Table of Contents
Introduction
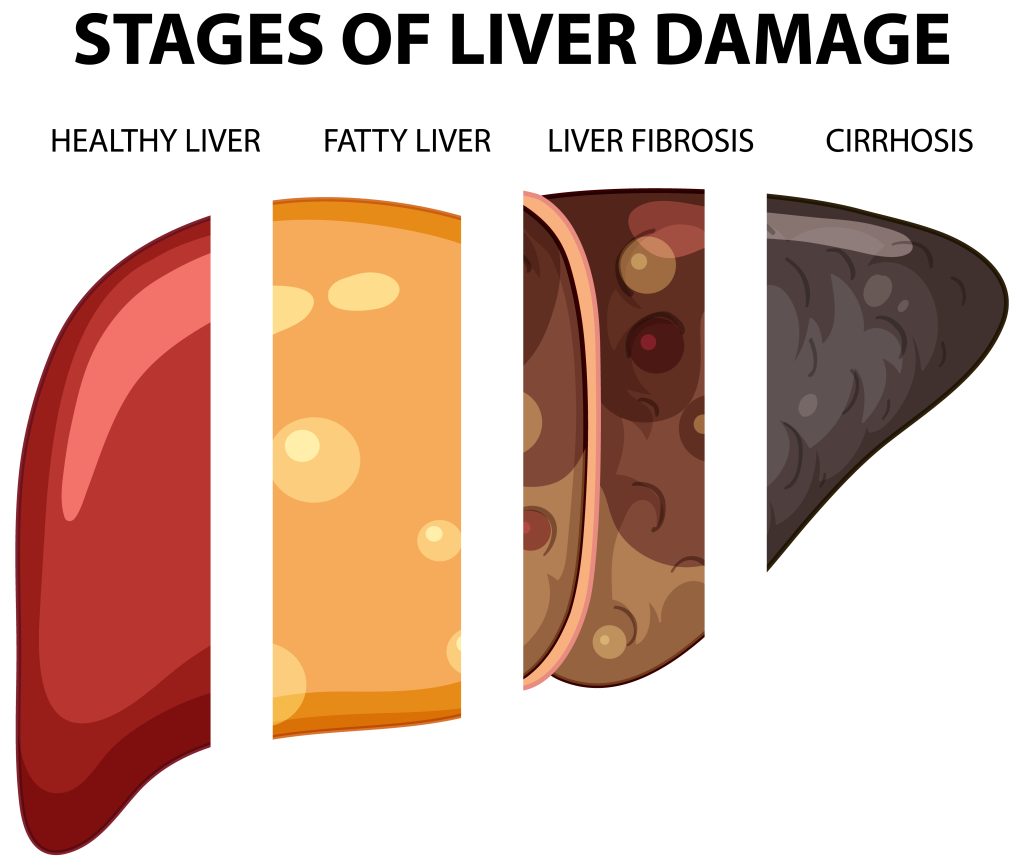
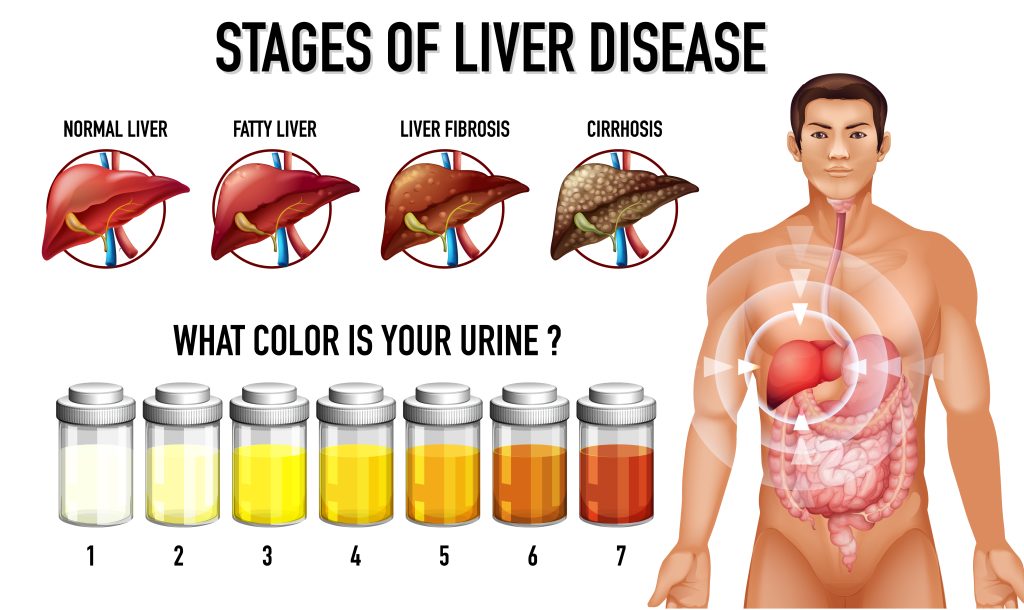
Non-Alcoholic Fatty Liver Disease (NAFLD) encompasses various liver conditions not caused by alcohol consumption. Characterized by the buildup of fat in the liver (steatosis), NAFLD is a growing global health concern, affecting about 25% of people worldwide. It’s strongly linked to obesity, type 2 diabetes, and metabolic syndrome, all increasingly prevalent in modern society. This chronic liver disease can progress from simple steatosis to non-alcoholic steatohepatitis (NASH), involving inflammation and liver cell damage, and can further advance to fibrosis, cirrhosis, and hepatocellular carcinoma.
NAFLD often remains undiagnosed due to its silent onset and lack of specific early symptoms. Traditionally, managing NAFLD focuses on lifestyle changes like diet and exercise, but these are hard to maintain and don’t work for everyone. Therefore, pharmacological treatments are being increasingly considered, especially for those with NASH or significant fibrosis.
Semaglutide, originally developed for type 2 diabetes, shows promise for NAFLD treatment. As a glucagon-like peptide-1 (GLP-1) receptor agonist, Semaglutide mimics GLP-1 hormone functions, which regulate appetite and insulin secretion. Recent studies indicate that Semaglutide can effectively manage NAFLD by inducing weight loss and improving insulin sensitivity, both crucial in addressing the disease. Even modest weight loss can significantly reduce liver fat, inflammation, and fibrosis, while better glycemic control benefits those with diabetes.
Clinical trials have shown positive outcomes for Semaglutide in NAFLD management. A notable study in the New England Journal of Medicine reported significant reductions in liver fat and fibrosis markers in NASH patients treated with Semaglutide.
In this guide, we will explore Semaglutide’s mechanisms, benefits, side effects, and practical applications for NAFLD. We will also discuss how this medication fits into the broader NAFLD management landscape, considering current research and future directions.
Understanding NAFLD’s complexities and Semaglutide’s emerging role in its treatment is essential for healthcare providers, patients, and their families. This represents a significant advancement in addressing a silent yet widespread health issue affecting millions globally.
Non-Alcoholic Fatty Liver Disease (NAFLD): Understanding and Action Steps
Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition where excess fat accumulates in liver cells, not due to alcohol use. It is now the most prevalent chronic liver disease globally, closely tied to obesity and type 2 diabetes. NAFLD spans a range of liver disorders, from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), which involves liver inflammation and cell damage. In advanced stages, it can lead to liver fibrosis, cirrhosis, and even liver cancer.
Causes and Risk Factors
NAFLD’s development is multifaceted, often linked to metabolic syndrome—a cluster of conditions including obesity, insulin resistance, hypertension, and dyslipidemia. Insulin resistance is a key factor, causing increased liver fat and making the liver more vulnerable to inflammation and fibrosis. The prevalence of NAFLD is about 25% worldwide, higher in individuals with obesity and type 2 diabetes. Rates are particularly high in regions like the Middle East and South America. Men are more commonly affected than women, and the risk increases with age. Alarmingly, rising obesity in children is leading to more pediatric NAFLD cases.
Symptoms and Diagnosis
NAFLD often has no symptoms, especially in early stages, and is usually detected through abnormal liver function tests or imaging studies for other reasons. When symptoms do occur, they are typically vague, such as fatigue and discomfort in the upper right abdomen. Diagnosing NAFLD involves a thorough medical history, blood tests, imaging studies, and sometimes a liver biopsy. Distinguishing NAFLD from alcoholic liver disease and other liver conditions is crucial. A liver biopsy, though invasive, is the gold standard for diagnosing NASH and assessing liver fibrosis.
Public Health Impact
The increasing prevalence of NAFLD poses a significant public health challenge, heightening the risk of liver-related morbidity, mortality, and cardiovascular diseases. Understanding NAFLD, its risk factors, and potential complications is critical for effective management and prevention.
Call to Action
To combat this widespread and complex disease, it’s essential to:
- Promote Healthy Lifestyles: Advocate for balanced diets and regular exercise to prevent obesity.
- Regular Screening: Encourage routine liver function tests, especially for those at higher risk.
- Early Intervention: Seek medical advice at the first sign of liver discomfort or fatigue.
- Research and Education: Support ongoing research and public health campaigns to raise awareness about NAFLD.
Upcoming Treatment Options
Stay informed about emerging treatments. The next sections will explore the role of Semaglutide, a promising new therapy, in managing NAFLD.
Understanding Semaglutide
Semaglutide is a groundbreaking pharmaceutical agent, lauded for its effectiveness in treating type 2 diabetes and Non-Alcoholic Fatty Liver Disease (NAFLD). As a glucagon-like peptide-1 (GLP-1) receptor agonist, it mimics the action of the natural hormone GLP-1, essential for glucose metabolism and appetite regulation.
Mechanism of Action
Semaglutide’s multifaceted mechanism primarily involves stimulating insulin secretion and suppressing glucagon secretion in a glucose-dependent manner. This selective action reduces high blood sugar levels without causing hypoglycemia, a common issue with other diabetes medications. Additionally, it slows gastric emptying, reducing appetite and calorie intake, which aids in weight loss.
Impact on Weight Loss and NAFLD
The weight loss effects of Semaglutide are substantial, making it particularly beneficial for NAFLD management. Excess body weight, especially central obesity, is a major risk factor for NAFLD. Weight loss induced by Semaglutide significantly reduces liver fat content, crucial for managing NAFLD. Research shows that a 5-10% body weight reduction can markedly improve liver fat, inflammation, and fibrosis in NAFLD patients.
Clinical Evidence
Numerous large-scale clinical trials have documented Semaglutide’s efficacy in managing blood sugar levels and promoting weight loss. The SCALE study demonstrated significant weight loss with GLP-1 receptor agonists, including Semaglutide. The STEP program further confirmed its effectiveness in weight management.
Benefits Beyond Glucose Control
Semaglutide may also offer direct benefits to liver health. Studies indicate improvements in liver function markers and reductions in liver inflammation and fibrosis, although the precise mechanisms are still under investigation.
Administration and Dosing
Semaglutide is administered via subcutaneous injection, which patients can self-administer. The dosing starts low and gradually increases to minimize gastrointestinal side effects, ensuring patient compliance and maximizing therapeutic benefits.
Semaglutide represents a novel approach to managing NAFLD, with dual benefits in glycemic control and weight management. Its potential to improve liver outcomes, combined with its proven efficacy in diabetes management, makes it a potentially transformative agent in metabolic disease treatment. The following sections will delve deeper into Semaglutide’s clinical benefits, potential side effects, and real-world applications.
The Link Between Semaglutide and NAFLD
Semaglutide’s potential in treating Non-Alcoholic Fatty Liver Disease (NAFLD) is a groundbreaking development in the medical field. This drug’s ability to address core factors of NAFLD—insulin resistance, obesity, and metabolic syndrome—makes it a promising candidate for effective treatment.
NAFLD is marked by fat accumulation in liver cells, often due to insulin resistance and obesity. These conditions disrupt glucose and fat metabolism, leading to fat buildup in the liver. Over time, this can cause inflammation, liver cell damage, fibrosis, and severe complications like cirrhosis and liver cancer.
Semaglutide improves insulin sensitivity and promotes weight loss, directly tackling the root causes of NAFLD. Enhancing the body’s response to insulin helps reduce liver fat associated with insulin resistance. Furthermore, Semaglutide-induced weight loss significantly decreases liver fat, preventing NAFLD progression and potentially reversing its effects.
Empirical evidence supports Semaglutide’s role in NAFLD management. A notable study in the “New England Journal of Medicine” showed that Semaglutide significantly reduced liver fat and fibrosis markers in patients with NASH, a severe form of NAFLD. These findings are encouraging, indicating that Semaglutide not only manages metabolic aspects of NAFLD but also improves liver pathology.
Additionally, Semaglutide’s ability to lower blood glucose levels benefits NAFLD patients with type 2 diabetes, reducing the risk of liver-related complications. This dual benefit underscores the drug’s potential as a comprehensive treatment.
The connection between Semaglutide and NAFLD signifies a major advancement in managing this liver disease. By targeting the metabolic roots of NAFLD, Semaglutide offers a holistic treatment approach, addressing both liver-specific and systemic aspects. Further exploration of its clinical benefits, potential side effects, and practical use will enhance our understanding and application of this promising therapy.
Benefits of Semaglutide in NAFLD Management
Semaglutide has emerged as a promising treatment for Non-Alcoholic Fatty Liver Disease (NAFLD), offering a range of benefits that address key aspects of the disease. This section highlights the clinical advantages of Semaglutide in NAFLD management, based on recent studies and clinical trials.
Reduction in Liver Fat Content
Semaglutide significantly reduces liver fat, a hallmark of NAFLD. This reduction is essential in preventing further liver damage. Studies show marked decreases in liver fat, as measured by MRI and ultrasound, in patients treated with Semaglutide.
Improvement in Liver Enzymes
Semaglutide lowers elevated liver enzymes (ALT and AST), indicating reduced liver inflammation and damage. Normalizing these enzymes often correlates with improved liver health, making this a positive prognostic indicator.
Impact on Liver Fibrosis
Semaglutide has shown potential in reducing liver fibrosis, the scarring response to injury, which is crucial in preventing the progression to cirrhosis. Early research suggests improvements in fibrosis markers in patients with NASH, a severe form of NAFLD.
Metabolic Benefits
Beyond its impact on liver fat, Semaglutide improves insulin sensitivity and glucose metabolism, benefiting patients with type 2 diabetes, a common comorbidity in NAFLD. Better glycemic control further reduces liver damage risk.
Weight Loss and Appetite Control
Semaglutide promotes sustained weight loss by reducing appetite and calorie intake. This weight loss is vital for reducing liver fat and improving other aspects of metabolic syndrome, such as hypertension and dyslipidemia, which further benefits NAFLD patients.
Cardiovascular Benefits
Patients with NAFLD are at a higher risk of cardiovascular diseases. Semaglutide reduces cardiovascular risk factors, including high blood pressure and abnormal lipid profiles, addressing the high incidence of heart disease in these patients.
Quality of Life Improvements
By improving liver health, promoting weight loss, and enhancing metabolic control, Semaglutide significantly boosts the quality of life for NAFLD patients. Many report increased energy levels, improved physical functioning, and overall well-being.
Semaglutide offers a comprehensive approach to NAFLD management, targeting the disease’s root causes and secondary effects. Its ability to reduce liver fat, improve liver enzymes, potentially reverse fibrosis, and provide metabolic and cardiovascular benefits positions it as a promising treatment option. The next sections will explore Semaglutide’s potential side effects and practical considerations in its use for NAFLD patients.
Potential Side Effects and Risks of Semaglutide
While Semaglutide is a promising treatment for Non-Alcoholic Fatty Liver Disease (NAFLD), it is essential to understand its potential side effects and risks. This knowledge is crucial for both healthcare providers and patients to make well-informed decisions about treatment. Here, we outline the common and rare side effects of Semaglutide and provide strategies for managing them.
Gastrointestinal Side Effects
The most common side effects are gastrointestinal, including nausea, vomiting, diarrhea, and constipation. These symptoms are typically mild to moderate and diminish over time. A slow titration schedule can help reduce these effects. However, some patients may experience more severe symptoms, possibly leading to discontinuation. To manage these effects, maintaining adequate hydration and making dietary adjustments is recommended.
Risk of Hypoglycemia
Although Semaglutide alone is not usually linked to high hypoglycemia risk, this risk increases when combined with other antidiabetic medications like sulfonylureas or insulin. Patients on these combinations must monitor their blood glucose levels regularly and adjust dosages as needed, under healthcare professional guidance.
Pancreatitis
There have been reports of acute pancreatitis in patients using GLP-1 receptor agonists, including Semaglutide. Patients should be aware of pancreatitis symptoms, such as severe abdominal pain, and seek immediate medical attention if they occur. Semaglutide should be discontinued if pancreatitis is suspected.
Changes in Appetite and Weight Loss
While weight loss is beneficial for NAFLD treatment, excessive weight loss or decreased appetite can be problematic, especially for patients at a healthy weight or with a history of eating disorders. Regular monitoring of weight and nutritional intake is advised.
Thyroid Tumors
Animal studies have shown a potential link between GLP-1 receptor agonists and thyroid C-cell tumors. While this risk in humans remains unclear, caution is advised for patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
Allergic Reactions
Allergic reactions to Semaglutide, though rare, can occur. Symptoms range from rash, itching, and hives to severe reactions like difficulty breathing and facial swelling. Immediate medical attention is essential if an allergic reaction is suspected.
Renal Impairment
There have been reports of worsening renal function, including acute renal failure, in patients treated with GLP-1 receptor agonists. Patients with pre-existing renal disease or severe gastrointestinal reactions leading to dehydration should be closely monitored for changes in renal function.
Cardiovascular Effects
While Semaglutide has shown cardiovascular benefits, it can increase resting heart rate in some patients. It should be used cautiously in patients with a history of tachyarrhythmias.
Semaglutide offers significant benefits for managing NAFLD, but awareness and management of its side effects are crucial. Regular monitoring and prompt attention to any concerning symptoms ensure that patients can maximize the benefits of Semaglutide while minimizing risks. The next sections will cover the dosage and administration of Semaglutide and lifestyle considerations for patients undergoing treatment.

Dosage and Administration of Semaglutide for NAFLD
When using Semaglutide to treat Non-Alcoholic Fatty Liver Disease (NAFLD), it’s crucial to understand the proper dosage and administration to ensure effectiveness and safety. This section outlines the recommended dosage, administration methods, and monitoring requirements.
Starting Dosage and Titration
Begin Semaglutide at 0.25 mg weekly to minimize gastrointestinal side effects. After four weeks, increase to 0.5 mg weekly. Depending on the patient’s response and tolerance, the dose can be further increased, with a maximum of 1.0 mg weekly. Follow a gradual titration schedule to avoid increased side effects, especially gastrointestinal discomfort.
Administration Method
Semaglutide is administered via subcutaneous injection. Patients are trained to self-administer using a pre-filled, single-use pen injector. Rotate injection sites (abdomen, thigh, or upper arm) to reduce the risk of lipodystrophy and irritation. Injections can be given any time of day, with or without meals, offering flexibility.
Monitoring Response to Treatment
Regular monitoring is essential to assess the effectiveness and tolerance of Semaglutide. Track changes in liver enzymes, liver fat content (via imaging), and other liver health markers. Monitor weight, blood glucose levels, and HbA1c (for diabetic patients). Regular follow-ups with healthcare providers are crucial to adjust doses and manage side effects.
Considerations for Special Populations
Exercise caution when prescribing Semaglutide to patients with renal or hepatic impairment. Although dose adjustments are generally not required, these patients need close monitoring for side effects and efficacy. Elderly patients and those with a history of pancreatitis require careful consideration and monitoring.
Addressing Missed Doses
If a dose is missed, take it as soon as possible within five days. If more than five days have passed, skip the missed dose and take the next dose on the regular schedule. This approach maintains consistent medication levels and ensures optimal efficacy.
Patient Education and Support
Effective patient education about Semaglutide use, potential side effects, and treatment adherence is essential. Providing support and resources, such as nursing services or educational materials, can enhance compliance and treatment success.
Proper dosage, careful administration, and close monitoring of Semaglutide are key to managing NAFLD effectively. Individualize treatment plans based on patient response, tolerability, and specific health considerations. Subsequent sections will explore lifestyle modifications and additional therapies to complement Semaglutide treatment for NAFLD.
Lifestyle Considerations and Additional Therapies in NAFLD Management
Managing Non-Alcoholic Fatty Liver Disease (NAFLD) transcends pharmacological interventions like Semaglutide. Central to effective treatment are lifestyle modifications, often the first line of defense against disease progression. This section delves into essential lifestyle changes and complementary therapies that enhance the comprehensive management of NAFLD.
Dietary Changes
Diet is paramount in NAFLD management. A balanced diet, low in saturated fats, sugars, and refined carbohydrates, and high in fiber, significantly reduces liver fat. The Mediterranean diet, rich in fruits, vegetables, whole grains, lean protein, and healthy fats (such as olive oil), is especially beneficial. Achieving and maintaining a healthy weight through calorie reduction is crucial, as weight loss markedly improves liver health in NAFLD patients.
Physical Activity
Regular physical activity is a cornerstone of NAFLD management. Exercise reduces liver fat and improves insulin sensitivity, even without notable weight loss. Patients should aim for at least 150 minutes of moderate-intensity aerobic exercise per week, complemented by muscle-strengthening activities. Engaging in enjoyable activities like brisk walking, cycling, or swimming ensures consistency and long-term adherence.
Alcohol and Smoking
Although NAFLD is not alcohol-induced, minimizing alcohol intake is advisable to prevent further liver damage. Smoking cessation is equally vital, as smoking exacerbates liver inflammation and fibrosis.
Additional Therapies
Beyond lifestyle changes, other therapeutic options may enhance the effects of Semaglutide. Vitamin E and pioglitazone have shown benefits for some NAFLD patients, particularly those with NASH. These treatments should be tailored to individual patient profiles and medical histories.
Bariatric Surgery
For patients with severe obesity and NAFLD, bariatric surgery can be a viable option. This surgery not only leads to significant weight loss but also improves metabolic parameters and liver health. However, it is typically considered only when other interventions have failed and should be evaluated on a case-by-case basis.
Monitoring and Regular Health Check-ups
Ongoing monitoring of liver health through blood tests, imaging, and sometimes liver biopsies is crucial. These check-ups track disease progression and treatment efficacy. Regular consultations with healthcare providers, including hepatologists, dietitians, and physical therapists, ensure continuous support and necessary adjustments to the treatment plan.
Mental Health
Addressing mental health is vital in managing chronic illnesses like NAFLD. Support from mental health professionals, support groups, or counseling can help patients cope with stress, anxiety, or depression associated with long-term health conditions.
Managing NAFLD requires a holistic approach that combines pharmacological treatments like Semaglutide with lifestyle interventions and additional therapies. A multidisciplinary team, including dietitians, exercise physiologists, and medical professionals, is crucial for effective management. The following sections will share patient perspectives and testimonials on Semaglutide treatment, offering real-world insights into its impact on NAFLD management.
Patient Perspectives and Testimonials on Semaglutide Treatment
Patient experiences and testimonials offer crucial insights into the real-world impact of Semaglutide for treating Non-Alcoholic Fatty Liver Disease (NAFLD). This section explores patient journeys, highlighting their challenges and successes with Semaglutide.
Experiences with Semaglutide’s Effectiveness
Patients frequently report significant improvements in their condition with Semaglutide, including reduced liver enzymes, better liver function tests, weight loss, and improved blood sugar control. Those with type 2 diabetes often find dual benefits in managing both their diabetes and liver health.
Weight Loss Journeys
A standout benefit of Semaglutide is its impact on weight loss. Many patients share inspiring stories of successful weight reduction, which enhances their liver health, overall well-being, and energy levels. However, weight loss results can vary, and some patients may need additional support, such as dietary counseling.
Managing Side Effects
Patients also discuss the challenge of managing side effects, particularly gastrointestinal issues like nausea and reduced appetite. Strategies to cope include dietary adjustments, smaller, frequent meals, and gradual medication titration under medical guidance.
Psychological and Emotional Impact
The testimonials reveal the emotional journey of dealing with NAFLD and its treatment. While the initial diagnosis can be distressing, many patients feel relieved and empowered by actively managing their condition with Semaglutide and lifestyle changes. Improved health metrics often lead to increased optimism and motivation.
The Role of Healthcare Support
Patients emphasize the importance of support from healthcare professionals. Regular follow-ups, personalized advice, and the sense of being monitored and cared for are crucial. The roles of hepatologists, endocrinologists, dietitians, and primary care physicians are frequently praised.
Varied Responses and Personalized Experiences
Patient responses to Semaglutide can vary. While many report positive outcomes, some experience less pronounced benefits or struggle with side effects. These variations highlight the need for personalized treatment approaches and ongoing research in NAFLD management.
Patient testimonials on Semaglutide for NAFLD illustrate a journey of hope and challenge. They showcase the medication’s potential to improve liver health and quality of life while emphasizing the need to manage side effects, provide supportive care, and personalize treatment. These real-world insights are invaluable in understanding Semaglutide’s holistic impact on NAFLD management. The next sections will explore the future of Semaglutide in NAFLD treatment and the broader landscape of this liver condition.
The Future of Semaglutide in NAFLD Treatment
Semaglutide is at the forefront of innovative treatments for Non-Alcoholic Fatty Liver Disease (NAFLD). Emerging research and ongoing clinical trials indicate promising advancements that could transform patient care. This section delves into the future of Semaglutide in NAFLD treatment, highlighting ongoing studies, anticipated breakthroughs, and broader health implications.
Ongoing Research and Clinical Trials
Semaglutide’s efficacy in treating NAFLD is under rigorous investigation through numerous clinical trials. Researchers are evaluating its long-term benefits, optimal dosing, and safety across diverse populations. Key areas of interest include its effects on advanced NAFLD stages, such as non-alcoholic steatohepatitis (NASH) and fibrosis. Additionally, studies are uncovering the molecular mechanisms by which Semaglutide influences liver metabolism and pathology, paving the way for more targeted therapies.
Personalized Medicine Approaches
As our understanding of NAFLD and its subtypes grows, treatment is shifting towards personalized medicine. Genetic, environmental, and lifestyle factors significantly impact NAFLD progression. Future treatment strategies, including Semaglutide use, will likely be tailored to individual patient profiles, optimizing efficacy and minimizing side effects.
Combination Therapies
Combining Semaglutide with other therapeutic agents shows promise for enhancing treatment outcomes. For instance, pairing Semaglutide with drugs targeting liver fibrosis could offer powerful solutions for patients with advanced disease stages.
Broader Implications for Metabolic Health
Semaglutide’s benefits extend beyond NAFLD, impacting weight loss, glucose metabolism, and cardiovascular risk factors. This positions Semaglutide as a potential cornerstone in managing metabolic syndrome and related conditions, heralding a new era in metabolic disease treatment.
Challenges and Opportunities
Despite its potential, challenges remain. Ensuring Semaglutide’s affordability and accessibility is crucial. Moreover, patient adherence and education for both patients and healthcare providers are essential to maximize treatment benefits.
The Role of Technology and Digital Health
Technological advancements, including digital health tools and telemedicine, will increasingly support NAFLD management. These tools can monitor treatment responses, manage side effects, and provide essential patient education and support, especially for chronic conditions like NAFLD.
The future of Semaglutide in NAFLD treatment is promising, with significant advancements on the horizon. As research progresses, we will better understand how to utilize this medication effectively, both as a standalone treatment and in combination with other therapies. Integrating personalized medicine and digital health tools will further enhance NAFLD management, offering a holistic and patient-centered approach to this growing health concern. Subsequent sections will provide a comprehensive summary and final insights into Semaglutide’s impact on NAFLD management.
Conclusion
This guide has comprehensively examined the role of Semaglutide in treating Non-Alcoholic Fatty Liver Disease (NAFLD), highlighting its benefits, challenges, and future potential. As we conclude, let’s revisit the key points and consider their broader implications for NAFLD patients and the healthcare community.
Semaglutide stands out in the NAFLD landscape due to its significant impact on metabolic health and liver function. It reduces liver fat content, improves liver enzyme levels, and may reverse liver fibrosis, making it a promising treatment option. Additionally, its benefits in weight loss and glycemic control make it versatile, especially for patients with type 2 diabetes.
While Semaglutide is promising, NAFLD management requires a holistic approach. Lifestyle modifications, such as a healthy diet, regular physical activity, and alcohol avoidance, are essential. Combining these changes with Semaglutide treatment can lead to the best outcomes, underscoring the importance of a comprehensive management strategy.
Patient experiences with Semaglutide vary, emphasizing the need for personalized care. Treatment plans should be tailored, regularly monitored, and adjusted based on individual responses and health profiles to maximize effectiveness and minimize side effects.
Ongoing research into Semaglutide’s long-term effects offers hope for more refined treatment strategies. The potential for personalized medicine, combination therapies, and digital health advancements could further revolutionize NAFLD management. However, challenges such as accessibility, cost, and patient adherence need to be addressed to fully leverage Semaglutide’s potential.
Advancing our understanding and management of NAFLD requires ongoing research and education. Healthcare professionals must stay updated on the latest treatments like Semaglutide and educate patients about lifestyle modifications and adherence to treatment regimens.
In conclusion, Semaglutide represents a significant advancement in NAFLD treatment, offering hope for improved outcomes in a condition that has been difficult to manage. Its ability to address underlying metabolic issues and improve liver health makes it a valuable addition to the therapeutic arsenal. However, the best approach to NAFLD management remains comprehensive, involving medication, lifestyle changes, and regular medical monitoring. Embracing these multifaceted strategies will be crucial in improving the lives of those affected by NAFLD.
For more information, visit our Semaglutide cost page.
Research Citations
Non-alcoholic fatty liver disease (NAFLD) is a common hepatic disorder characterized by excessive fat accumulation in the liver, ranging from simple steatosis to non-alcoholic steatohepatitis (NASH) and fibrosis. Emerging evidence suggests a potential role for glucagon-like peptide-1 receptor agonists (GLP-1 RAs), such as semaglutide, in the treatment of NAFLD, owing to their effects on weight loss, insulin sensitivity, and hepatic lipid metabolism. This article reviews current research on the use of semaglutide in NAFLD, including its mechanisms of action, clinical efficacy, and safety profile, highlighting opportunities and challenges in its implementation as a therapeutic option for NAFLD.
- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84. doi:10.1002/hep.28431
- US Food and Drug Administration (FDA). Highlights of prescribing information: Rybelsus (semaglutide) tablets, for oral use. Accessed January 10, 2024. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf
- Semaglutide – Novo Nordisk. Drugs.com. https://www.drugs.com/mtm/semaglutide.html. Accessed January 10, 2024.
- Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357. doi:10.1002/hep.29367
- Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679-690. doi:10.1016/S0140-6736(15)00803-X
- Newsome PN, Buchholtz K, Cusi K, et al. A placebo-controlled trial of subcutaneous semaglutide in nonalcoholic steatohepatitis. N Engl J Med. 2021;384(12):1113-1124. doi:10.1056/NEJMoa2028395
- Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;385(9972):956-965. doi:10.1016/S0140-6736(14)61933-4
- Francque S, Bedossa P, Ratziu V, et al. Liraglutide in patients with non-alcoholic steatohepatitis: results from the phase IIb LIRA-NAFLD study. J Hepatol. 2020;73(4):739-748. doi:10.1016/j.jhep.2020.05.015
- Sanyal A, Charles ED, Neuschwander-Tetri BA, et al. Pegbelfermin (BMS-986036), a PEGylated fibroblast growth factor 21 analogue, in patients with non-alcoholic steatohepatitis: a randomised, double-blind, placebo-controlled, phase 2a trial. Lancet. 2019;392(10165):2705-2717. doi:10.1016/S0140-6736(18)31785-9
- Ratziu V, Harrison SA, Francque S, et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor-α and -δ, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150(5):1147-1159.e5. doi:10.1053/j.gastro.2016.01.038
These references provide a comprehensive overview of the current evidence and future directions regarding the use of semaglutide in the treatment of non-alcoholic fatty liver disease (NAFLD), offering valuable insights into its potential as a therapeutic option for this increasingly prevalent hepatic disorder.
Questions and Answers: Semaglutide and Non-alcoholic fatty liver disease (NAFLD)
Semaglutide has shown promising results in the treatment of NAFLD, particularly in terms of reducing liver fat content and improving liver enzyme levels. Clinical studies have demonstrated that Semaglutide can significantly decrease the amount of fat in the liver, which is a key factor in the progression of NAFLD. Moreover, it helps in improving metabolic parameters like blood sugar control and body weight, which are closely linked to liver health in NAFLD patients. However, the effectiveness can vary based on individual patient factors, including the stage of NAFLD, co-existing medical conditions, and adherence to treatment and lifestyle modifications.
While Semaglutide is a promising treatment option, it may not be suitable for all NAFLD patients. Its use should be considered based on individual health profiles, including the presence of comorbidities such as type 2 diabetes, the severity of liver disease, and potential contraindications. Patients with a history of medullary thyroid carcinoma, Multiple Endocrine Neoplasia syndrome type 2, or pancreatitis should use Semaglutide with caution. It is essential for healthcare providers to evaluate each patient’s medical history and current health status before prescribing Semaglutide.
Common side effects of Semaglutide include gastrointestinal symptoms like nausea, vomiting, diarrhea, and constipation. These are usually mild to moderate and tend to decrease over time. Other potential side effects include a risk of hypoglycemia (especially when used with other diabetes medications), pancreatitis, allergic reactions, renal impairment, and an increase in heart rate. Patients should be closely monitored for these side effects, and any concerning symptoms should be promptly addressed.
While weight loss is a common and desired effect of Semaglutide, it is not guaranteed for every patient. The extent of weight loss varies among individuals, and it depends on various factors, including dosage, individual metabolism, lifestyle factors, and adherence to the treatment regimen. In addition to Semaglutide, implementing dietary changes and increasing physical activity are crucial for achieving significant weight loss.
The timeframe for seeing improvements in NAFLD with Semaglutide varies. Some patients may notice changes in their liver enzyme levels and weight within a few months, while significant improvements in liver fat content and fibrosis might take longer. Continuous monitoring through liver function tests, imaging studies, and assessments of metabolic health is essential to evaluate the effectiveness of the treatment over time.
Currently, there is no cure for NAFLD, but Semaglutide can significantly improve the condition. It helps in reducing liver fat, improving liver enzymes, and potentially slowing down or reversing liver fibrosis. However, NAFLD management typically requires a lifelong commitment to healthy lifestyle choices alongside medication. Semaglutide can be a valuable part of a comprehensive treatment plan that includes diet, exercise, and regular medical monitoring.
Yes, lifestyle modifications are a critical component of NAFLD management, even when taking Semaglutide. A healthy diet, regular physical activity, avoiding alcohol, and maintaining a healthy weight are essential. These lifestyle changes complement the effects of Semaglutide and are crucial for achieving the best outcomes in NAFLD treatment.
Semaglutide has been shown to be safe for long-term use in clinical trials, but its long-term effects specifically in NAFLD patients are still being studied. Ongoing research is focused on understanding the long-term safety and efficacy of Semaglutide in the management of NAFLD. Patients using Semaglutide should be under regular medical supervision to monitor for any potential side effects or complications.
Semaglutide may be used in combination with other medications, but this should be done under the guidance of a healthcare provider. The combination of drugs should be carefully selected based on the patient’s overall health, the presence of co-existing conditions, and the potential for drug interactions. In some cases, combining Semaglutide with other treatments targeting different aspects of NAFLD can enhance overall treatment efficacy.
If Semaglutide is discontinued, its beneficial effects on liver fat, liver enzymes, and metabolic health may diminish over time. It is important to discuss any decision to stop Semaglutide with a healthcare provider, as a comprehensive plan for managing NAFLD should be maintained. This might include continuing with lifestyle modifications and possibly introducing other treatments.

Dr. Jay Flottman
Dr. Jay Flottmann is a physician in Panama City, FL. He received his medical degree from University of Texas Medical Branch and has been in practice 21 years. He is experienced in military medicine, an FAA medical examiner, human performance expert, and fighter pilot.
Professionally, I am a medical doctor (M.D. from the University of Texas Medical Branch at Galveston), a fighter pilot (United States Air Force trained – F-15C/F-22/AT-38C), and entrepreneur.
