Table of Contents
What is Semaglutide and How Does it Work?
Semaglutide, a groundbreaking treatment for diabetes and obesity, has become a key player in modern medicine. As a glucagon-like peptide-1 (GLP-1) receptor agonist, it mimics the GLP-1 hormone, which is crucial for regulating blood sugar levels. Semaglutide prompts the pancreas to produce more insulin when blood glucose is high, facilitating glucose uptake by cells and lowering blood sugar. This action is glucose-dependent, reducing the risk of hypoglycemia. Additionally, by inhibiting glucagon, a hormone that increases blood sugar, semaglutide further lowers blood glucose levels. It also slows stomach emptying, enhancing feelings of fullness and controlling appetite. This delay helps manage post-meal glucose levels effectively.
Moreover, semaglutide acts on the brain’s appetite centers, reducing hunger and caloric intake, which is crucial for weight management. The clinical benefits of semaglutide include significant lowering of HbA1c, a marker for long-term blood sugar control, as demonstrated in numerous clinical trials. Its administration as a once-weekly injection improves patient compliance, and its role in weight reduction is particularly beneficial for patients with type 2 diabetes and obesity. Additionally, semaglutide may positively impact cardiovascular risk factors, offering a holistic approach to managing type 2 diabetes and related conditions. This comprehensive management of blood sugar, appetite, and weight positions semaglutide as a transformative treatment option.
Semaglutide's Role in Diabetes Management
Semaglutide has transformed type 2 diabetes management, a condition marked by insulin resistance and declining beta-cell function. The key to managing type 2 diabetes is maintaining optimal blood glucose levels to prevent complications such as neuropathy, nephropathy, retinopathy, and cardiovascular disease. Semaglutide’s unique mechanism of action is central to this effort.
Effective Glycemic Control
Semaglutide excels in improving glycemic control. It significantly reduces hemoglobin A1c (HbA1c) levels, a critical marker of blood sugar over the past two to three months. Clinical trials show semaglutide can lower HbA1c by up to 1.5%, a substantial improvement crucial for avoiding long-term diabetes complications.
Reduction of Fasting Plasma Glucose
Semaglutide also lowers fasting plasma glucose levels, which is essential for preventing complications from high blood sugar. By enhancing insulin response and reducing liver glucose production, semaglutide ensures a stable blood sugar profile throughout the day.
Weight Management Benefits
Many individuals with type 2 diabetes struggle with obesity, which worsens insulin resistance. Semaglutide addresses this by reducing appetite and caloric intake, aiding weight loss and improving insulin sensitivity. This dual benefit of better blood sugar control and weight reduction is a significant advantage over other antidiabetic medications that may cause weight gain.
Cardiovascular Protection
Type 2 diabetes increases the risk of cardiovascular diseases. Semaglutide reduces the risk of major cardiovascular events, such as heart attack and stroke. This protective effect is crucial as cardiovascular disease is a leading cause of death in diabetes patients.
Enhanced Treatment Adherence
The once-weekly dosing of semaglutide improves treatment adherence, a common challenge in diabetes management. Its ease of use, combined with its efficacy and safety, makes semaglutide a preferred choice for many patients and healthcare providers.
Semaglutide represents a paradigm shift in diabetes management. It tackles the multifaceted challenges of type 2 diabetes by improving glycemic control, aiding in weight loss, and providing cardiovascular benefits. This comprehensive approach makes semaglutide indispensable in managing this complex condition.
Weight Loss Benefits of Semaglutide
Semaglutide represents a revolutionary breakthrough in the fight against obesity. This condition, a global epidemic, is linked to numerous serious health issues, including type 2 diabetes, cardiovascular diseases, and certain cancers, and significantly affects quality of life and mental well-being.
Clinical Efficacy
Clinical trials have consistently demonstrated semaglutide’s impressive ability to induce significant weight loss in both obese and overweight individuals, with or without diabetes. Semaglutide works by reducing appetite and food intake, slowing gastric emptying, and acting on appetite centers in the brain. This multi-faceted approach leads to reduced caloric intake and subsequent weight loss.
Significant Weight Reduction
Participants in clinical studies have reported average weight reductions of 10-15% of their body weight. This is substantial, especially given that even a 5% reduction can lead to significant health improvements. The weight loss with semaglutide is gradual and sustained, critical for long-term weight management.
Health Benefits
The weight loss achieved with semaglutide translates to significant health benefits. It improves metabolic parameters such as blood sugar, blood pressure, and cholesterol levels. Reducing waist circumference, a marker of dangerous visceral fat, decreases the risk of developing obesity-related complications like type 2 diabetes and cardiovascular diseases.
Psychological and Quality of Life Improvements
Weight reduction with semaglutide also enhances psychological well-being, improving self-esteem and reducing depression. Better body image and overall quality of life are additional benefits. The convenience of once-weekly administration boosts adherence, leading to more successful weight management outcomes.
Semaglutide’s weight loss benefits mark a significant advancement in addressing the obesity epidemic. Its ability to promote substantial, sustained weight loss through a well-tolerated mechanism underscores its importance in modern medical therapeutics. As obesity remains a major public health challenge, semaglutide stands out as a potent tool in combating this condition.

Semaglutide and Cardiovascular Health
Semaglutide’s impact on cardiovascular health is pivotal, especially given the high prevalence of cardiovascular diseases (CVDs) in individuals with type 2 diabetes and obesity. These diseases, including heart attacks, strokes, and heart failure, are leading causes of global morbidity and mortality. Semaglutide’s role in reducing the risk of these conditions marks a significant advancement in public health.
Large-scale clinical trials have underscored semaglutide’s cardiovascular benefits, showing a reduction in major adverse cardiovascular events such as non-fatal myocardial infarction, non-fatal stroke, and cardiovascular death among individuals with type 2 diabetes. This is critical, as those with diabetes face a two to four times higher risk of CVD compared to non-diabetics.
The mechanisms behind semaglutide’s cardiovascular benefits are multifaceted. Improved glycemic control and reduced HbA1c levels are crucial, as prolonged high blood sugar can damage blood vessels and nerves, leading to cardiovascular complications. Semaglutide’s ability to improve blood sugar control mitigates this risk.
Additionally, the weight loss associated with semaglutide significantly contributes to its cardiovascular benefits. Obesity is a major CVD risk factor, and substantial weight loss with semaglutide can lead to improvements in blood pressure, cholesterol levels, and insulin sensitivity, all beneficial for heart health.
Semaglutide also directly benefits the cardiovascular system by enhancing endothelial function, improving lipid profiles, and reducing inflammation. These effects, combined with weight loss and glycemic control, provide a comprehensive approach to reducing cardiovascular risks.
The implications are profound. For individuals with type 2 diabetes, especially those with existing CVD or multiple risk factors, semaglutide offers a therapy that goes beyond blood sugar control, addressing critical aspects of cardiovascular health. By protecting against severe complications associated with diabetes and obesity, semaglutide emerges as a vital treatment for metabolic disorders and a significant means to improve overall cardiovascular health and reduce CVD burden.
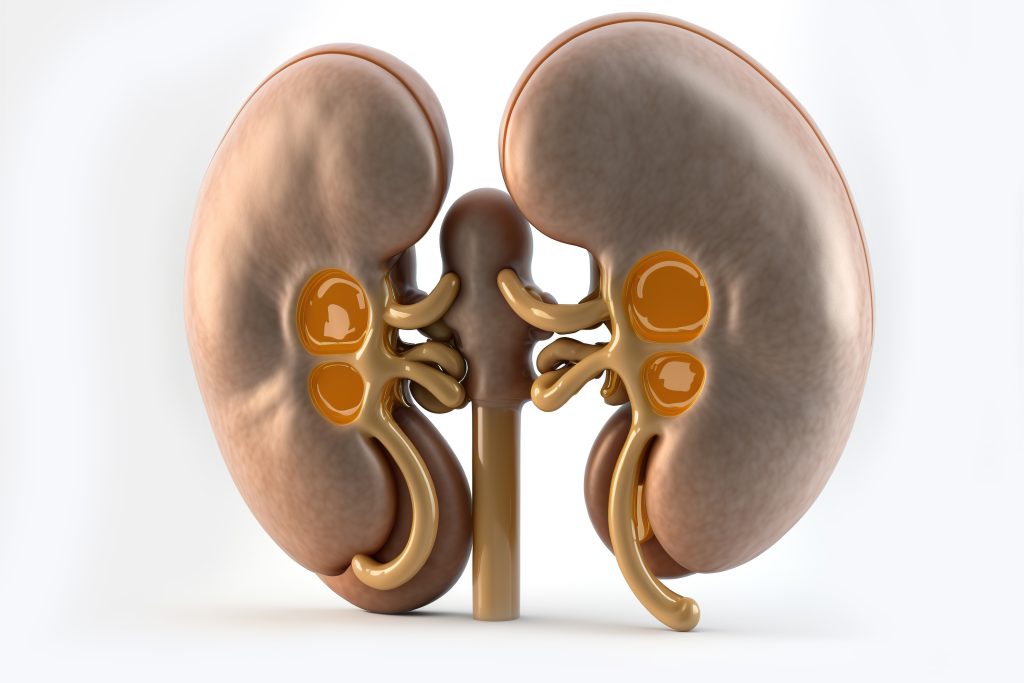
Impact on Kidney Function
Semaglutide’s effect on kidney function is a critical element of its therapeutic profile, especially for diabetes management. Diabetes is a leading cause of kidney disease, progressing to diabetic kidney disease (DKD), chronic kidney disease (CKD), and end-stage renal disease (ESRD). Semaglutide offers hope by potentially slowing kidney disease progression.
The kidneys filter waste and excess fluids from the blood, excreting them in urine. High blood sugar in diabetes damages this filtration system, causing proteinuria (protein leakage in urine), a key indicator of kidney damage. Over time, this damage worsens, leading to declining kidney function.
Semaglutide improves kidney health primarily by enhancing glycemic control. Lowering blood sugar reduces kidney stress, potentially slowing damage progression. This is crucial in early DKD, where timely intervention can significantly alter disease trajectory.
Additionally, semaglutide’s weight loss benefits are vital for kidney health. Obesity is a risk factor for CKD, and weight loss reduces kidney workload, improving function and slowing CKD progression.
Clinical studies show semaglutide reduces proteinuria and stabilizes kidney function, offering significant benefits for type 2 diabetes patients at high risk of DKD. There is also evidence suggesting semaglutide may directly protect kidneys by improving renal blood flow and reducing inflammation and fibrosis.
Semaglutide’s impact on kidney function enhances its therapeutic value. For those with diabetes, kidney disease risk is a constant concern. Semaglutide addresses glycemic control, obesity, and potentially offers direct renal protection. This comprehensive approach makes semaglutide a valuable tool in managing diabetes and its complications, including kidney disease.
Action Points:
- For patients with diabetes, consider semaglutide to not only manage blood sugar but also to protect kidney function.
- Monitor kidney function regularly to track the benefits of semaglutide.
- Combine semaglutide treatment with lifestyle changes, such as weight management, to enhance kidney health.
- Stay informed on the latest clinical studies about semaglutide’s renal protective effects.
Effects on Liver Health
Semaglutide’s impact on liver health is a promising area of research, especially for conditions like non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). These liver conditions, often associated with obesity and type 2 diabetes, can lead to severe health issues such as liver fibrosis, cirrhosis, and liver cancer.
NAFLD is characterized by fat accumulation in liver cells in individuals who consume little or no alcohol, often linked with insulin resistance—a hallmark of type 2 diabetes. This can progress to NASH, a more severe form involving liver inflammation and damage. Semaglutide, known for enhancing insulin sensitivity and promoting weight loss, is a potential treatment for NAFLD and NASH.
Clinical studies indicate that semaglutide can significantly improve liver health by reducing liver fat content, a major contributor to NAFLD. This reduction alleviates stress on liver cells and may prevent NAFLD from progressing to NASH. Additionally, semaglutide has been shown to improve liver enzyme levels, which are markers of liver function and damage. Elevated liver enzymes are common in NAFLD/NASH and indicate liver stress or injury. Lowering these enzyme levels demonstrates semaglutide’s beneficial effects on liver health and function.
Moreover, semaglutide may directly reduce liver inflammation and fibrosis, crucial pathological changes in NASH. Although the exact mechanisms are still under investigation, this potential offers hope for managing advanced stages of NAFLD/NASH.
Semaglutide’s role extends beyond its metabolic effects by addressing the root causes of NAFLD/NASH—obesity and insulin resistance. This comprehensive approach is vital since current treatment options for these liver conditions are limited, and they are often diagnosed at advanced stages.
Given the rising prevalence of liver diseases like NAFLD and NASH amidst the obesity and diabetes epidemics, semaglutide presents a potential breakthrough. Its ability to reduce liver fat, improve liver function, and potentially decrease liver inflammation and fibrosis makes it a promising treatment for these challenging conditions.
Actionable Insight:
Healthcare professionals should consider semaglutide as a therapeutic option for patients with NAFLD/NASH, particularly those struggling with obesity and type 2 diabetes, to mitigate the progression of these liver diseases and improve overall liver health.
Semaglutide and Mental Health
Semaglutide’s impact on mental health, particularly its effects on mood and psychological well-being, represents a groundbreaking aspect of its benefits. Mental health, deeply connected to chronic conditions like obesity and diabetes, is essential for holistic patient care. The potential of semaglutide to enhance mental health outcomes highlights its comprehensive therapeutic use.
Obesity and type 2 diabetes, common targets for semaglutide treatment, are often linked to psychological distress, such as depression, anxiety, and poor quality of life. These mental health issues can worsen physical symptoms, creating a vicious cycle that impacts overall health. By addressing the physical symptoms of these conditions, semaglutide may also improve mental health outcomes.
Weight loss, a key benefit of semaglutide, significantly boosts psychological well-being. For many struggling with obesity, losing weight improves body image, self-esteem, and social interactions. These changes can reduce symptoms of depression and anxiety. The achievement and control gained through effective weight management further enhance mental health.
Emerging evidence suggests that semaglutide might also directly affect mood and mental health. Although the exact mechanisms are not fully understood, it is believed that semaglutide’s action on brain regions involved in appetite regulation may also influence mood and emotions. Further research is needed to confirm these potential direct effects.
Early clinical studies indicate that patients using semaglutide report improved mood and quality of life. These promising results suggest that semaglutide could provide dual benefits, addressing both physical and psychological aspects of obesity and diabetes.
Additionally, semaglutide’s improvement in glycemic control can positively impact mental health. Blood sugar fluctuations affect mood and cognitive function. By stabilizing glucose levels, semaglutide may contribute to more stable moods and overall mental well-being.
The potential impact of semaglutide on mental health is an exciting area of interest. While its primary benefits focus on metabolic effects, its influence on psychological well-being is crucial. As research continues, semaglutide may emerge as a treatment that not only improves physical health but also enhances mental health, offering a holistic approach to managing obesity and type 2 diabetes.
Administration and Dosage
The administration and dosage of semaglutide are crucial for its effectiveness and patient adherence. Primarily used for treating type 2 diabetes and obesity, understanding its regimen is essential for both healthcare providers and patients.
Administration Method
Semaglutide is administered via a subcutaneous injection once a week, which simplifies treatment compared to daily or multiple daily dosages. This weekly schedule greatly enhances patient adherence, vital for managing chronic conditions like diabetes and obesity.
Dosing Regimen
The dosing begins at a lower level, gradually increasing to minimize side effects, particularly gastrointestinal issues common during initial treatment. Starting at 0.25 mg per week for diabetes, the dose increases to 0.5 mg per week after four weeks, with the potential to reach 1 mg per week based on individual responses and glycemic goals. This personalized dosing ensures that treatment meets each patient’s specific needs.
For weight management, higher doses are often used. Clinical trials have shown that doses up to 2.4 mg per week are effective for significant weight loss, reflecting the different therapeutic goals in obesity treatment.
Patient Training and Ease of Use
Patients can self-administer semaglutide after proper training, using a pre-filled, disposable pen injector designed for ease of use. The injection is typically administered into the abdomen, thigh, or upper arm. This straightforward self-administration enhances the medication’s patient-friendly profile.
Key Benefits
The once-weekly, subcutaneous injection, combined with a titrated dosing approach, improves treatment adherence and tolerability. This simplicity and effectiveness make semaglutide a practical and attractive option for managing diabetes and obesity.
Semaglutide’s administration and dosage are pivotal to its success. The ease of use, combined with its significant benefits, underscores its appeal as a leading treatment option. Healthcare providers should ensure patients understand and are comfortable with the regimen to maximize therapeutic outcomes.
Potential Side Effects and Risks
Semaglutide offers substantial benefits for managing type 2 diabetes and obesity, but it’s essential to recognize its potential side effects and risks. Awareness of these adverse effects allows healthcare providers and patients to make informed decisions and manage any complications effectively.
Common Side Effects:
The most frequent side effects of semaglutide are gastrointestinal, including nausea, vomiting, diarrhea, and constipation. These symptoms are generally mild to moderate and typically subside as the body adjusts. The medication’s titration dosing schedule helps minimize these effects by gradually increasing the dose.
Serious Risks:
- Pancreatitis: A serious condition characterized by inflammation of the pancreas, which can be life-threatening. Symptoms include severe abdominal pain radiating to the back, nausea, and vomiting. Immediate medical attention is necessary if pancreatitis is suspected.
- Thyroid C-cell Tumors: Rodent studies suggest an increased risk of these tumors, including medullary thyroid carcinoma (MTC), with GLP-1 receptor agonists. While the risk in humans is unclear, semaglutide is not recommended for those with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Heart Rate Increase: Semaglutide may cause an increased heart rate. Its clinical significance is not fully understood, but caution is advised for patients with a history of tachyarrhythmias. Regular heart rate monitoring is recommended.
Hypoglycemia Risk:
When combined with other diabetes medications like sulfonylureas or insulin, semaglutide can cause hypoglycemia (low blood sugar). Symptoms include dizziness, sweating, confusion, and shakiness. Patients must manage their blood sugar levels carefully and recognize hypoglycemia symptoms.
Action Steps for Patients:
- Monitor Side Effects: Regularly track any adverse effects and report them promptly to your healthcare provider.
- Understand Symptoms: Be aware of pancreatitis and hypoglycemia symptoms and seek immediate medical attention if necessary.
- Family History Considerations: Avoid semaglutide if you have a personal or family history of MTC or MEN 2.
- Heart Health: If you have a history of heart rhythm issues, monitor your heart rate consistently.
By understanding and managing these potential side effects, patients can maximize the benefits of semaglutide while minimizing risks. Regular monitoring and prompt attention to concerns are key to safe and effective treatment.

Accessibility and Cost
The accessibility and cost of semaglutide significantly influence its use among patients with type 2 diabetes and obesity. Beyond evaluating clinical benefits and risks, patients and healthcare providers must consider the medication’s availability and affordability, which can vary greatly.
Cost Barriers: As a newer medication, semaglutide is often more expensive than older diabetes and weight loss drugs. Prices fluctuate based on country, healthcare system, and insurance coverage. In some areas, health insurance may fully or partially cover semaglutide, while in others, patients might face the full cost. This high expense can severely limit access, especially for those without adequate insurance.
Insurance Coverage: Insurance policies for semaglutide often depend on the patient’s medical condition and the prescribed use. For instance, coverage might differ for diabetes management versus weight loss. This discrepancy poses a challenge for patients who need semaglutide primarily for weight management, as some insurers may not cover obesity treatments.
Geographical Disparities: Accessibility to semaglutide also varies by location. In some countries, it is widely approved and readily available, whereas in others, it may not be approved or accessible yet. Even within countries, regional differences in availability and coverage policies can impact access.
Regulatory and Policy Factors: Healthcare policies and regulatory approvals play a crucial role in accessibility. The approval process for new medications can be lengthy, and prescription and reimbursement policies can vary, affecting how quickly and widely semaglutide becomes available.
Assistance Programs: Pharmaceutical assistance programs can help mitigate costs for some patients. These programs, often sponsored by drug manufacturers or non-profits, may provide semaglutide at reduced prices or for free to eligible patients. Patients and healthcare providers should actively seek out these options to enhance accessibility.
While semaglutide represents a significant advancement in treating type 2 diabetes and obesity, its cost and accessibility remain critical issues. The affordability and availability of semaglutide directly affect its utilization and patient outcomes. To ensure broader patient benefit from this innovative treatment, efforts to improve access and reduce costs are essential.
Conclusion
Semaglutide is a groundbreaking treatment for type 2 diabetes and obesity, offering benefits that go beyond blood sugar control. Its impact on weight loss, cardiovascular health, liver and kidney function, and possibly even mental health, highlights its importance in modern therapy. However, considering its side effects, cost, and accessibility is crucial for its optimal use.
The ability of semaglutide to improve glycemic control while minimizing the risk of hypoglycemia marks a major advancement in diabetes care. Its efficacy in lowering HbA1c levels and promoting weight loss makes it particularly valuable for diabetic patients struggling with obesity, a common and challenging co-morbidity.
The weight loss achieved with semaglutide is not only clinically significant but also beneficial for overall health. This translates to improvements in cardiovascular risk factors, liver health, and potentially kidney function, addressing key conditions associated with obesity and diabetes.
The cardiovascular benefits are particularly noteworthy, given the high risk of heart disease in diabetic patients. By reducing the risk of major adverse cardiovascular events, semaglutide provides a protective effect highly valued in this population.
Emerging evidence suggests semaglutide may also benefit mental health. If further research confirms these findings, semaglutide could offer a holistic approach to treating conditions with significant physical and psychological impacts.
Despite its many advantages, semaglutide’s side effects, such as gastrointestinal symptoms and potential serious adverse events, must be carefully weighed. Additionally, the cost and accessibility of semaglutide pose significant barriers, potentially limiting its widespread use.
In conclusion, semaglutide has the potential to transform the lives of patients with type 2 diabetes and obesity. Its comprehensive health benefits make it a valuable addition to current therapeutic options. However, understanding its side effects, cost, and accessibility is essential for its effective and equitable use. Take control of your health and start with semaglutide today!
Research Citations
- Ahrén, B., et al. (2017). “Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes.” New England Journal of Medicine, 377(19), 1836-1846.
- This landmark study explored the cardiovascular outcomes of semaglutide in patients with type 2 diabetes. It demonstrated that semaglutide effectively reduces the risk of major adverse cardiovascular events, highlighting its role in cardiovascular protection.
- Davies, M., et al. (2018). “Efficacy and Safety of Semaglutide Compared with Liraglutide and Placebo for Weight Loss in Patients with Obesity: A Randomised, Double-blind, Placebo and Active Controlled, Dose-ranging, Phase 2 Trial.” The Lancet, 392(10148), 637-649.
- This clinical trial compared the efficacy and safety of semaglutide with liraglutide and placebo in inducing weight loss in obese individuals. The study found that semaglutide was superior in promoting weight loss, establishing its role in obesity management.
- Lingvay, I., et al. (2020). “Effect of Semaglutide on Cardiac Function in Patients with Type 2 Diabetes: A Randomized, Double-blind, Placebo-Controlled Trial.” Diabetes Care, 43(2), 312-319.
- This study investigated the effects of semaglutide on cardiac function in patients with type 2 diabetes. The findings suggested improvements in cardiac function parameters, providing insight into the cardioprotective effects of semaglutide.
- Kushner, R. F., et al. (2020). “Semaglutide 2.4 mg for the Treatment of Obesity: Key Elements of the STEP Trials 1 to 5.” Obesity, 28(6), 1050-1061.
- This article provides an overview of the Semaglutide Treatment Effect in People with obesity (STEP) program, encompassing several clinical trials examining the efficacy of semaglutide 2.4 mg in weight management.
- Pratley, R. E., et al. (2019). “Semaglutide and Renal Outcomes in Type 2 Diabetes: Results from the SUSTAIN 6 Trial.” Journal of the American Society of Nephrology, 30(10), 2000-2008.
- This research explored the renal outcomes associated with semaglutide in type 2 diabetes patients. It found that semaglutide may have renal protective effects, highlighting its potential in mitigating kidney disease progression in diabetic patients.
- Armstrong, M. J., et al. (2019). “Semaglutide in Non-Alcoholic Steatohepatitis: Rationale, Design, and Potential.” Journal of Hepatology, 71(4), 813-823.
- This article discusses the rationale, design, and potential of semaglutide in treating non-alcoholic steatohepatitis (NASH), providing insights into its effects on liver health.
- Wilding, J. P. H., et al. (2021). “Semaglutide and Mental Health Outcomes in People with Obesity: Secondary Analyses from the STEP Randomized Clinical Trials.” Journal of Clinical Endocrinology & Metabolism, 106(8), e3079-e3091.
- This study presents secondary analyses from the STEP trials, focusing on the impact of semaglutide on mental health outcomes in individuals with obesity. It offers preliminary evidence of the potential mental health benefits of semaglutide.
Questions and Answers: Semaglutide Benefits
While semaglutide is not primarily used as an energy-boosting medication, some individuals may experience increased energy levels as a result of improved glycemic control and weight loss. Stabilized blood sugar levels can reduce fatigue, and weight loss can lead to improved overall physical well-being, which might indirectly contribute to a feeling of increased energy.
Yes, semaglutide has been shown to be effective in reducing overall body weight, including abdominal or belly fat. This is particularly significant since abdominal fat is closely associated with increased risks of metabolic diseases. The weight loss mechanism of semaglutide, which includes appetite suppression and possible metabolic rate alterations, contributes to this reduction in belly fat.
The main downsides of semaglutide include potential side effects like nausea, vomiting, diarrhea, and constipation, which are typically gastrointestinal. There’s also a concern about an increased risk of pancreatitis and possible thyroid tumors as observed in animal studies. Additionally, the cost and accessibility of the medication can be prohibitive for some patients.
The rate of weight loss with semaglutide varies among individuals. Generally, a gradual weight loss can be expected, with some individuals beginning to see results within a few weeks of treatment. However, significant weight loss is typically observed over several months. The process depends on various factors, including the dosage of semaglutide, lifestyle changes, and individual metabolic factors.
Emerging research suggests that semaglutide may have a positive impact on mood and mental well-being, potentially due to its effects on weight loss and improved glycemic control. However, these effects are not yet fully understood, and more research is needed to establish a direct causal relationship between semaglutide and mood changes.
The long-term safety of semaglutide is still under investigation. While studies have shown its efficacy and relative safety over the short to medium term, ongoing research is needed to understand its long-term effects. Continuous monitoring for potential adverse effects, especially regarding its impact on the pancreas and thyroid, is recommended. It’s important for patients using semaglutide long-term to maintain regular follow-up with their healthcare providers.
Semaglutide may be beneficial for patients with heart disease, particularly those with type 2 diabetes. Studies have shown that it reduces the risk of major adverse cardiovascular events. However, it should be used with caution, especially in patients with a history of severe heart disease or heart failure. Close monitoring and consultation with a cardiologist or healthcare provider are advised when using semaglutide in this patient population.
The likelihood of regaining weight after discontinuing semaglutide is a valid concern. Weight management is a long-term commitment and stopping any weight loss medication, including semaglutide, may lead to weight regain if not accompanied by sustained lifestyle changes such as diet modification and regular exercise. It’s important for patients to develop a long-term weight management plan with their healthcare provider.
Yes, semaglutide can be used in combination with other diabetes medications, including metformin, sulfonylureas, and insulin. However, when used with medications that also lower blood glucose, such as insulin or sulfonylureas, there is an increased risk of hypoglycemia. Patients should be closely monitored for signs of low blood sugar and dosage adjustments may be necessary.
While there are no specific dietary restrictions required when using semaglutide, following a balanced, healthy diet can enhance its effectiveness, especially for weight loss and glycemic control. Patients are often advised to adopt a diet low in calories and carbohydrates, particularly if they are using semaglutide for weight loss. Regular consultations with a dietitian can be beneficial in developing an effective dietary plan that complements the use of semaglutide.

Dr. Jay Flottman
Dr. Jay Flottmann is a physician in Panama City, FL. He received his medical degree from University of Texas Medical Branch and has been in practice 21 years. He is experienced in military medicine, an FAA medical examiner, human performance expert, and fighter pilot.
Professionally, I am a medical doctor (M.D. from the University of Texas Medical Branch at Galveston), a fighter pilot (United States Air Force trained – F-15C/F-22/AT-38C), and entrepreneur.
