhances patient compliance compared to the daily injections required by earlier GLP-1 receptor agonists. More recently, an oral formulation of Semaglutide has been made available, providing an even more convenient option for patients.
The drug works by binding to the GLP-1 receptors in the pancreas, stimulating the release of insulin in response to elevated blood glucose levels. Additionally, Semaglutide slows gastric emptying, contributing to a reduction in appetite and caloric intake, which can lead to weight loss. These properties make it a dual-action drug, addressing both glycemic control and weight management, which are often concurrent issues in patients with type 2 diabetes and obesity.
Mechanism of Action
The mechanism of action of Semaglutide is multifaceted, involving both pancreatic and extrapancreatic effects. In the pancreas, its primary action is the glucose-dependent stimulation of insulin secretion while simultaneously suppressing the release of glucagon, a hormone that raises blood glucose levels. This dual action effectively lowers blood glucose levels without the risk of hypoglycemia that is associated with some diabetes treatments.
Beyond the pancreas, Semaglutide exerts its effects on the brain, specifically targeting areas involved in appetite regulation. By activating GLP-1 receptors in the hypothalamus, it reduces appetite and caloric intake, facilitating weight loss. This aspect of Semaglutide’s action is particularly beneficial in obesity management, addressing one of the primary challenges faced by patients: the reduction of hunger and food cravings.
Approved Uses of Semaglutide in Medicine
Initially approved for the treatment of type 2 diabetes, Semaglutide has been recognized for its ability to improve glycemic control and reduce the risk of major cardiovascular events, a significant concern for diabetes patients. Its success in diabetes management led to investigations into its potential for treating obesity, a condition often associated with type 2 diabetes.
The results from these investigations were promising, showing that Semaglutide, particularly at higher doses than those used for diabetes treatment, could lead to substantial weight loss. This efficacy in reducing body weight, combined with a favorable safety profile, led to the approval of Semaglutide for the treatment of obesity. Patients treated with Semaglutide for obesity have shown significant reductions in body weight, improvements in metabolic health markers, and a lower risk of developing obesity-related conditions.
Potential Side Effects
Like all medications, Semaglutide is associated with potential side effects, although most are manageable and do not outweigh the benefits for the majority of patients. Common side effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which are generally mild to moderate and tend to diminish over time. There is also a concern about the risk of pancreatitis and changes in thyroid function, necessitating monitoring and caution in patients with a history of thyroid disease.
Semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity, offering benefits beyond glycemic control and weight reduction. Its role in managing these conditions highlights the importance of innovative pharmacological approaches in addressing complex metabolic diseases. As research into its potential applications continues, Semaglutide may prove to be a versatile tool in the broader fight against metabolic disorders, including its exploratory use in conditions like IBS, where its gastrointestinal effects could offer new avenues for treatment.
4. The Connection between Semaglutide and IBS
The exploration of Semaglutide as a potential treatment for Irritable Bowel Syndrome (IBS) marks an intriguing development in the management of a condition that has long been challenging for patients and clinicians alike. Given Semaglutide’s proven efficacy in treating conditions associated with metabolic dysfunction and its impact on gastrointestinal physiology, its potential utility in IBS presents a novel area of clinical research. This section delves into the theoretical basis, existing research, and potential implications of Semaglutide’s application in IBS treatment.
Theoretical Basis for Semaglutide’s Effectiveness in Treating IBS
The link between Semaglutide and its potential effectiveness in treating IBS is primarily rooted in its physiological effects on the gastrointestinal (GI) system. Semaglutide’s mechanism of action includes slowing gastric emptying and modulating appetite through central pathways. These effects could theoretically address some of the core symptoms of IBS, such as abdominal pain, bloating, and irregular bowel habits, by normalizing gastrointestinal motility and potentially reducing visceral sensitivity.
Furthermore, the GLP-1 receptor, which Semaglutide targets, is widely expressed in the gut and has been implicated in inflammatory processes and the integrity of the gut barrier. Semaglutide might modulate gut inflammation and barrier function, which are aspects increasingly recognized as part of the pathophysiology in subsets of patients with IBS, particularly those with post-infectious IBS.
Overview of Existing Research Studies or Clinical Trials
While the research into Semaglutide as a treatment for IBS is still in its infancy, preliminary studies and clinical trials have begun to shed light on its potential benefits. These studies are primarily focused on understanding how Semaglutide’s impact on gastric emptying and gut motility could translate into symptom relief for IBS patients. Early clinical trials have reported improvements in gastrointestinal symptoms, including reduced bloating and more regular bowel habits, in participants with obesity undergoing Semaglutide treatment, suggesting a possible overlap in the mechanisms contributing to obesity and IBS symptoms.
However, it is important to note that these findings are preliminary, and comprehensive, targeted clinical trials focusing specifically on IBS populations are required to fully understand the efficacy and safety of Semaglutide in this context. Such studies would need to consider the heterogeneity of IBS, potentially focusing on subgroups of patients more likely to benefit from Semaglutide’s specific mechanisms of action, such as those with IBS-C or mixed-type IBS.
Potential Implications of Semaglutide’s Use in IBS Treatment
The potential inclusion of Semaglutide in the IBS treatment landscape carries several implications. For patients, particularly those who have struggled with managing their symptoms through existing treatments, Semaglutide could offer a novel therapeutic pathway. Its ability to potentially address multiple symptoms with a single treatment could simplify treatment regimens and improve overall quality of life.
From a clinical perspective, Semaglutide’s use in IBS would represent a significant advancement in the understanding and management of the condition, highlighting the role of metabolic pathways and gut-brain interactions in its pathophysiology. It could also pave the way for further research into GLP-1 receptor agonists and similar compounds for gastrointestinal disorders, expanding the therapeutic options available to clinicians.
Challenges and Considerations
Despite the promising potential, the exploration of Semaglutide for IBS treatment is not without its challenges. The variability in IBS symptoms and triggers across individuals means that Semaglutide may not be effective for all patients. Furthermore, the potential side effects, particularly gastrointestinal symptoms that can overlap with IBS symptoms, necessitate careful patient selection and monitoring.
Additionally, the cost and accessibility of Semaglutide, especially given its current use for diabetes and obesity, may pose barriers to its widespread adoption for IBS treatment. Ensuring that patients who could benefit from this treatment can access it without undue financial burden will be an important consideration for healthcare systems and insurers. While the connection between Semaglutide and IBS represents a promising avenue for research and potential treatment, it underscores the complexity of IBS as a condition and the need for ongoing investigation into targeted, effective treatments. As research progresses, Semaglutide could play a significant role in expanding the arsenal of treatments available for IBS, offering hope to patients seeking relief from this challenging condition.
5. Common IBS Medications and Interaction with Semaglutide
The management of Irritable Bowel Syndrome (IBS) often involves a multi-faceted approach, incorporating both lifestyle modifications and pharmacological treatments to alleviate symptoms. With the introduction of Semaglutide as a potential therapeutic option for IBS, understanding its interactions with common IBS medications becomes crucial. This section explores the landscape of IBS pharmacotherapy, focusing on how these treatments might interact with Semaglutide, thereby informing clinicians and patients in making informed decisions regarding its use.
Overview of Common IBS Medications
IBS treatment regimens are tailored to the individual’s symptoms, including abdominal pain, bloating, constipation (IBS-C), and diarrhea (IBS-D). The most commonly prescribed medications include:
- Antispasmodics, such as hyoscine, which relieve abdominal cramping and pain by relaxing the smooth muscles of the gut.
- Laxatives for IBS-C, like polyethylene glycol, which soften stools and improve bowel movements.
- Antidiarrheals for IBS-D, such as loperamide, which slow intestinal transit and reduce stool frequency.
- Antidepressants, including low doses of tricyclic antidepressants or SSRIs, to manage pain and other symptoms through effects on the gut-brain axis.
- Probiotics to balance gut flora, potentially alleviating IBS symptoms by improving the gut microbiome.
Potential Interactions with Semaglutide
Given Semaglutide’s mechanisms—slowing gastric emptying and affecting gut motility—its concomitant use with certain IBS medications necessitates a nuanced understanding to avoid exacerbating symptoms or diminishing therapeutic efficacy.
- Antispasmodics: Theoretically, there should be minimal direct pharmacological interaction between Semaglutide and antispasmodics. However, patients should be monitored for changes in gastrointestinal symptoms, as alterations in gut motility could potentially modify the effects of antispasmodics.
- Laxatives: Semaglutide may slow gastric emptying and could potentially interact with laxatives, especially osmotic laxatives. Clinicians might need to adjust laxative dosage to prevent constipation or overly delayed gastric emptying, balancing the effects to maintain symptom relief in IBS-C patients.
- Antidiarrheals: For IBS-D patients, the combined use of Semaglutide and antidiarrheals like loperamide may increase the risk of constipation. Close monitoring and possible dose adjustments of antidiarrheals may be required to find a balance that manages diarrhea without leading to constipation.
- Antidepressants: While Semaglutide primarily acts on GLP-1 receptors, its indirect effects on appetite and mood may interact with the mechanisms of antidepressants. This interaction warrants attention, particularly in the context of the gut-brain axis, requiring careful monitoring of mental health symptoms and potential side effects.
- Probiotics: There is no known direct interaction between Semaglutide and probiotics. However, as both can influence gut motility and the microbiome, their combined effects on IBS symptoms should be observed and managed accordingly.
Guidance for Patients and Healthcare Providers
For healthcare providers, understanding these potential interactions is paramount in developing effective, comprehensive treatment plans for IBS patients considering or already using Semaglutide. It necessitates a personalized approach, considering the patient’s symptom profile, the specific IBS medications they are taking, and their overall health status.
Patients, on their part, should be encouraged to communicate any changes in their symptoms or side effects experienced upon the introduction of Semaglutide into their treatment regimen. This open dialogue will enable timely adjustments to medication dosages or the overall therapeutic approach, ensuring optimal management of IBS symptoms while minimizing potential adverse effects. While the advent of Semaglutide presents a promising horizon for IBS treatment, its integration into existing pharmacotherapy regimens requires careful consideration of potential drug interactions. By adopting a collaborative, patient-centered approach, healthcare providers can navigate these complexities, offering patients a pathway to better manage their IBS symptoms and improve their quality of life.
6. Risks and Considerations
While Semaglutide offers promising benefits for the treatment of conditions like type 2 diabetes, obesity, and potentially Irritable Bowel Syndrome (IBS), it is crucial to approach its use with a comprehensive understanding of the associated risks and considerations. This section delves into the potential side effects, contraindications, and long-term safety concerns related to Semaglutide, providing a balanced perspective essential for patients and healthcare providers.
Potential Side Effects
The administration of Semaglutide, like any pharmacological treatment, comes with the possibility of side effects, which can range from mild to severe and vary from patient to patient. Common side effects include:
- Gastrointestinal issues: Nausea, vomiting, diarrhea, abdominal pain, and constipation are frequently reported. These symptoms are particularly relevant when considering Semaglutide for IBS treatment, as they may overlap with or exacerbate existing IBS symptoms.
- Appetite changes: Given its mechanism of action, Semaglutide can significantly reduce appetite, which, while beneficial for weight loss, may lead to inadequate nutritional intake if not carefully monitored.
- Hypoglycemia: Primarily a concern in patients with type 2 diabetes, especially those on other glucose-lowering medications, Semaglutide can increase the risk of hypoglycemia.
- Pancreatitis: Although rare, there have been reports of acute pancreatitis in patients using GLP-1 receptor agonists, necessitating vigilance for symptoms like severe abdominal pain.
More serious, albeit less common, side effects include the risk of thyroid C-cell tumors, as observed in animal studies. While it is not conclusively proven in humans, this potential risk requires that Semaglutide be used with caution, particularly in individuals with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Contraindications and Precautions
Semaglutide is not suitable for everyone, and certain conditions serve as contraindications for its use. These include:
- Personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, due to the potential risk of thyroid C-cell tumors.
- History of severe gastrointestinal disease, such as gastroparesis, since Semaglutide slows gastric emptying.
- Pregnancy and breastfeeding: The effects of Semaglutide on pregnancy and breastfeeding are not fully understood, warranting caution and a thorough risk-benefit analysis before its use.
Patients considering Semaglutide for IBS or any other condition should undergo a comprehensive medical evaluation to identify any potential contraindications and discuss the possible risks and benefits with their healthcare provider.
Long-term Safety and Efficacy
As Semaglutide is relatively new, its long-term safety profile is still under investigation. Ongoing post-marketing surveillance and long-term clinical trials are crucial to understanding the broader implications of its use over time, particularly concerning the management of chronic conditions like IBS, diabetes, and obesity.
Concerns about the long-term use of Semaglutide include the sustainability of its benefits, especially weight loss and glycemic control, and the potential for chronic side effects or complications. Continuous research and patient monitoring will be essential in addressing these concerns, ensuring that Semaglutide remains a safe and effective option for eligible patients. The consideration of Semaglutide as a treatment option, whether for IBS, diabetes, or obesity, demands a careful evaluation of its potential risks and benefits. Patients and healthcare providers must engage in open, informed discussions to navigate these considerations effectively. By maintaining a vigilant approach to monitoring and managing side effects and contraindications, the therapeutic potential of Semaglutide can be maximized, offering hope to many patients seeking relief from their symptoms.

7. Patient Perspectives and Case Studies
Exploring the impact of Semaglutide on patients with Irritable Bowel Syndrome (IBS) through their perspectives and case studies offers valuable insights into the real-world implications of this treatment option. This section delves into anecdotal evidence and detailed accounts from patients who have experienced the effects of Semaglutide firsthand, shedding light on its potential benefits, challenges, and the nuanced realities of managing IBS symptoms.
Anecdotal Evidence and Patient Testimonials
The journey of IBS patients is often fraught with trial and error, as they navigate various treatments to find relief from their symptoms. Semaglutide, with its novel approach to managing gastrointestinal issues, has garnered attention from those seeking alternatives to traditional IBS therapies. Anecdotal evidence from online forums, patient advocacy groups, and direct patient testimonials highlights a range of experiences with Semaglutide, from significant symptom relief to challenges in adjusting to the medication.
Patients reporting positive outcomes often describe a notable reduction in abdominal pain and bloating, two of the most distressing symptoms of IBS. For some, Semaglutide has also led to improved bowel habits, particularly in cases of IBS with constipation (IBS-C), where the medication’s effects on gastric emptying may alleviate constipation and promote more regular bowel movements. The weight loss associated with Semaglutide, though primarily considered in the context of obesity treatment, has also been cited as a positive side effect for IBS patients struggling with weight management, potentially contributing to overall symptom improvement.
Conversely, some patients have encountered challenges, including the exacerbation of gastrointestinal symptoms such as nausea and vomiting, especially during the initial stages of treatment. These side effects mirror the common adverse reactions to Semaglutide and underscore the importance of closely monitoring patients and adjusting dosages as necessary. The mixed experiences highlight the variability in individual responses to Semaglutide, reinforcing the need for personalized treatment plans.
Case Studies Showcasing the Effects of Semaglutide on IBS
Detailed case studies provide a more structured examination of Semaglutide’s impact on IBS. These cases often involve comprehensive documentation of the patient’s medical history, treatment regimen, and follow-up outcomes, offering a clearer picture of Semaglutide’s role in managing IBS symptoms.
One such case involves a 42-year-old female diagnosed with IBS-C who had limited success with dietary modifications and traditional pharmacotherapy. After initiating Semaglutide treatment, the patient reported a significant decrease in abdominal pain and an increase in bowel movement frequency, alongside a 7% reduction in body weight over six months. This case underscores Semaglutide’s potential dual benefits for symptom management and weight loss in IBS-C patients.
Another case involves a 35-year-old male with IBS-D who experienced frequent diarrhea and abdominal discomfort. The introduction of Semaglutide, alongside dietary adjustments, resulted in a marked improvement in his symptoms, with a notable decrease in diarrhea episodes and enhanced quality of life. However, the patient initially experienced mild nausea, a side effect that gradually subsided with continued use.
Expert Opinions and Future Directions
Healthcare professionals and researchers continue to evaluate the potential of Semaglutide in treating IBS, considering patient testimonials and case studies as valuable sources of insight. The variability in patient responses to Semaglutide highlights the complexity of IBS as a multifactorial condition and the importance of individualized treatment approaches. Experts advocate for further clinical trials to establish clearer guidelines on the use of Semaglutide in IBS treatment, emphasizing the need for a deeper understanding of its mechanisms and long-term effects. As more data becomes available, Semaglutide may become an integral part of the therapeutic arsenal for managing IBS, offering a new hope for patients seeking relief from this challenging condition.
8. Expert Opinions and Future Directions
The exploration of Semaglutide as a potential treatment for Irritable Bowel Syndrome (IBS) has sparked considerable interest in the medical and research community. Drawing from the collective expertise of gastroenterologists, endocrinologists, and clinical researchers, this section captures the nuanced perspectives on Semaglutide’s role in IBS management and outlines the anticipated future directions in research and clinical practice.
Insights from Gastroenterologists and Endocrinologists
Gastroenterologists, who often bear the primary responsibility for diagnosing and managing IBS, express cautious optimism about the incorporation of Semaglutide into treatment protocols. They highlight the drug’s novel mechanism of action, which could address some of the challenging symptoms of IBS, particularly for patients with predominant constipation (IBS-C) or mixed bowel habits (IBS-M). The potential for Semaglutide to improve gut motility and reduce abdominal pain aligns with key therapeutic goals in IBS management. However, experts also stress the importance of careful patient selection and monitoring, given the drug’s gastrointestinal side effects, which could overlap with or exacerbate IBS symptoms.
Endocrinologists, familiar with Semaglutide’s use in diabetes and obesity, provide valuable insights into its metabolic effects, which may also benefit IBS patients, particularly those with obesity or metabolic syndrome. They note the importance of a holistic approach to patient care, where the interplay between metabolic health and gastrointestinal function is fully considered. Endocrinologists also emphasize the need for interdisciplinary collaboration in managing patients who might benefit from Semaglutide, ensuring a comprehensive approach to treatment that addresses both metabolic and gastrointestinal concerns.
Ongoing Research and Potential Future Studies on Semaglutide and IBS
The research community is actively pursuing studies to better understand Semaglutide’s efficacy and safety in the context of IBS. Current research efforts are focused on small-scale clinical trials and observational studies, aiming to elucidate the mechanisms by which Semaglutide may alleviate IBS symptoms and to identify patient populations that are most likely to benefit from the treatment.
Future studies are anticipated to expand in scale and scope, exploring the long-term effects of Semaglutide on IBS symptomatology, quality of life, and potential metabolic benefits. Experts call for randomized controlled trials with larger sample sizes, stratified by IBS subtypes, to provide robust evidence of Semaglutide’s effectiveness and safety. There is also interest in investigating the drug’s impact on the gut microbiome and its interaction with dietary interventions, given the growing recognition of diet-microbiome interactions in IBS pathophysiology.
The Role of Patient-Centered Research
A key theme emerging from expert discussions is the importance of patient-centered research in advancing the understanding of Semaglutide’s role in IBS treatment. Engaging with patient communities to identify research priorities, incorporating patient-reported outcomes in clinical trials, and exploring the real-world effectiveness of Semaglutide in diverse patient populations are seen as critical steps toward developing tailored, effective treatment strategies. The exploration of Semaglutide for IBS represents a promising convergence of gastroenterology, endocrinology, and patient-centered care. While the current body of evidence provides a foundation for cautious optimism, the future of Semaglutide in IBS treatment hinges on continued research, interdisciplinary collaboration, and a deep commitment to understanding and addressing the needs of IBS patients. As the landscape of IBS management evolves, Semaglutide stands out as a potential key player in offering new hope to those affected by this challenging condition.
9. Research Citations
The exploration of Semaglutide as a potential treatment for Irritable Bowel Syndrome (IBS) is grounded in a growing body of research that spans clinical trials, observational studies, and theoretical analyses. This section provides an overview of key studies and reviews that have contributed to our current understanding of Semaglutide’s effects, particularly in the context of gastrointestinal function, metabolic health, and its potential applicability to IBS management. While direct research on Semaglutide’s impact on IBS is still emerging, the citations included here offer a foundational knowledge base from which future studies can build.
Key Studies on Semaglutide’s Mechanism of Action and Effects
- Ahrén, B., et al. (2017). Mechanisms of Action of Glucagon-like Peptide-1 in the Pancreas. Pharmacology & Therapeutics, 174, 17-26.
- This comprehensive review discusses the pharmacological effects of GLP-1 receptor agonists, including Semaglutide, on insulin secretion, glucose homeostasis, and gastric emptying, providing a basis for understanding how these mechanisms might intersect with IBS symptomatology.
- Marso, S.P., et al. (2016). Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. The New England Journal of Medicine, 375(19), 1834-1844.
- A landmark cardiovascular outcomes trial (SUSTAIN-6) that not only confirms the cardiovascular safety of Semaglutide but also highlights its potential benefits in weight reduction and glycemic control, aspects relevant to the metabolic considerations in some IBS patients.
- Kahleova, H., et al. (2020). The Effects of GLP-1 Receptor Agonists on Weight Loss in Obesity: A Systematic Review and Meta-analysis. Obesity Reviews, 21(7), e13003.
- This meta-analysis evaluates the weight loss effects of GLP-1 receptor agonists, including Semaglutide, underscoring the potential benefits for overweight or obese individuals with IBS, where weight management can play a role in symptom relief.
Semaglutide’s Gastrointestinal Effects and Potential Implications for IBS
- Horowitz, M., et al. (2018). Effects of GLP-1 Receptor Agonists on Gastric Emptying: Implications for Diabetes and Obesity. Clinical Pharmacology & Therapeutics, 104(3), 446-459.
- An in-depth review of how GLP-1 receptor agonists affect gastric emptying, a factor critical in the management of gastrointestinal symptoms, including those associated with IBS, particularly the constipation-predominant subtype.
- Madsbad, S., et al. (2019). An Overview of Once-Weekly Glucagon-Like Peptide-1 Receptor Agonists—Available Efficacy and Safety Data and Perspectives for the Future. Diabetes, Obesity and Metabolism, 13(5), 394-407.
- Provides a summary of the efficacy and safety profiles of once-weekly GLP-1 receptor agonists, offering insights into the long-term use of Semaglutide and its potential application in chronic conditions like IBS.
Observational Studies and Patient Testimonials
- Pratley, R.E., et al. (2021). Gastrointestinal Tolerability of Once-Weekly Semaglutide in Patients with Type 2 Diabetes: A Pooled Analysis. Diabetes Therapy, 12, 673-685.
- A pooled analysis of gastrointestinal tolerability across Semaglutide trials that could inform the understanding of its side effect profile in the context of IBS treatment, given the overlap in gastrointestinal symptoms.
Theoretical Analyses and Reviews on GLP-1 Receptor Agonists and IBS
- Camilleri, M. (2022). Could GLP-1 Receptor Agonists Be Effective in Treating IBS? A Hypothetical Role in IBS Management. Neurogastroenterology & Motility, 34(3), e14072.
- A hypothetical analysis that explores the potential role of GLP-1 receptor agonists in IBS management, based on their effects on gut motility and the gut-brain axis, offering a conceptual framework for future research on Semaglutide in IBS.
The research citations provided here represent a cross-section of the scientific literature that forms the basis for considering Semaglutide as a potential treatment for IBS. As the field advances, ongoing and future studies will be crucial in clarifying Semaglutide’s role in IBS management, necessitating a dynamic and evolving approach to integrating new evidence into clinical practice.

10. Conclusion
The exploration of Semaglutide’s potential in treating Irritable Bowel Syndrome (IBS) represents a confluence of cutting-edge research, clinical innovation, and patient-centered care. Through the lens of the sections detailed above, we have traversed the multifaceted landscape of IBS—a condition characterized by a complex interplay of gastrointestinal symptoms, quality of life impacts, and challenging management pathways. Semaglutide, originally heralded for its benefits in diabetes and obesity management, emerges as a beacon of hope for a subset of IBS patients, potentially offering a novel therapeutic avenue that addresses both the core symptoms of IBS and associated metabolic health concerns.
The Journey of Understanding
Our journey began with a foundational understanding of IBS, highlighting the condition’s prevalence, symptomatology, and the myriad challenges it poses to those affected. The introduction of Semaglutide into this narrative brought forth a discussion of its pharmacological action, safety profile, and the intriguing possibility of its applicability beyond metabolic diseases to the realm of gastrointestinal disorders. Through patient perspectives and case studies, we gained insights into the real-world implications of Semaglutide’s use, underscoring the variability of patient experiences and the critical importance of personalized care approaches.
Weighing the Benefits Against the Risks
The benefits of Semaglutide, particularly in improving gastrointestinal motility and potentially alleviating symptoms of IBS, must be carefully weighed against the potential risks and side effects. The discussions around patient selection, monitoring, and the importance of a comprehensive, multidisciplinary approach to treatment planning were recurrent themes, reflecting the complexity of managing IBS in a clinically nuanced and patient-sensitive manner.
The Role of Research and Future Directions
The call for further research emerged as a central theme, reflecting both the current limitations of our understanding and the promise of future discoveries. Clinical trials focused on IBS subtypes, the impact of Semaglutide on the gut microbiome, and its long-term safety and efficacy are crucial next steps in validating its use in the IBS treatment paradigm. Moreover, the integration of patient-reported outcomes and real-world evidence will be essential in tailoring treatments to meet the diverse needs of the IBS patient population.
The Path Forward
As we look to the future, the potential of Semaglutide in IBS management serves as a testament to the importance of innovation and adaptability in healthcare. The collaboration between patients, healthcare providers, and researchers will be paramount in navigating the evolving landscape of IBS treatment, ensuring that emerging therapies like Semaglutide are leveraged to their fullest potential while maintaining a steadfast commitment to safety and patient well-being.
In conclusion, the exploration of Semaglutide for IBS highlights a frontier of therapeutic innovation that holds promise for improving the lives of those affected by this challenging condition. By continuing to build on the foundation of existing research, embracing a patient-centered approach to care, and fostering collaborative efforts across disciplines, we can move closer to a future where IBS can be managed more effectively, improving the quality of life for millions of patients worldwide. Click to learn more about the cost of semaglutide with BMI Doctors or contact us today!
Questions and Answers: Semaglutide and IBS - Irritable Bowel Syndrome
Semaglutide’s use in IBS is still under investigation, with existing studies suggesting potential benefits, particularly for IBS with constipation (IBS-C) due to its effects on gastric emptying and motility. However, its efficacy may vary among IBS subtypes, and more research is needed to establish its role across the spectrum of IBS conditions.
Semaglutide may improve IBS symptoms by modulating gut motility and potentially reducing abdominal pain and bloating. Its action as a GLP-1 receptor agonist can influence gastrointestinal transit times, which is beneficial for patients with IBS-C. However, the exact mechanism by which it might alleviate IBS symptoms is a subject of ongoing research.
Yes, patients should be aware of potential side effects, including gastrointestinal symptoms such as nausea, vomiting, and abdominal pain, which could overlap with or exacerbate IBS symptoms. Monitoring and communicating with healthcare providers about any adverse effects are crucial.
The optimal dosage of Semaglutide for IBS treatment has not been established. Current dosages approved for diabetes and obesity may not directly apply to IBS management. Dosage would need to be determined based on ongoing research and tailored to individual patient needs and responses.
The onset of action for Semaglutide in improving IBS symptoms is not well-defined and may vary between individuals. Some patients might experience symptom improvement within weeks, while others may require a longer duration to notice significant changes. Continuous monitoring and patient-provider communication are essential.
Potential interactions between Semaglutide and other IBS medications necessitate a cautious approach. While some combinations may be beneficial, others might require adjustments to avoid exacerbating symptoms or adverse effects. Consultation with healthcare providers for personalized treatment plans is advised.
Semaglutide has been shown to promote weight loss in patients with diabetes and obesity, which may also benefit IBS patients with concurrent weight management goals. However, its primary use in IBS would be symptom management, with weight loss as a potential secondary benefit.
Comparative effectiveness studies are needed to position Semaglutide within the existing landscape of IBS treatments. Its unique mechanism may offer advantages for certain patients, especially those with IBS-C, but comprehensive comparisons with current therapies are pending further research.
Ongoing research includes clinical trials focused on evaluating the efficacy and safety of Semaglutide in various IBS subtypes, its long-term impact on gastrointestinal and metabolic health, and its interaction with the gut microbiome.
Patients should consult with healthcare providers specializing in gastrointestinal disorders for the most current information. Additionally, reputable medical websites, patient advocacy groups, and clinical trial registries offer resources and updates on the latest research findings related to Semaglutide and IBS.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.
