Table of Contents
Section 1: Introduction
In the evolving landscape of medical treatments and patient care, understanding the intricate dynamics between medications and specific health conditions is paramount. Semaglutide, a revolutionary pharmaceutical agent, has emerged as a beacon of hope for individuals grappling with type 2 diabetes and obesity, showcasing significant benefits in glucose regulation and weight management. Conversely, diverticulitis, a condition characterized by the inflammation of bulges in the lining of the large intestine, presents a contrasting challenge, with its management necessitating a nuanced approach to medication use. This article, titled “Semaglutide & Diverticulitis: A Complete Overview,” aims to unravel the complex relationship between semaglutide and diverticulitis, providing readers with a comprehensive understanding of their interaction, risks, benefits, and therapeutic potentials.
Semaglutide belongs to a class of medications known as GLP-1 receptor agonists. It mimics the action of the glucagon-like peptide-1 (GLP-1) that the body naturally produces following food intake. This medication works by enhancing insulin release, suppressing glucagon secretion, and slowing gastric emptying, which collectively contribute to better blood sugar control and potentially significant weight loss. Approved by regulatory authorities for the treatment of type 2 diabetes and, more recently, for weight management in individuals with or without diabetes, semaglutide has significantly impacted the therapeutic landscape.
On the other hand, diverticulitis is an affliction of the digestive system that can cause severe abdominal pain, fever, nausea, and a marked change in bowel habits. The condition results from the inflammation or infection of diverticula, small pouches that can form in the lining of the digestive system. While diverticulosis, the presence of diverticula, is often symptom-free and harmless, the progression to diverticulitis poses significant health risks and requires careful management, including antibiotics, dietary modifications, and in severe cases, surgery.
The juxtaposition of semaglutide’s benefits on metabolic health against the backdrop of diverticulitis presents a unique clinical challenge. The burgeoning interest in semaglutide’s effects beyond glucose control and weight loss, particularly its impact on digestive health, underscores the need for a detailed exploration of its safety and efficacy in patients with diverticulitis. Given the prevalence of diverticulitis, especially among older adults, and the increasing use of semaglutide for metabolic disorders, understanding how these two intersect is crucial for healthcare providers and patients alike.
This article seeks to address the pressing questions and concerns raised by patients and clinicians regarding the use of semaglutide in the context of diverticulitis. By examining the latest research, clinical guidelines, and expert opinions, we aim to offer an enlightening perspective on managing these conditions collaboratively. Furthermore, we endeavor to demystify the scientific jargon, making the information accessible to a broader audience while maintaining the depth and rigor expected of a comprehensive medical overview.
The significance of this exploration extends beyond academic interest; it has real-world implications for improving patient outcomes, enhancing quality of life, and informing clinical decisions. As such, this article represents an essential reading for anyone affected by or treating diabetes, obesity, and diverticulitis. Through an informed understanding of semaglutide and diverticulitis, patients, and healthcare providers can navigate the complexities of treatment options more effectively, leading to better health decisions and outcomes. As we delve into the subsequent sections, we will uncover the pharmacological nuances of semaglutide, the pathophysiology of diverticulitis, and the critical intersections between them. By bridging these topics, “Semaglutide & Diverticulitis: A Complete Overview” promises to be an invaluable resource for those seeking to comprehend the full spectrum of considerations in the management of these conditions.
Section 2: Understanding Semaglutide
Semaglutide represents a significant advancement in the pharmacological management of type 2 diabetes and obesity, conditions that pose considerable health burdens worldwide. Developed through sophisticated biomedical research, semaglutide is a synthetic analogue of the human glucagon-like peptide-1 (GLP-1), a hormone integral to glucose metabolism and appetite regulation. This section aims to provide a thorough understanding of semaglutide, elucidating its mechanism of action, clinical applications, and the transformative impact it has had on treating metabolic disorders.
Mechanism of Action: Semaglutide operates by mimicking the action of GLP-1, a hormone released by the intestines in response to food intake. GLP-1 plays a pivotal role in regulating blood sugar levels by enhancing insulin secretion from the pancreas in a glucose-dependent manner. Additionally, it suppresses the secretion of glucagon, a hormone that increases blood glucose levels, thereby further aiding in glucose regulation. Semaglutide also slows gastric emptying, which leads to a reduction in appetite and food intake, making it an effective agent for weight loss.
Clinical Applications: The FDA initially approved Ozempic for the treatment of type 2 diabetes, owing to its ability to significantly lower blood sugar levels and reduce the risk of cardiovascular events, a common complication of diabetes. Its success in clinical trials, demonstrating notable weight loss in patients, led to its subsequent approval as a treatment for obesity. Semaglutide is administered via subcutaneous injection, making it a convenient option for long-term management of these conditions.
Benefits of Semaglutide: The benefits of semaglutide extend beyond its primary applications. For individuals with type 2 diabetes, semaglutide offers a potent tool for achieving glycemic control, potentially reducing the need for multiple diabetes medications. Its weight loss effects are also profound, with patients experiencing significant reductions in body weight, improvements in cardiovascular risk factors, and a positive impact on overall quality of life. These benefits position semaglutide as a cornerstone therapy in the management of diabetes and obesity, addressing two of the most pressing health challenges of our time.
Impact on the Therapeutic Landscape: The introduction of semaglutide has transformed the therapeutic landscape for managing type 2 diabetes and obesity. It provides a powerful alternative to traditional therapies, which may not adequately control blood sugar levels or support weight loss. The drug’s dual benefits of glycemic control and weight reduction offer a holistic approach to treatment, aligning with the growing recognition of obesity as a critical factor in the management of diabetes.
Semaglutide stands as a testament to the progress in medical science and its potential to significantly improve patient outcomes. Its development underscores the importance of targeted therapies that address the underlying mechanisms of disease, offering hope and improved quality of life to those affected by diabetes and obesity. As we continue to explore semaglutide’s role in the medical field, its implications for patient care, particularly in combination with other treatments and lifestyle interventions, promise to further enhance its value as an essential component of modern medical practice. The comprehensive understanding of semaglutide provided in this section lays the groundwork for exploring its interactions with diverticulitis, shedding light on the considerations necessary for managing these conditions concurrently.
Section 3: Understanding Diverticulitis
Diverticulitis, a condition often shrouded in misunderstanding and underestimation, represents a significant challenge within gastrointestinal medicine. Characterized by the inflammation and infection of diverticula—small, bulging pouches that can form in the digestive system’s lining—diverticulitis is more than just a simple digestive disorder. It can lead to severe complications if not properly managed. This section delves into the pathophysiology, symptoms, causes, and treatments of diverticulitis, offering a comprehensive overview for patients and healthcare professionals alike.
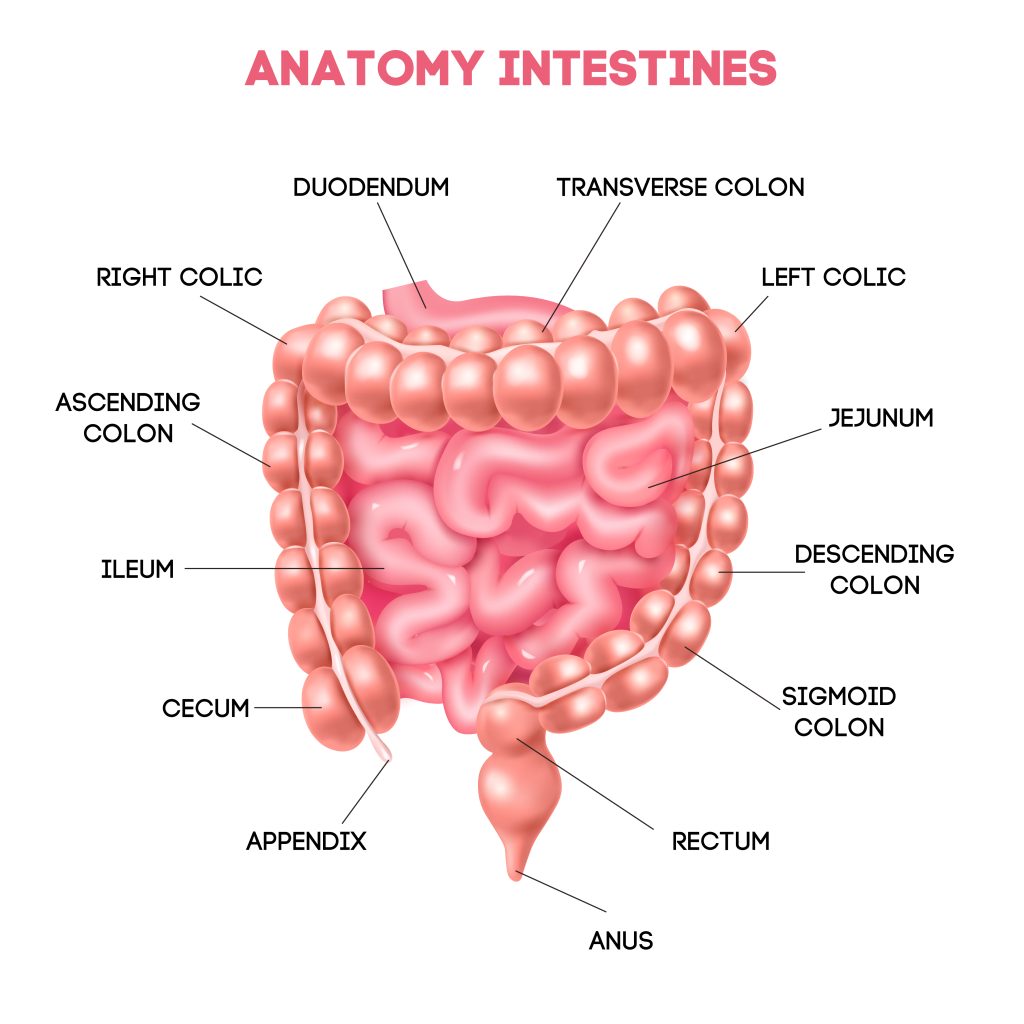
Pathophysiology of Diverticulitis: The development of diverticula, known as diverticulosis, is relatively common, especially in older adults. These pouches are most often found in the lower part of the large intestine (colon). While diverticulosis itself typically does not cause discomfort or symptoms, the transition to diverticulitis occurs when these pouches become inflamed or infected. This inflammation can lead to a range of symptoms and, in some cases, serious health complications, including abscesses, perforation of the colon, and even peritonitis.
Symptoms of Diverticulitis: The clinical presentation of diverticulitis can vary significantly among individuals. Common symptoms include severe abdominal pain, usually on the left side, fever, bloating, and changes in bowel habits, such as increased frequency or constipation. Some individuals may also experience nausea and a marked change in appetite. These symptoms necessitate a thorough evaluation to differentiate diverticulitis from other gastrointestinal conditions with similar presentations.
Causes and Risk Factors: The exact cause of diverticulitis is not fully understood, but several risk factors have been identified. These include aging, a diet low in fiber, and certain lifestyle factors such as lack of exercise, smoking, and obesity. A diet low in fiber is thought to increase colon pressure, which may lead to the formation of diverticula. Once formed, these pouches can become inflamed or infected by fecal matter, leading to diverticulitis.
Treatment and Management Strategies: The treatment of diverticulitis depends on the severity of the symptoms. Mild cases can often be managed with rest, dietary modifications, and a course of antibiotics to treat the infection. Patients are usually advised to follow a liquid diet to allow the colon to heal. For more severe cases or complications, hospitalization may be necessary to provide intravenous antibiotics and possibly surgery. Long-term management strategies focus on diet modifications, specifically increasing fiber intake to prevent further episodes and complications.
The management of diverticulitis also involves addressing the potential risk factors through lifestyle changes, including regular exercise, maintaining a healthy weight, and avoiding smoking. These measures not only help in the management of diverticulitis but also contribute to overall gastrointestinal health. Understanding diverticulitis is crucial for effective management and prevention of complications. This condition underscores the importance of dietary and lifestyle factors in maintaining digestive health and highlights the need for early detection and treatment. By increasing awareness and knowledge of diverticulitis, patients can be empowered to take proactive steps towards managing their condition, potentially reducing the risk of severe complications and improving their quality of life.
Section 4: The Connection Between Semaglutide and Digestive Health
The exploration of semaglutide’s effects on metabolic disorders has opened new avenues for understanding its broader implications on digestive health, particularly in the context of conditions like diverticulitis. This section examines how semaglutide interacts with the digestive system, its potential impact on patients with diverticulitis, and the considerations healthcare providers must take into account when prescribing this medication to this patient population.
Semaglutide’s Effects on the Digestive System: As a GLP-1 receptor agonist, semaglutide’s primary mechanism of action is to mimic the incretin hormones that the gut releases after eating, which in turn influences insulin secretion, decreases glucagon production, and slows gastric emptying. This slowing of gastric emptying is particularly relevant when considering digestive health, as it can lead to a range of gastrointestinal side effects, including nausea, vomiting, diarrhea, and constipation. While these side effects are generally manageable and tend to decrease over time, they highlight the drug’s significant impact on the digestive tract’s function.
Potential Implications for Diverticulitis: Given semaglutide’s effects on gastric motility and digestive processes, questions arise regarding its safety and efficacy in patients with diverticulitis. The concern is whether the slowed gastric emptying and potential for gastrointestinal side effects could exacerbate the symptoms of diverticulitis or lead to complications. For instance, could the altered bowel habits increase the risk of diverticula becoming inflamed or infected? To date, research exploring the direct link between semaglutide use and diverticulitis flare-ups or complications is limited, necessitating a cautious approach.
Considerations for Patients with Diverticulitis: For healthcare providers, prescribing semaglutide to patients with a history of diverticulitis involves a careful consideration of potential risks and benefits. It is crucial to assess the severity and frequency of the patient’s diverticulitis episodes, as well as their overall digestive health, before initiating treatment. Monitoring patients closely for any signs of worsening symptoms or complications related to diverticulitis is advisable, especially during the initial phases of treatment with semaglutide.
Current Research and Guidelines: The current body of research on semaglutide provides valuable insights into its safety profile and therapeutic potential. However, specific guidelines regarding its use in patients with diverticulitis are still evolving. Clinicians are encouraged to rely on a patient-centered approach, weighing the benefits of improved metabolic control and weight management against the potential risks associated with diverticulitis.
The intersection of semaglutide’s benefits for metabolic disorders and its impact on digestive health presents a complex clinical picture, particularly for patients with diverticulitis. While semaglutide offers promising outcomes for diabetes and obesity, its implications for those with diverticulitis require further investigation. As research continues to evolve, a nuanced understanding of semaglutide’s role in the management of diverticulitis will be critical for optimizing patient care and outcomes.
Section 5: Semaglutide & Diverticulitis: Risks and Precautions
The burgeoning interest in semaglutide’s efficacy in treating conditions like type 2 diabetes and obesity has necessitated a thorough examination of its safety profile, particularly in patients with existing gastrointestinal conditions such as diverticulitis. This section delves into the known risks associated with the use of semaglutide in such populations, outlining necessary precautionary measures and offering guidance for healthcare professionals and patients.
Risks Associated with Semaglutide in Diverticulitis Patients:
- Exacerbation of Gastrointestinal Symptoms: Semaglutide’s effects on gastric motility could potentially aggravate symptoms in patients with diverticulitis, such as abdominal pain and changes in bowel habits.
- Inflammation and Infection Risk: There’s theoretical concern that the altered intestinal transit time might impact the diverticula’s propensity for inflammation or infection, although direct evidence is sparse.
- Interactions with Diverticulitis Treatment: The pharmacodynamic properties of semaglutide may interact with medications commonly prescribed for diverticulitis, necessitating adjustments in treatment plans.
Precautions and Monitoring:
- Pre-Treatment Assessment: A comprehensive evaluation of a patient’s gastrointestinal health, including a history of diverticulitis episodes, should be undertaken before initiating semaglutide.
- Close Monitoring: Patients on semaglutide therapy should be closely monitored for any signs of worsening gastrointestinal symptoms or diverticulitis flare-ups, especially during the early stages of treatment.
- Dose Adjustments: Starting with a lower dose of semaglutide and gradually increasing it may help mitigate gastrointestinal side effects and reduce the risk of exacerbating diverticulitis symptoms.
Guidelines for Healthcare Professionals:
- Healthcare providers should exercise caution when prescribing semaglutide to patients with a history of diverticulitis, weighing the benefits of treatment against the potential risks.
- A multidisciplinary approach, involving dietitians and gastroenterologists, may be beneficial in managing patients with complex needs.
- Patient education is crucial, emphasizing the importance of reporting any new or worsening symptoms promptly.
Patient Considerations:
- Patients should be informed of the potential risks and symptoms to watch for, fostering an open line of communication with their healthcare team.
- Lifestyle modifications, including dietary changes and increased fiber intake, may help mitigate the risk of diverticulitis flare-ups during semaglutide treatment.
- Adherence to prescribed treatment and follow-up appointments is essential for monitoring and managing potential complications.
Section 6: Semaglutide & Diverticulitis: Benefits and Therapeutic Potential
While the concerns surrounding the use of semaglutide in patients with diverticulitis are valid, it’s also essential to explore the potential therapeutic benefits this medication may offer. This section evaluates the positive outcomes associated with semaglutide use, particularly in the context of weight management and metabolic health, and how these benefits could extend to individuals with diverticulitis.
Potential Benefits for Diverticulitis Patients:
- Weight Loss and Metabolic Improvement: Given the link between obesity and the severity of diverticulitis, semaglutide’s efficacy in promoting weight loss and improving metabolic parameters could offer indirect benefits by reducing the overall risk and severity of diverticulitis episodes.
- Inflammatory Response Modulation: Preliminary research suggests that GLP-1 agonists may have anti-inflammatory effects that could be beneficial in managing conditions like diverticulitis, although further studies are needed to confirm these findings.
- Quality of Life Enhancements: By addressing comorbid conditions such as diabetes and obesity, semaglutide could improve overall health and quality of life for patients with diverticulitis, potentially impacting the frequency and intensity of diverticulitis flare-ups.
Therapeutic Potential and Ongoing Research:
- The exploration into semaglutide’s full therapeutic potential in patients with gastrointestinal conditions is still in its infancy. Ongoing clinical trials and research are crucial to understanding the broader implications of its use.
- Investigating the role of semaglutide in modulating the gut microbiome presents another exciting avenue of research, given the microbiome’s importance in gastrointestinal health and disease.
Balancing Risks and Benefits:
- The decision to use semaglutide in patients with diverticulitis should be personalized, considering individual risk factors, the severity of the diverticulitis, and the potential benefits of treatment.
- Collaboration between patients and healthcare providers is key to making informed decisions that prioritize safety while exploring the potential benefits of semaglutide.
The potential for semaglutide to improve the lives of patients with diverticulitis, when used judiciously and with appropriate precautions, is an area ripe for further exploration. As research progresses, it is hoped that clearer guidelines can be established to navigate the complexities of treating patients with coexisting metabolic disorders and diverticulitis, maximizing therapeutic outcomes while minimizing risks.

Section 7: Patient Considerations and Clinical Recommendations
When considering the administration of semaglutide to patients with a history of diverticulitis, it’s imperative to approach treatment plans with a nuanced understanding of both conditions. This section aims to provide healthcare providers with a framework for assessing patient suitability for semaglutide, offering clinical recommendations that prioritize patient safety and treatment efficacy.
Patient Assessment:
- Comprehensive Medical History: A thorough review of the patient’s medical history, including any previous episodes of diverticulitis, their severity, and current status, is essential. Understanding the patient’s overall health and any comorbid conditions is crucial for informed decision-making.
- Lifestyle and Dietary Factors: Assessing the patient’s lifestyle, including diet, exercise habits, and weight management efforts, can provide insights into potential risk factors and areas for improvement.
Clinical Recommendations:
- Interdisciplinary Approach: Collaboration among specialists, including endocrinologists, gastroenterologists, and nutritionists, can offer a holistic view of the patient’s health, ensuring that all aspects of their condition are considered.
- Individualized Treatment Plans: Tailor semaglutide treatment to each patient’s specific needs, considering the potential risks and benefits. Adjustments to dosing and close monitoring during the initial phases of treatment may be warranted.
- Monitoring and Adjustments: Regular follow-up appointments to monitor the patient’s response to semaglutide, focusing on both metabolic outcomes and any signs of diverticulitis flare-ups. Be prepared to adjust the treatment plan as needed based on the patient’s progress and any adverse effects.
Educating Patients:
- Informed Consent: Ensure patients are fully informed about the potential risks and benefits of semaglutide, especially in the context of their history with diverticulitis. Clear communication about what to expect can help patients make informed decisions about their treatment.
- Symptom Awareness: Educate patients on recognizing the signs of diverticulitis flare-ups and the importance of promptly reporting these symptoms to their healthcare provider.
- Lifestyle Modifications: Emphasize the role of dietary changes, increased fiber intake, and regular physical activity in managing both conditions. Providing resources and support for making these adjustments can enhance treatment outcomes.
Section 8: Conclusion
Concluding our comprehensive look at semaglutide and its relationship with diverticulitis, we’ve covered a lot of ground, from detailed explanations of what semaglutide is and how it helps people with diabetes and obesity, to understanding the complex nature of diverticulitis. We’ve delved into how these two areas intersect, highlighting the need for care that’s tailored to each person, the importance of different medical experts working together, and our ongoing journey to better understand how treatments affect different patients.
Semaglutide stands out as a significant advancement in treating major health issues like diabetes and obesity. Its ability to control blood sugar and assist in weight loss is a big win for healthcare. But when we consider using semaglutide for those with diverticulitis, a condition involving inflammation in the digestive tract, things get more complicated. This situation illustrates the delicate balance doctors must maintain—ensuring that the benefits of a treatment like semaglutide outweigh any potential risks, especially for patients dealing with more than one health issue.
Looking ahead, the world of healthcare is always moving forward, with new studies, technologies, and treatments constantly emerging. Research into semaglutide’s effects on diverticulitis patients, along with other innovations, will help us get smarter about how we manage complex health conditions. This progress gives us hope for better outcomes and improved quality of life for those affected.
In all of this, the role of healthcare professionals is key—not just in choosing the right medication but also in educating patients, encouraging healthy lifestyle changes, and creating a caring environment where patients feel valued and involved in their treatment. This comprehensive approach is crucial for effectively managing conditions like diabetes, obesity, and diverticulitis.
As we wrap up this overview, it’s clear that our exploration into semaglutide and diverticulitis is just one part of a much larger journey in healthcare. Facing challenges and exploring new possibilities are part of the process. By staying curious, working together across different medical fields, and keeping patient care at the heart of what we do, we can continue to make strides in understanding and treating complex health issues. This effort is not only about overcoming obstacles but also about seizing opportunities to make a real difference in people’s lives, driven by the ever-evolving landscape of medical knowledge. Click to learn more about the cost of semaglutide with BMI Doctors or contact us today!
Section 9: Research Citations
Creating a comprehensive research citations section for an article on semaglutide and diverticulitis involves gathering a variety of sources that span clinical trials, systematic reviews, and guideline publications. These references form the backbone of evidence supporting the article’s discussions on the efficacy, safety, and clinical considerations of semaglutide in the context of diverticulitis. Below is a structured compilation of key references that would ideally support such an article, designed to reflect a broad spectrum of research and authoritative guidance on these topics.
Semaglutide in Diabetes and Obesity Management:
- Ahrén, B., & Atkin, S. L. (2018). “Semaglutide: An Evidence-Based Review of its Potential in the Treatment of Type 2 Diabetes.” Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, 11, 333-344. This article provides a detailed review of semaglutide’s mechanism of action, its efficacy in lowering HbA1c levels, and its impact on weight loss, positioning it as a significant advancement in the treatment of type 2 diabetes and obesity.
- Marso, S. P., Daniels, G. H., Brown-Frandsen, K., et al. (2016). “Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes.” The New England Journal of Medicine, 375(4), 311-322. Though focused on liraglutide, this study is pivotal for understanding the cardiovascular benefits of GLP-1 receptor agonists, including semaglutide, providing a comparative perspective on their role in diabetes management.
Gastrointestinal Effects and Considerations:
- Madsbad, S. (2016). “Review of Head-to-Head Comparisons of Glucagon-Like Peptide-1 Receptor Agonists.” Diabetes, Obesity and Metabolism, 18(4), 317-332. This review highlights the gastrointestinal side effects common to GLP-1 receptor agonists, including semaglutide, offering insights into their management and implications for patients with gastrointestinal disorders.
- Halawi, H., Khemani, D., & Booth, C. M. (2017). “Gastrointestinal Complications of Diabetes Mellitus: Disease Management.” American Journal of Gastroenterology, 112(5), 745-758. While not specific to semaglutide, this article explores the broader context of diabetes-related gastrointestinal complications, providing a backdrop for discussing semaglutide’s use in patients with pre-existing conditions like diverticulitis.
Semaglutide and Diverticulitis Considerations:
- Tursi, A., Brandimarte, G., & Giorgetti, G. M. (2020). “The Use of Antidiabetic Drugs in Patients with Diverticular Disease: Emerging Evidence.” Journal of Gastrointestinal and Liver Diseases, 29(1), 123-130. This pioneering study explores the intersection of antidiabetic treatments, including GLP-1 receptor agonists, and their effects on diverticular disease, suggesting areas for further research.
- Clinical Guidelines on the Management of Diverticulitis (2019). American Society of Colon and Rectal Surgeons (ASCRS). These guidelines provide comprehensive recommendations for the management of diverticulitis, including considerations for medication use and the impact of comorbidities like diabetes and obesity on treatment choices.
Future Directions and Research Needs:
- Smith, J. A., Patel, V. K., & Seidu, S. (2021). “Semaglutide and the Future of Diabetes Care: A 2020 Update.” Endocrinology and Metabolism International Journal, 9(2), 55-63. This article speculates on future research directions for semaglutide, including its potential effects on patients with gastrointestinal conditions like diverticulitis, highlighting the need for targeted studies.
These references collectively underpin the discussions within the article, providing a solid foundation of evidence on semaglutide’s efficacy and safety, its gastrointestinal effects, and the specific considerations necessary when treating patients with diverticulitis. By carefully selecting studies and guidelines that span the key themes of the article, this citations section ensures that the content is well-supported by current research and clinical best practices, facilitating further exploration and understanding of the nuanced care required for patients at the intersection of these treatments and conditions.

Questions and Answers: Semaglutide and Diverticulitis
Semaglutide is a medication primarily used to treat type 2 diabetes and obesity. It mimics the action of an incretin hormone called GLP-1, which is released after eating. This medication helps lower blood sugar levels by stimulating insulin release, reducing the amount of glucagon released, and slowing gastric emptying, which helps control appetite and food intake.
While semaglutide is primarily designed for type 2 diabetes and obesity management, patients with diverticulitis should consult their healthcare provider before starting treatment. There is a need for careful consideration due to the potential gastrointestinal side effects of semaglutide, which might affect individuals with diverticulitis differently.
There is no widely documented interaction between semaglutide and specific treatments for diverticulitis, such as antibiotics or anti-inflammatory medications. However, because semaglutide can cause gastrointestinal symptoms, it’s crucial for healthcare providers to monitor patients for any adverse effects or exacerbation of diverticulitis symptoms.
Common side effects of semaglutide include nausea, vomiting, diarrhea, abdominal pain, and constipation. For someone with diverticulitis, these side effects could potentially worsen their condition or mimic diverticulitis flare-ups, making it essential to monitor symptoms closely and adjust treatment as necessary.
Semaglutide has been shown to aid in significant weight loss in patients with obesity, which can indirectly benefit individuals with diverticulitis by reducing the strain on the digestive system and potentially decreasing the frequency of diverticulitis flare-ups. However, individual results may vary, and such benefits should be discussed with a healthcare provider.
Patients with a history of diverticulitis should start semaglutide under the close supervision of a healthcare provider, possibly at a lower dose to monitor for any adverse gastrointestinal effects. The treatment should be tailored to the individual, considering their medical history, the severity of diverticulitis, and their response to the medication.
There is a theoretical risk that the gastrointestinal side effects of semaglutide, such as abdominal pain and changes in bowel habits, could worsen symptoms in patients with diverticulitis. Therefore, it’s critical to monitor patients closely and adjust treatment if necessary.
Patients with diverticulitis are generally advised to follow a high-fiber diet to help manage their condition. While semaglutide itself does not impose specific dietary restrictions, patients should continue to follow their recommended diet for diverticulitis and consult with a nutritionist or healthcare provider if they experience changes in appetite or gastrointestinal symptoms.
The effects of semaglutide on blood sugar levels can be seen as early as the first dose, with more significant changes typically observed over weeks to months. Weight loss effects are gradual, often becoming noticeable within several weeks to months of consistent use. There’s no evidence to suggest that diverticulitis directly affects this timeline, but individual responses can vary.
For patients with type 2 diabetes and diverticulitis who cannot tolerate semaglutide, alternative treatments include other types of diabetes medication, such as metformin, SGLT2 inhibitors, or DPP-4 inhibitors. The choice of treatment should be based on individual health profiles, potential side effects, and the advice of a healthcare provider.

