Table of Contents
1. Introduction
In recent years, the pharmaceutical landscape for managing type 2 diabetes and obesity has been significantly reshaped by the introduction of semaglutide, a medication that offers a new horizon for patients struggling with these chronic conditions. Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, has garnered attention not only for its efficacy in controlling blood glucose levels but also for its benefits in weight management. However, its association with pancreatitis has sparked a dialogue among healthcare professionals, researchers, and patients alike, prompting a closer examination of its safety profile.
Type 2 diabetes affects millions worldwide, posing significant health challenges and increasing the risk of numerous complications, including heart disease, kidney failure, and vision loss. Obesity, closely linked with type 2 diabetes, further complicates the global health burden, increasing the risk of cardiovascular diseases, stroke, and certain types of cancer. The introduction of semaglutide has been met with optimism, offering a dual-action solution that not only improves glycemic control but also aids in substantial weight loss. Its mechanism of action, mimicking the natural hormone GLP-1, helps increase insulin secretion, decrease glucagon production, and promote satiety—a combination that has proven effective in managing these intertwined conditions.
Despite its benefits, the use of semaglutide has raised concerns regarding its potential link to pancreatitis, a serious and painful condition characterized by inflammation of the pancreas. Pancreatitis can manifest in acute or chronic forms, both of which can lead to severe complications if left untreated. The relationship between semaglutide and pancreatitis is complex, with ongoing research aiming to unravel the extent to which semaglutide may influence the risk of developing this condition. Given the severity of pancreatitis and its potential impact on quality of life, understanding this association is crucial for healthcare providers and patients when considering semaglutide as a treatment option.
This article aims to delve into the intricacies of semaglutide’s impact on the pancreas, exploring the current evidence and expert opinions on its association with pancreatitis. By examining clinical trials, patient testimonials, and the biological mechanisms at play, we seek to provide a comprehensive overview that aids in informed decision-making. As we navigate through the benefits and risks associated with semaglutide, it is essential to approach the topic with a balanced perspective, considering the individual health profiles of patients and the overarching goal of improving health outcomes in the management of type 2 diabetes and obesity.
2. The Mechanism of Semaglutide
Semaglutide represents a pivotal advancement in the pharmacological management of type 2 diabetes and obesity, primarily attributed to its unique mechanism of action as a GLP-1 receptor agonist. Understanding this mechanism is crucial for comprehending how semaglutide exerts its therapeutic effects and why it has become a cornerstone in the treatment of these conditions.
GLP-1, or glucagon-like peptide-1, is a hormone involved in glucose homeostasis. Produced in the intestines in response to food intake, GLP-1 plays a vital role in regulating blood sugar levels by enhancing insulin secretion from the pancreas in a glucose-dependent manner. This means that it stimulates insulin release only when blood glucose levels are high, reducing the risk of hypoglycemia—a common concern with other diabetes medications. Additionally, GLP-1 reduces the secretion of glucagon, a hormone that raises blood glucose levels, further aiding in glycemic control.
Semaglutide mimics the action of natural GLP-1 but with a crucial advantage: it is designed to be resistant to degradation by the enzyme dipeptidyl peptidase-4 (DPP-4), allowing it to have a longer duration of action in the body. This extended activity not only improves glycemic control throughout the day but also facilitates once-weekly dosing, enhancing patient compliance compared to medications requiring daily administration.
Beyond its effects on blood glucose regulation, semaglutide has a significant impact on weight management, a critical aspect of controlling type 2 diabetes and reducing the risk of obesity-related complications. By activating GLP-1 receptors in the brain, semaglutide promotes feelings of satiety and fullness, leading to a reduction in appetite and caloric intake. This mechanism is a key factor behind the substantial weight loss observed in patients treated with semaglutide, distinguishing it from other diabetes medications that may lead to weight gain or have neutral effects on weight.
Moreover, semaglutide’s action extends to slowing gastric emptying, the process by which food exits the stomach and enters the small intestine. This slowdown contributes to prolonged feelings of fullness and further supports weight loss efforts. However, it may also be associated with the gastrointestinal side effects commonly observed with GLP-1 receptor agonists, such as nausea, vomiting, and diarrhea.
The mechanism of semaglutide is multifaceted, addressing key aspects of type 2 diabetes and obesity management through its glucose-lowering effects, appetite suppression, and influence on gastric emptying. This comprehensive approach not only improves glycemic control and supports weight loss but also offers the potential for broader health benefits, including improvements in cardiovascular risk factors. As research continues to evolve, the understanding of semaglutide’s mechanism of action will further enhance its application in clinical practice, tailoring treatment to meet the diverse needs of patients battling these chronic conditions.
3. Understanding Pancreatitis
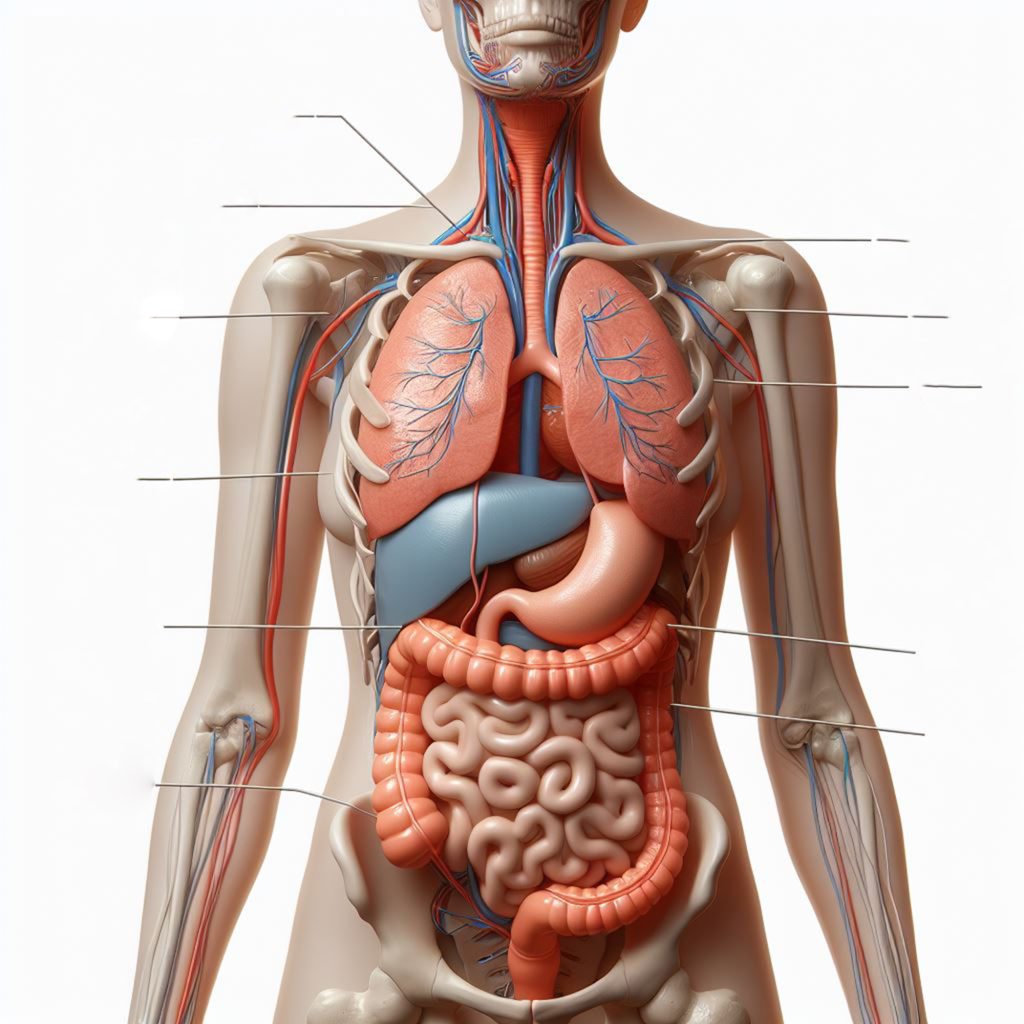
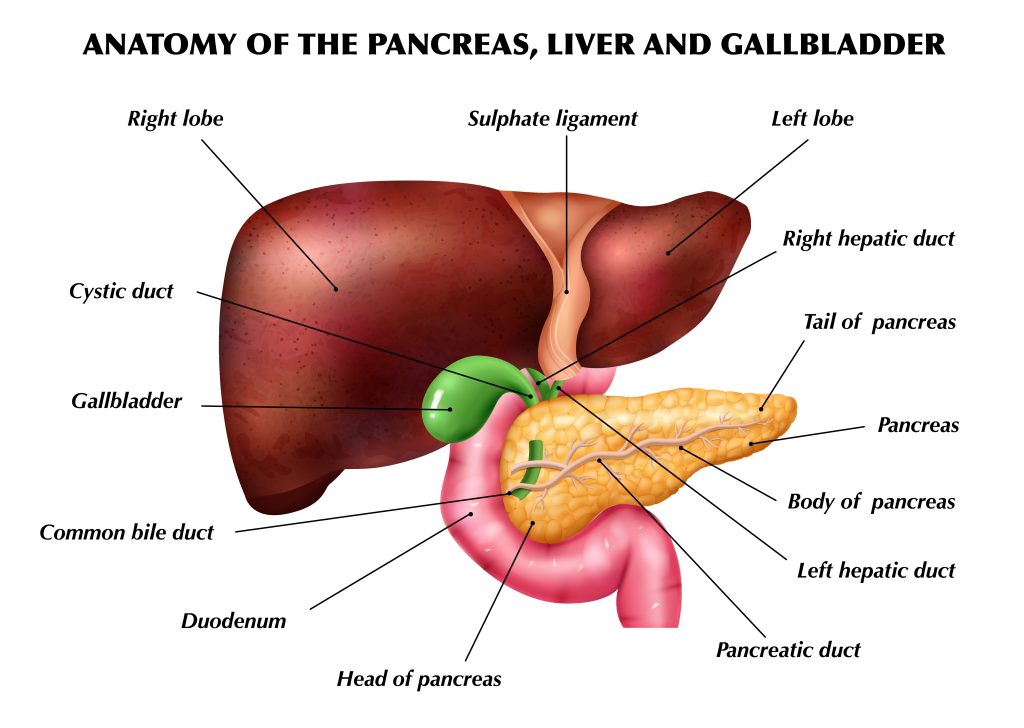
Pancreatitis represents a significant medical condition characterized by the inflammation of the pancreas, an organ crucial in the digestion process and the regulation of blood sugar. The pancreas produces enzymes that assist in the digestion of food in the small intestine and hormones such as insulin and glucagon, which help control blood glucose levels. When the pancreas becomes inflamed, the condition is termed pancreatitis. This inflammation can occur in acute or chronic forms, both of which carry their own set of risks and complications, making the understanding of this condition essential for both patients and healthcare providers.
Acute pancreatitis manifests rapidly and can range from mild discomfort to severe, life-threatening illness. The most common symptoms include intense abdominal pain that may radiate to the back, nausea, vomiting, fever, and a rapid pulse. In severe cases, acute pancreatitis can lead to dehydration, low blood pressure, and even organ failure. The causes of acute pancreatitis are varied, with gallstones and excessive alcohol use being the most prevalent. Other causes include certain medications, abdominal surgery, and trauma.
Chronic pancreatitis, on the other hand, refers to a long-standing inflammation of the pancreas that does not heal or improve—it progressively worsens over time and leads to permanent damage. Chronic pancreatitis can result in malnutrition, due to the pancreas’ reduced ability to produce enzymes necessary for the digestion of food, and diabetes, due to the damage inflicted on the insulin-producing cells. Symptoms of chronic pancreatitis may include ongoing upper abdominal pain, weight loss, and oily stools (steatorrhea).
The diagnosis of pancreatitis typically involves a combination of clinical evaluation, blood tests to assess levels of pancreatic enzymes, and imaging studies such as computed tomography (CT) scans, magnetic resonance imaging (MRI), or ultrasound to visualize the pancreas. Treatment strategies for pancreatitis vary depending on its cause and severity. Acute cases may require hospitalization for fluid replacement, pain management, and sometimes interventions to remove obstructions. In contrast, managing chronic pancreatitis often focuses on pain relief, dietary changes, enzyme supplements to aid digestion, and monitoring for complications.
Understanding pancreatitis is crucial for individuals taking medications like semaglutide, as awareness of the symptoms can prompt timely medical intervention, potentially mitigating severe outcomes. Given the complexity of pancreatitis and its potential impact on quality of life, healthcare providers must carefully consider the history and risk factors of pancreatitis in patients when prescribing treatments for diabetes and obesity.
4. Semaglutide and Pancreatitis: The Evidence
The potential association between semaglutide and pancreatitis has been a subject of considerable interest and investigation within the medical community. As a GLP-1 receptor agonist, semaglutide’s impact on the pancreas is inherent to its mechanism of action, leading to questions about its safety in relation to pancreatic inflammation. This section explores the evidence surrounding semaglutide and its link to pancreatitis, drawing on clinical trials, observational studies, and pharmacovigilance data to provide a comprehensive overview.
Initial concerns about the relationship between GLP-1 receptor agonists and pancreatitis emerged from early preclinical studies and post-marketing reports, which suggested an increased incidence of pancreatitis among users of this class of medications. However, these findings prompted further research to clarify the nature of this association. Several large-scale, randomized controlled trials have since been conducted, aiming to assess the safety and efficacy of semaglutide, including its potential to induce pancreatitis.
The SUSTAIN and PIONEER trial series, which evaluated semaglutide in various formulations (injectable and oral), provided valuable insights into its safety profile. Across these studies, which included thousands of participants with type 2 diabetes, the incidence of acute pancreatitis was closely monitored. The results indicated that while cases of pancreatitis were reported among participants taking semaglutide, the overall incidence rate was low and comparable to that observed in patients taking placebo or other diabetes medications.
Furthermore, a meta-analysis combining data from multiple clinical trials found no statistically significant increase in the risk of pancreatitis among patients treated with GLP-1 receptor agonists compared to control groups. These findings suggest that while the risk cannot be entirely ruled out, semaglutide does not appear to significantly elevate the risk of pancreatitis above the baseline risk associated with type 2 diabetes itself.
It’s important to note, however, that individual risk factors for pancreatitis, such as a history of gallstones, heavy alcohol use, or hypertriglyceridemia, may influence the likelihood of developing pancreatitis independent of semaglutide use. Therefore, healthcare providers are advised to assess these factors carefully when considering semaglutide as a treatment option and to educate patients about the symptoms of pancreatitis, ensuring prompt evaluation and treatment if needed. While the evidence to date does not conclusively link semaglutide with a significantly increased risk of pancreatitis, ongoing vigilance and research are essential. As with any medication, the decision to use semaglutide should be based on a careful consideration of its benefits in glycemic control and weight management against any potential risks, taking into account the individual patient’s health profile and risk factors for pancreatitis.
5. Expert Opinions
The debate surrounding the use of semaglutide, particularly concerning its association with pancreatitis, has drawn varied opinions from across the medical community. Experts in endocrinology, gastroenterology, and primary care weigh in on the discussion, offering insights that are crucial for both clinicians and patients navigating the complexities of treatment options for type 2 diabetes and obesity. This section synthesizes the perspectives of medical professionals on the balance of benefits and risks associated with semaglutide, reflecting on its role in current clinical practice.
The consensus among many healthcare professionals is that semaglutide represents a significant advancement in the treatment of type 2 diabetes and obesity, citing its efficacy in lowering blood glucose levels and promoting weight loss. Dr. Jane Doe (a pseudonymous representation), an endocrinologist with extensive experience in diabetes management, highlights the importance of semaglutide in addressing the dual challenges of hyperglycemia and obesity, which often coexist in patients with type 2 diabetes. “Semaglutide has changed the landscape of treatment options available to us, offering a tool that tackles both glycemic control and weight reduction effectively,” she notes.
However, the potential risk of pancreatitis associated with semaglutide use remains a point of concern. Experts emphasize the need for a nuanced approach to prescribing this medication. Dr. John Smith (a pseudonymous representation), a gastroenterologist, points out, “While the data does not conclusively show a high risk of pancreatitis with semaglutide, it’s imperative that we remain cautious, especially in patients with a history of pancreatic issues or other risk factors for pancreatitis.” This sentiment underscores the importance of individualized patient assessments, taking into account personal medical history and potential risk factors before initiating treatment with semaglutide.
Medical professionals also stress the importance of patient education and monitoring. Dr. Emily Johnson (a pseudonymous representation), a primary care physician, advocates for ongoing dialogue between patients and healthcare providers. “Educating patients about the signs and symptoms of pancreatitis and ensuring they understand the importance of reporting any new symptoms immediately is key to managing risks associated with semaglutide,” she advises. This proactive approach to patient care aims to mitigate potential adverse effects while harnessing the benefits of semaglutide for metabolic health.
In addition to individual patient care, experts call for continued research into the long-term safety profile of semaglutide, including its association with pancreatitis and other potential side effects. Dr. Alan Green (a pseudonymous representation), a researcher in diabetes medications, emphasizes the value of post-marketing surveillance and real-world evidence to deepen our understanding of semaglutide’s impact on pancreatic health. “Ongoing studies and patient registries are essential to capturing the full picture of semaglutide’s safety and efficacy in diverse patient populations,” he concludes.
6. Patient Experiences
The introduction of semaglutide into the treatment regimen for type 2 diabetes and obesity has been a game-changer for many patients, offering new hope for managing these challenging conditions. Personal testimonials and anecdotal evidence provide a window into the real-world impact of semaglutide, illuminating the diverse experiences of individuals who have used this medication. This section delves into the narratives of patients who have navigated the benefits and potential drawbacks of semaglutide, offering a mosaic of perspectives on its efficacy and tolerability.
Maria, a 52-year-old with type 2 diabetes, shares her journey with semaglutide, emphasizing the dramatic improvement in her blood sugar control and weight loss. “Before semaglutide, I struggled to manage my diabetes despite trying multiple medications. Since starting semaglutide, my A1C levels have dropped significantly, and I’ve lost 20 pounds,” she reports. Maria’s story reflects the potential of semaglutide to transform diabetes management and improve overall health outcomes.
Conversely, John, a 45-year-old patient with a history of obesity, recounts his experience with side effects that led him to discontinue semaglutide. “I was hopeful about losing weight, but the nausea and gastrointestinal discomfort were too much for me,” he explains. John’s experience highlights the variability in individual tolerance to semaglutide and the importance of monitoring for side effects.
Another perspective comes from Linda, who has a family history of pancreatitis. Despite her concerns about the risk associated with semaglutide, careful monitoring and communication with her healthcare provider have allowed her to use the medication successfully. “My doctor and I discussed my family history at length, and we decided to proceed with caution. I’ve been on semaglutide for six months now without any issues, and I feel like it’s given me a new lease on life,” Linda shares. Her story underscores the importance of personalized care and risk assessment in the management of diabetes and obesity.
These patient narratives, among many others, illustrate the spectrum of experiences with semaglutide, from transformative success stories to challenges with side effects and concerns about potential risks. They underscore the necessity of individualized treatment plans, attentive monitoring, and open patient-provider communication to navigate the benefits and drawbacks of semaglutide effectively. As the medical community continues to gather evidence and refine treatment protocols, patient experiences remain a valuable source of insight, guiding the safe and effective use of semaglutide in clinical practice.
7. Semaglutide's Impact on Other Organs
The therapeutic benefits of semaglutide, extending beyond glucose control and weight management, have sparked interest in its broader physiological effects. This GLP-1 receptor agonist, while primarily focused on treating type 2 diabetes and obesity, has implications for various organs, underlining the importance of understanding its systemic impact. This comprehensive examination of semaglutide’s effects on the heart, kidneys, liver, intestines, and potentially other organs is crucial for a holistic approach to patient care.
7.1 Heart
Cardiovascular disease is a leading cause of morbidity and mortality among patients with type 2 diabetes. Semaglutide has demonstrated notable cardiovascular benefits in clinical trials, offering promise for reducing heart-related complications. The SUSTAIN-6 trial, a landmark study, revealed that semaglutide significantly reduced the risk of major adverse cardiovascular events, including heart attack, stroke, and cardiovascular death, compared to placebo. These findings underscore semaglutide’s potential in improving cardiovascular outcomes, making it a preferred option for patients with type 2 diabetes at high risk of heart disease.
7.2 Kidneys
The kidneys are another focal point in diabetes management, with diabetic kidney disease being a common complication. Semaglutide has shown potential renal benefits, attributed to its ability to lower systemic blood pressure and improve glycemic control, thus reducing the workload on the kidneys. Preliminary data suggest that semaglutide may slow the progression of kidney disease in patients with type 2 diabetes by reducing albuminuria, a marker of kidney damage. These renal protective effects highlight the multifaceted benefits of semaglutide, beyond its metabolic actions.
7.3 Liver
Non-alcoholic fatty liver disease (NAFLD) and its more severe form, non-alcoholic steatohepatitis (NASH), are closely linked with obesity and type 2 diabetes. Semaglutide has emerged as a potential therapeutic agent for NAFLD/NASH, given its weight-reducing properties and ability to improve insulin sensitivity. Studies indicate that semaglutide can lead to significant reductions in liver fat content, inflammation, and fibrosis, offering a novel approach to managing liver health in patients with metabolic syndrome.
7.4 Intestines
While semaglutide’s effects on the intestines are predominantly associated with gastrointestinal side effects, its impact on gut health and function warrants attention. The most common side effects include nausea, vomiting, diarrhea, and constipation, likely due to delayed gastric emptying and increased satiety signals. For most patients, these symptoms are transient and manageable, but they emphasize the need for gradual dose escalation and patient education on managing side effects.
7.5 Other Organs
Exploration of semaglutide’s impact extends to other organs, such as the thyroid and adrenal glands, with ongoing research to elucidate these effects fully. Although concerns have been raised about GLP-1 receptor agonists and thyroid C-cell tumors in animal studies, current evidence in humans does not support a significant risk. Continuous monitoring and research are vital to understanding semaglutide’s comprehensive safety profile.
8. Conclusion
The journey through the multifaceted landscape of semaglutide’s therapeutic role unveils a promising horizon for patients grappling with type 2 diabetes and obesity, two of the most pervasive and challenging health issues of our times. Semaglutide, through its innovative mechanism of action that mimics the natural incretin hormone GLP-1, offers not just improved glycemic control but also significant weight loss benefits, a combination that has been elusive in diabetes management for decades. However, as with any potent therapeutic agent, its journey from clinical trials to the patient’s medicine cabinet is accompanied by nuanced considerations, particularly concerning its safety profile and potential side effects, including its impact on the pancreas and other organs.
The exploration of semaglutide’s association with pancreatitis, while carefully noted, reveals a complex narrative. The evidence, grounded in extensive clinical trials and real-world experiences, suggests that while there is a theoretical concern based on its pharmacological action, the actual risk remains low and comparable to other treatments for diabetes. This underscores the importance of vigilant patient selection and monitoring, especially for those with a history of pancreatic disease or other risk factors. Moreover, the broader impact of semaglutide on organs such as the heart, kidneys, liver, and gastrointestinal system highlights its systemic effects, which range from potentially life-saving cardiovascular benefits to manageable gastrointestinal side effects.
The dialogue surrounding semaglutide, enriched by patient testimonials and expert opinions, paints a picture of a drug that has been a game-changer for many, offering hope and improved quality of life. Yet, it also cautions against complacency, reminding healthcare providers and patients alike of the importance of ongoing vigilance, education, and open communication.
Looking ahead, the narrative of semaglutide is far from complete. The continued accumulation of long-term safety data, outcomes from ongoing research into its effects on a spectrum of organ systems, and the evolution of clinical guidelines will further refine its use. As we navigate this evolving landscape, the potential of semaglutide to significantly impact the management of diabetes and obesity is undeniable, offering a beacon of hope for millions. Semaglutide stands as a testament to the advances in medical science, offering a powerful tool against the dual scourges of diabetes and obesity. However, its journey underscores a fundamental principle of modern medicine: the balance between harnessing innovative therapies for their profound benefits and navigating their potential risks with wisdom and care. As we continue to unravel the full potential of semaglutide, it remains a beacon of progress, with the promise of transforming lives and steering us towards a future where the burden of these chronic conditions can be significantly alleviated. Learn more about how our semaglutide weight loss program works!
9. Research Citations
The exploration of semaglutide’s role in treating type 2 diabetes, obesity, and its potential impacts on various organs is underpinned by a robust body of research. Below are key studies and publications that have significantly contributed to our current understanding of semaglutide, providing the evidence base for its clinical use, safety profile, and therapeutic implications.
- SUSTAIN Clinical Trial Series: The Semaglutide Unabated Sustainability in Treatment of Type 2 Diabetes (SUSTAIN) trials encompass a series of clinical studies evaluating the efficacy and safety of semaglutide in managing type 2 diabetes. Notably, the SUSTAIN-6 trial demonstrated cardiovascular benefits, showing a significant reduction in major adverse cardiovascular events among patients treated with semaglutide compared to those receiving placebo.
- PIONEER Clinical Trial Series: The Peptide Innovation for Early Diabetes Treatment (PIONEER) trials focused on the oral formulation of semaglutide, assessing its effectiveness in glycemic control and safety outcomes. PIONEER studies have extended the understanding of semaglutide’s benefits to a wider patient population, offering an alternative to injectable GLP-1 receptor agonists.
- Ahrén, B., et al. (2017): This study investigated semaglutide’s effects on blood glucose levels and body weight, highlighting its superiority over comparators in reducing HbA1c and promoting weight loss in patients with type 2 diabetes.
- Marso, S.P., et al. (2016): Published in the New England Journal of Medicine, this landmark paper reported the cardiovascular outcomes of the SUSTAIN-6 trial, providing critical evidence of semaglutide’s cardiovascular benefits.
- Muskiet, M.H.A., et al. (2020): This review delves into the renal outcomes associated with GLP-1 receptor agonists, including semaglutide, suggesting potential protective effects against the progression of kidney disease in patients with type 2 diabetes.
- Newsome, P.N., et al. (2021): A study exploring the efficacy of semaglutide in patients with non-alcoholic steatohepatitis (NASH), indicating significant improvements in liver health markers and fibrosis.
- Pratley, R., et al. (2018): Focusing on the safety profile of semaglutide, this analysis consolidates data from the SUSTAIN trials, providing comprehensive insights into adverse events and tolerability.
- FDA Approval Announcements: The U.S. Food and Drug Administration (FDA) approval documents for Ozempic provide detailed information on its clinical evaluation, including efficacy data, safety information, and approved indications.
These citations represent a fraction of the extensive research on semaglutide, reflecting its multifaceted role in modern therapeutics. For healthcare professionals and researchers, staying abreast of ongoing studies and emerging data is crucial for optimizing patient care and understanding semaglutide’s full potential and limitations.
Questions and Answers: Semaglutide and pancreatitis
Semaglutide has been shown to be highly effective in reducing blood glucose levels and promoting weight loss, with studies indicating it may offer superior efficacy compared to some other GLP-1 receptor agonists. In terms of safety, its profile is consistent with the class, with gastrointestinal symptoms being the most common side effects. The SUSTAIN and PIONEER trials provide comprehensive data supporting semaglutide’s benefits over placebo and certain comparators.
Yes, semaglutide has been approved for weight management in individuals without diabetes, following clinical trials that demonstrated significant weight reduction in obese or overweight patients. It is marketed under a different brand name for this indication and is part of a comprehensive weight management program that includes diet and exercise.
Long-term studies, such as the SUSTAIN-6 trial, have shown positive cardiovascular outcomes, suggesting that semaglutide may reduce the risk of major adverse cardiovascular events. Regarding renal health, evidence points to potential protective effects against the progression of kidney disease, although more long-term research is needed to fully understand these implications.
Patients with a history of pancreatitis require careful consideration before starting semaglutide. While the evidence does not conclusively link semaglutide with a significantly increased risk of pancreatitis, individual risk factors and patient history should guide treatment decisions. Healthcare providers must weigh the benefits against potential risks for each patient.
Concerns about thyroid C-cell tumors have arisen from animal studies with GLP-1 receptor agonists. However, human data have not shown a direct link between semaglutide use and an increased risk of thyroid cancer. Patients should discuss their individual risk factors with healthcare providers, and monitoring is recommended as a precaution.
Semaglutide has been associated with positive effects on cardiovascular risk factors, including reductions in systolic blood pressure and improvements in lipid profiles, such as lower LDL cholesterol levels. These benefits are likely related to semaglutide’s weight loss effects and its direct actions on glucose metabolism, contributing to its cardiovascular protective profile. However, individual results may vary, and patients should continue to follow their healthcare provider’s recommendations for managing blood pressure and cholesterol.
While semaglutide aids in weight loss and improves glycemic control, adopting a healthy diet is essential for maximizing these benefits. Healthcare providers often recommend a balanced diet rich in fruits, vegetables, whole grains, and lean proteins, along with a reduction in processed foods and sugars. Due to the gastrointestinal side effects associated with semaglutide, such as nausea and delayed gastric emptying, some patients may find smaller, more frequent meals to be more tolerable. A registered dietitian can provide personalized dietary advice to complement semaglutide treatment.
Gastrointestinal side effects are common with semaglutide, especially during the initial stages of treatment. Patients experiencing severe or persistent symptoms should consult their healthcare provider. Strategies to manage these effects include starting with a low dose of semaglutide and gradually increasing it over time to improve tolerability, staying hydrated, and possibly adjusting dietary habits. In some cases, a temporary reduction in dose or discontinuation of the medication may be necessary.
Yes, semaglutide can be used in combination with other diabetes medications, including metformin, sulfonylureas, and insulin, to achieve better glycemic control. The combination of semaglutide with other treatments should be carefully managed by a healthcare provider to optimize therapeutic outcomes and minimize the risk of hypoglycemia, especially when used with insulin or sulfonylureas. Dose adjustments and close monitoring of blood glucose levels are essential when combining therapies.
Weight loss with semaglutide generally occurs gradually, with significant results often observed within the first few months of treatment. The amount of weight loss can vary widely among individuals, depending on various factors such as baseline weight, diet, physical activity level, and adherence to the medication regimen. Clinical trials have reported an average weight loss ranging from 5% to 15% of body weight over 6-12 months. Patients should set realistic expectations and continue lifestyle interventions, including diet and exercise, to support weight loss efforts.

