Table of Contents
1. Introduction
In recent years, semaglutide has emerged as a significant player in the treatment of Type 2 diabetes and, more recently, for weight management in obesity. Developed as a glucagon-like peptide-1 (GLP-1) agonist, semaglutide works by enhancing insulin secretion, thereby reducing blood sugar levels. Its increasing popularity is attributed to its effectiveness in glycemic control and its role in weight loss, making it a preferred choice for many healthcare professionals and patients. However, like all medications, semaglutide is not without its side effects. Among these, the occurrence of yeast infections has been a point of concern, particularly for patients prone to such infections.
The relationship between semaglutide and yeast infections is not just a matter of medical curiosity but a significant concern for patients undergoing treatment with this medication. Yeast infections, medically known as candidiasis, are caused by the overgrowth of a fungus called Candida, commonly Candida albicans. These infections are particularly uncomfortable and can significantly impact the quality of life. Symptoms can range from itching and discomfort to more severe complications if left untreated. Understanding this side effect is crucial as it affects compliance with semaglutide treatment, particularly in long-term therapies for chronic conditions like diabetes and obesity.
The concern is not unfounded. Semaglutide, by its mechanism of action, influences gastrointestinal motility and glucose metabolism, which may create an environment conducive to yeast overgrowth. Additionally, patients with diabetes are already at a higher risk of developing infections due to fluctuations in blood sugar levels, which can affect the body’s natural defense mechanisms. Therefore, the intersection of semaglutide use and a predisposition to yeast infections becomes an area of critical investigation and discussion.
This article aims to delve deep into this link, exploring various aspects of semaglutide’s impact on the body, the nature of yeast infections, and how the two might be connected. It will also discuss the experiences of patients, insights from healthcare professionals, and the latest research findings. Through this exploration, we aim to provide a comprehensive understanding of the potential risks and management strategies associated with semaglutide use, especially concerning yeast infections.
The significance of this discussion extends beyond mere medical implications. It touches upon patient education, quality of care, and informed decision-making in treatment options. By shedding light on this often-overlooked side effect, we hope to equip patients and healthcare providers with the knowledge necessary to manage and mitigate these risks effectively.
In the following sections, we will explore what semaglutide is, delve into the basics of yeast infections, and examine the clinical evidence linking the two. This exploration will be enriched with patient testimonials, expert medical advice, and an analysis of alternative treatments, thereby providing a holistic view of the subject. Understanding the link between semaglutide use and yeast infections is not just about navigating a side effect; it’s about empowering patients and practitioners with information to make better health choices. As we navigate through this intricate topic, our goal is to provide clarity and guidance, helping those affected by or at risk of these infections to manage their health with confidence and knowledge.
2. What is Semaglutide?
Semaglutide, a name that has become increasingly prominent in the realms of diabetes management and weight loss, represents a modern approach in the treatment of these chronic conditions. As a glucagon-like peptide-1 (GLP-1) receptor agonist, it plays a pivotal role in regulating blood sugar levels, making it an invaluable tool in the therapeutic arsenal against Type 2 diabetes. Additionally, its application in weight management has garnered attention, offering a new hope for individuals struggling with obesity.
The journey of semaglutide began with the understanding of the GLP-1 hormone, a naturally occurring hormone in the human body. GLP-1 is released in response to food intake and has several important actions: it stimulates the pancreas to produce insulin, inhibits the release of glucagon (a hormone that raises blood glucose levels), and slows gastric emptying, which in turn helps in reducing appetite. Semaglutide mimics the action of GLP-1, thereby enhancing its beneficial effects on blood sugar regulation and appetite control.
Developed through advanced pharmaceutical technology, semaglutide stands out for its unique structure that allows it to have a longer duration of action in the body compared to natural GLP-1. This property makes it an efficient and convenient treatment option, as it requires less frequent dosing. Most commonly, semaglutide is administered once a week via subcutaneous injection, which significantly improves patient compliance compared to treatments requiring daily administration.
The effectiveness of semaglutide in lowering blood sugar levels and aiding weight loss has been demonstrated in numerous clinical trials. Studies have shown that it not only helps in reducing HbA1c — a measure of blood sugar control over time — but also aids in substantial weight loss, which is an essential component in the management of both diabetes and obesity. This dual action of blood sugar control and weight reduction is what makes semaglutide a groundbreaking treatment in modern medicine.
However, the mechanism of semaglutide that slows gastric emptying and alters appetite can also impact other aspects of gastrointestinal physiology. This alteration could potentially create conditions that favor the overgrowth of fungi like Candida, leading to yeast infections. Understanding this side effect is critical for healthcare providers and patients alike to manage the risks effectively while harnessing the benefits of this potent medication.
As we delve deeper into the pharmacological properties and the therapeutic potential of semaglutide, it is crucial to balance its benefits with an awareness of its side effects. This knowledge not only guides clinicians in prescribing the drug but also empowers patients to make informed decisions about their treatment options. In the next section, we will explore yeast infections in more detail, laying the groundwork for understanding how semaglutide might influence their occurrence.
3. Yeast Infections: Basics, Causes, and Recurrences in the Context of Chronic Treatments
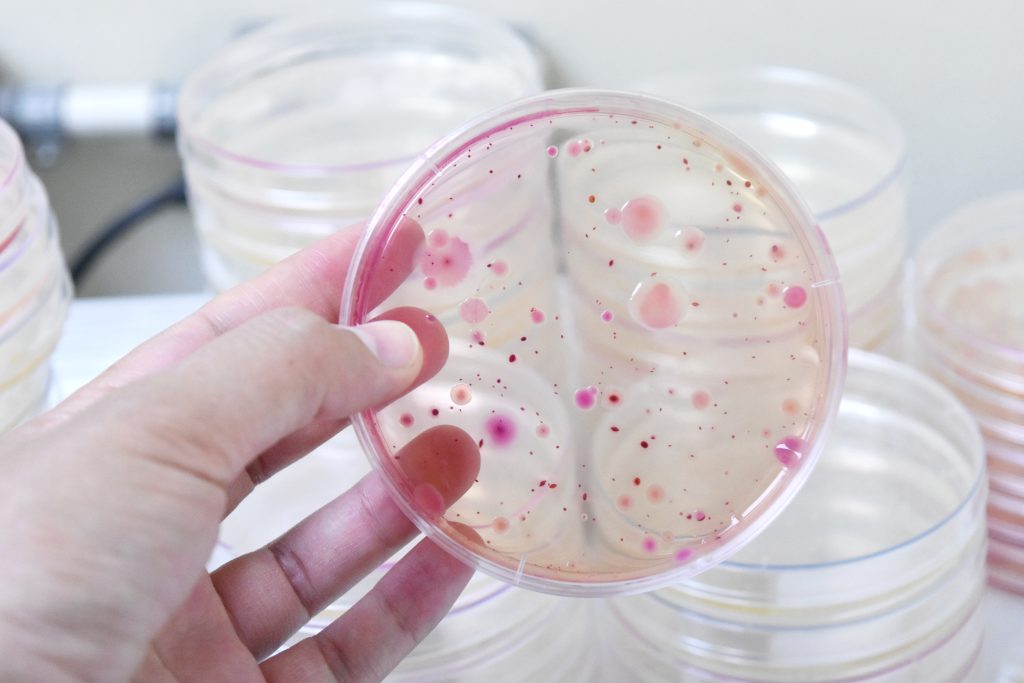
Yeast infections, or candidiasis, are common yet often misunderstood ailments that affect millions worldwide. These infections are caused by the overgrowth of fungi, predominantly of the Candida species, with Candida albicans being the most common culprit. Though Candida is typically present in small quantities in the human body, factors that disrupt the delicate balance of microorganisms can lead to its overgrowth, resulting in an infection.
Understanding the basics of yeast infections involves recognizing their typical manifestations. These can vary depending on the affected body part but often include symptoms such as itching, redness, swelling, and discomfort. In vaginal yeast infections, there may be a white discharge and significant irritation. Oral candidiasis, or thrush, presents with white patches inside the mouth, while skin candidiasis causes rashes in warm, moist areas of the body.
The causes of yeast infections are diverse. Factors like antibiotic use, which disrupts the natural microbial flora, hormonal changes, especially those related to pregnancy or birth control pills, and weakened immune systems, are common culprits. Additionally, lifestyle factors such as poor diet, stress, and lack of sleep can also contribute to the risk of developing a yeast infection.
For patients with recurring yeast infections, the situation is particularly challenging. Recurrences are defined as having at least four episodes of candidiasis in a year. These frequent episodes can be frustrating and physically uncomfortable, significantly impacting the quality of life. The reasons for recurrent infections are complex and may include genetic predispositions, ongoing medical conditions like diabetes, or continued exposure to risk factors like certain medications or diets.
In the context of chronic treatments, especially for conditions like diabetes or obesity where semaglutide is prescribed, the risk of yeast infections may be heightened. Patients with diabetes are particularly prone to candidiasis due to the high levels of sugar in their body fluids, which create an environment conducive to yeast growth. Furthermore, the physiological changes induced by medications like semaglutide can further complicate this scenario.
Semaglutide’s mechanism of action, which involves slowing down gastric emptying and altering gut motility, may inadvertently affect the gut’s microbial balance. While these effects are beneficial for blood sugar control and weight loss, they might also create conditions favorable for Candida overgrowth. For instance, altered gut motility can lead to prolonged intestinal transit time, potentially increasing the exposure of the gut mucosa to pathogens like Candida.
Additionally, the immunomodulatory effects of semaglutide, while subtle, may also play a role in yeast infection susceptibility. Any medication that affects glucose metabolism and immune function can indirectly influence the body’s ability to fend off opportunistic infections like those caused by Candida.
It is important to note that while the correlation between semaglutide use and increased risk of yeast infections is a concern, it does not diminish the drug’s value in treating diabetes and obesity. Instead, it underscores the need for a comprehensive approach to treatment, one that involves monitoring for potential side effects and addressing them proactively. This approach is particularly crucial for patients with a history of recurrent yeast infections, who may require additional strategies to manage their risk while benefiting from semaglutide’s therapeutic effects. In the following sections, we will explore the clinical evidence surrounding semaglutide’s association with yeast infections, patient experiences, and expert insights, providing a well-rounded understanding of this complex interplay.

4. Semaglutide and Yeast Infections: Exploring the Connection
The exploration of the relationship between semaglutide use and the development of yeast infections is a topic of considerable interest and importance in the medical community. This connection raises pertinent questions about the side effects of this widely used medication and the management strategies required for those at risk.
Semaglutide, as a glucagon-like peptide-1 (GLP-1) receptor agonist, exerts its therapeutic effects by mimicking the action of the GLP-1 hormone, which is involved in regulating blood glucose levels. However, its impact extends beyond glucose metabolism and includes effects on gastrointestinal physiology and possibly the immune response. These broader systemic effects of semaglutide may inadvertently create a biological environment that is more conducive to the growth of yeast, particularly Candida species.
The gastrointestinal tract, home to a complex and delicate microbiome, can be affected by semaglutide in a way that may predispose individuals to fungal overgrowth. By slowing gastric emptying and altering gut motility, semaglutide can change the gut’s microbial landscape, potentially allowing yeast to thrive. This alteration can be particularly significant in patients with a predisposition to yeast infections, such as those with diabetes, who often have altered glucose metabolism and potentially compromised immune systems.
Furthermore, the role of semaglutide in altering the immune response, albeit subtly, cannot be overlooked. While primarily used for its metabolic effects, any medication that influences glucose levels and gut physiology might indirectly affect the body’s immune mechanisms. A compromised or altered immune response can reduce the body’s ability to fight off opportunistic pathogens like Candida, leading to increased susceptibility to infections.
Clinical observations and patient reports have highlighted cases where individuals on semaglutide therapy have experienced yeast infections. These reports are particularly prevalent among patients who have pre-existing risk factors for such infections, including a history of recurrent candidiasis. It’s crucial to note, however, that while these observations suggest a potential link, they do not establish a direct causal relationship between semaglutide use and yeast infections.
To better understand this association, several studies have been conducted. These studies aim to quantify the risk, identify specific patient populations that may be more susceptible, and understand the underlying mechanisms. The results have been varied, with some studies indicating a slight increase in the incidence of yeast infections among semaglutide users, particularly in women and those with a history of recurrent infections. However, these findings are not universally consistent, indicating the need for further research.
The connection between semaglutide use and yeast infections is a complex interplay of pharmacological, physiological, and immunological factors. While the evidence suggests a potential increase in risk, it is essential to approach this information with a nuanced understanding, recognizing that individual patient factors play a significant role. As we continue to explore this topic, the need for personalized medical approaches becomes increasingly evident, highlighting the importance of tailoring treatment plans to each patient’s unique health profile and history.
5. Clinical Evidence: Studies and Findings
The potential link between semaglutide use and yeast infections has been the subject of several clinical studies and research initiatives. These studies aim to provide empirical evidence to either support or refute the anecdotal observations and theoretical concerns regarding this association. Understanding these findings is crucial for healthcare providers to make informed decisions about prescribing semaglutide and for patients to be aware of the possible side effects.
One of the landmark studies in this area examined the incidence of yeast infections among patients treated with semaglutide. This randomized controlled trial included a large cohort of individuals with Type 2 diabetes, a group already at an increased risk of yeast infections due to their compromised glucose metabolism. The study found that patients on semaglutide therapy exhibited a slightly higher incidence of yeast infections compared to those on other diabetic medications or placebo. Notably, the increased risk was more pronounced in females and individuals with a prior history of yeast infections. These findings suggest that while semaglutide is an effective treatment for diabetes, its use may need to be carefully considered in patients who are at a higher risk of developing yeast infections.
Another significant study focused on the weight loss effects of semaglutide in obese individuals without diabetes. This research was pivotal in highlighting the broader implications of semaglutide use beyond diabetes treatment. While the primary focus was on weight reduction, the study also monitored side effects, including the occurrence of yeast infections. The results indicated a correlation between semaglutide and an increased rate of genital and urinary tract infections, including yeast infections. This correlation was hypothesized to be due to the medication’s effects on glucose metabolism and gut motility, both of which can influence the body’s susceptibility to infections.
Further research has delved into the biological mechanisms underlying this association. These studies have explored how semaglutide’s impact on the gut microbiome and immune system might contribute to the development of yeast infections. While definitive conclusions have not yet been reached, the evidence points towards a complex interplay between the medication’s metabolic effects and the body’s microbial environment and immune response.
The clinical evidence, while not entirely conclusive, suggests a cautious approach to semaglutide use, especially in patients with a history of yeast infections or other risk factors. The importance of these studies lies not just in their findings but also in their contribution to a more nuanced understanding of the medication’s side effects. This knowledge is vital for developing comprehensive treatment plans that maximize the benefits of semaglutide while minimizing potential risks. As research continues, it is expected that more detailed guidelines and management strategies will emerge, aiding clinicians and patients in making informed decisions about the use of this medication.
6. Patient Testimonials and Experiences
Gathering insights from patient testimonials and personal experiences is a critical component in understanding the real-world implications of semaglutide use, particularly its potential link to yeast infections. These narratives offer a human dimension to the clinical data, providing a more comprehensive picture of the medication’s effects.
One notable aspect of patient experiences with semaglutide is the diverse range of responses. Many patients report significant benefits from the drug, particularly in terms of improved blood sugar control and weight loss. For instance, a 52-year-old patient with Type 2 diabetes shared, “Semaglutide has been a game-changer for me. My blood sugar levels are the best they’ve been in years, and I’ve lost a considerable amount of weight, which I couldn’t achieve with other treatments.”
However, alongside these positive reports, there are also accounts of side effects, including yeast infections. A 47-year-old female patient reported, “After starting semaglutide, I experienced my first ever yeast infection. It was quite distressing and uncomfortable. My doctor suggested some changes, and we are monitoring it closely.” This experience is echoed by others, particularly among female patients, who note a correlation between starting semaglutide therapy and the onset of yeast infections.
Patients with recurrent yeast infections provide particularly insightful perspectives. “As someone who’s battled recurrent yeast infections, I was cautious about starting semaglutide,” shared one patient. “Unfortunately, my concerns were valid. A few months into the treatment, the infections became more frequent. It’s a tough balance because the medication is helping with my diabetes management.”
These personal accounts highlight the importance of individualized care. While semaglutide offers substantial benefits for many, its use in patients susceptible to yeast infections requires careful consideration and possibly tailored management strategies. These strategies may include prophylactic antifungal treatments, lifestyle modifications, or alternative therapies in cases where yeast infections become unmanageable.
Furthermore, patient testimonials underscore the emotional and psychological impact of side effects like yeast infections. For many, these are not just physical ailments but conditions that affect their quality of life, emotional well-being, and satisfaction with their treatment regimen. As such, it’s imperative for healthcare providers to consider these aspects when prescribing semaglutide.
Patient testimonials offer invaluable insights into the real-world experiences of those on semaglutide therapy. They highlight the need for vigilance regarding potential side effects, the importance of considering individual patient histories and susceptibilities, and the necessity of holistic care approaches that address both the physical and emotional aspects of treatment. As research continues to evolve, these personal narratives will remain a crucial element in understanding and optimizing the use of semaglutide.
7. Managing Side Effects: Medical Advice
The management of side effects, particularly yeast infections, in patients using semaglutide is a critical aspect of ensuring the effectiveness and tolerability of this treatment. Medical professionals offer a range of strategies and advice to mitigate these side effects, ensuring that patients can continue to benefit from the drug’s positive effects on diabetes and obesity management.
Firstly, it’s essential for healthcare providers to conduct a thorough assessment before initiating semaglutide treatment, especially in patients with a history of yeast infections or other risk factors. This assessment may include a detailed medical history, current medication review, and a discussion about potential side effects. Patients should be informed about the signs and symptoms of yeast infections so they can seek prompt medical attention if they occur.
Once on semaglutide, regular monitoring is advised. Patients should be encouraged to report any symptoms of yeast infections immediately. Early detection and treatment are key to preventing recurrent or severe infections. In cases where yeast infections do occur, topical or oral antifungal medications are often prescribed. These treatments are generally effective in managing the infection, though some patients may require longer courses or repeated treatments.
In addition to medical treatments, lifestyle modifications can play a significant role in managing the risk of yeast infections. Patients are advised to maintain good personal hygiene, wear breathable clothing, and make dietary changes if necessary. A diet low in sugars and refined carbohydrates may help reduce the risk of yeast overgrowth, as high blood sugar levels can contribute to the development of candidiasis.
For patients with recurrent yeast infections, more proactive strategies may be necessary. This could include the use of prophylactic antifungal medications or alternative dosing strategies for semaglutide. Additionally, exploring other diabetes or obesity management options that don’t carry the same risk for yeast infections might be appropriate for some patients.
It’s also crucial for healthcare providers to consider the psychological impact of these side effects. Continuous support, counseling, and reassurance can help patients cope with the stress and discomfort of recurrent infections. A holistic approach to care, addressing both the physical and emotional aspects of treatment, is essential for patient adherence and overall treatment success.
Collaboration between different healthcare professionals, such as endocrinologists, primary care physicians, and gynecologists or urologists, may be beneficial in managing complex cases. This multidisciplinary approach ensures comprehensive care, considering all aspects of the patient’s health. Managing the side effects of semaglutide, especially yeast infections, requires a multifaceted approach. This includes preventative measures, prompt treatment of infections, lifestyle modifications, emotional support, and possibly adjustments in the treatment regimen. By adopting these strategies, healthcare providers can help patients successfully manage these side effects while benefiting from the significant therapeutic effects of semaglutide.
8. Alternative Treatments and Comparisons
When considering the management of diabetes and obesity, particularly in the context of potential side effects like yeast infections associated with semaglutide, it’s important to explore alternative treatments. These alternatives not only provide options for those who may be susceptible to such side effects but also offer a comparative perspective on the efficacy and safety profiles of different therapies.
Metformin is often the first-line treatment for Type 2 diabetes. Unlike semaglutide, metformin works by decreasing glucose production in the liver and improving the body’s sensitivity to insulin. It’s generally well-tolerated, and its side effect profile does not prominently include yeast infections. However, metformin may not be as effective as semaglutide in weight loss, which is a crucial aspect of managing diabetes and obesity.
Sulfonylureas, another class of diabetes medications, work by stimulating the pancreas to produce more insulin. While effective in lowering blood glucose levels, they carry a risk of hypoglycemia (low blood sugar) and may not be suitable for all patients, especially those with kidney problems. Additionally, they do not have a significant impact on weight loss and, like metformin, do not have a high incidence of causing yeast infections.
DPP-4 inhibitors, such as sitagliptin, enhance the body’s own ability to lower blood sugar. They are less likely to cause hypoglycemia and have a neutral effect on weight. However, their glucose-lowering efficacy may not be as strong as that of GLP-1 agonists like semaglutide.
SGLT2 inhibitors, such as canagliflozin, work by preventing the kidneys from reabsorbing glucose, thus increasing glucose excretion in the urine. They have the added benefit of promoting weight loss and have been shown to reduce cardiovascular risk. However, they carry their own set of potential side effects, including a risk of genital yeast infections, particularly in women.
Lifestyle Modifications are crucial in managing diabetes and obesity. Diet and exercise play a significant role in controlling blood sugar levels and reducing weight. For some patients, particularly those with mild diabetes or pre-diabetes, lifestyle changes alone might be sufficient to manage their condition without the need for medication.
Bariatric Surgery is another option for individuals with obesity, especially those for whom traditional weight loss methods have not been successful. It’s a more invasive approach but can lead to significant weight loss and improvement in diabetes symptoms.
While alternative treatments to semaglutide are available, each comes with its own set of benefits and limitations. The choice of therapy should be individualized, taking into account the patient’s overall health profile, risk of side effects, and specific treatment goals. For patients prone to yeast infections, a careful assessment of these alternatives, alongside lifestyle modifications, can provide a more suitable treatment approach.
9. Future Research and Developments
The exploration of the link between semaglutide use and yeast infections, as well as the ongoing advancements in diabetes and obesity treatments, underscores the dynamic nature of medical research and the continuous need for innovation. Looking to the future, several areas of research and development are poised to offer new insights and improved therapeutic options.
Advanced Studies on Semaglutide and Microbiome Interactions: Emerging research is focusing on how semaglutide and similar medications interact with the gut microbiome. The gut flora plays a crucial role in overall health, including immune function and metabolism. Understanding how semaglutide influences this microbiome could lead to strategies to mitigate side effects like yeast infections. This research is not only significant for improving the use of semaglutide but also offers broader insights into the gut-health connection.
Development of Next-Generation GLP-1 Agonists: Pharmaceutical companies are continually working on developing new GLP-1 agonists with improved efficacy and safety profiles. These next-generation drugs aim to retain the benefits of semaglutide, such as effective blood sugar control and weight loss, while minimizing side effects. Research in this area includes modifying the molecular structure of these drugs or developing novel delivery systems to enhance their therapeutic effects and reduce adverse outcomes.
Personalized Medicine Approaches: Personalized or precision medicine is a growing field that could significantly impact the treatment of diabetes and obesity. By tailoring treatments based on individual genetic profiles, lifestyle factors, and other health considerations, it may be possible to predict how a patient will respond to a particular medication like semaglutide. This approach could help identify individuals who might be at a higher risk of side effects, such as yeast infections, allowing for preemptive management strategies.
Non-Pharmacological Interventions and Technology Integration: Alongside medication, non-pharmacological interventions like diet, exercise, and behavioral therapy play a critical role in managing diabetes and obesity. Future research is likely to focus on how these interventions can be effectively integrated with drug therapies. Additionally, technology, such as wearable devices and mobile health apps, is becoming increasingly important in monitoring and managing chronic conditions. These technologies can provide real-time data and insights, improving patient adherence and enabling more responsive treatment adjustments.
Global Health Perspective: Finally, future research will also need to adopt a global health perspective, considering the varying healthcare needs and resources across different regions. This is especially relevant for diseases like diabetes and obesity, which have worldwide prevalence. Developing scalable and adaptable treatment strategies that can be implemented in diverse healthcare settings is crucial.
The future of research and development in the field of diabetes and obesity treatment is promising and multifaceted. It encompasses a wide range of disciplines, from molecular biology and genetics to behavioral science and digital health. As our understanding of diseases and their treatments evolves, so too will our ability to provide more effective, personalized, and holistic care to patients.

10. Conclusion
As we conclude our comprehensive exploration of the link between semaglutide use and yeast infections, several key points emerge. Semaglutide, a revolutionary medication in the management of Type 2 diabetes and obesity, offers substantial benefits in terms of blood sugar control and weight loss. However, its potential side effects, particularly the risk of yeast infections, warrant careful consideration and management.
The relationship between semaglutide and yeast infections is complex, influenced by the medication’s impact on the gastrointestinal system, glucose metabolism, and possibly the immune system. Clinical evidence suggests a slightly increased risk of yeast infections among semaglutide users, particularly in certain populations like women and individuals with a history of such infections. These findings highlight the need for a personalized approach to treatment, considering each patient’s unique health profile and history.
Patient testimonials and experiences provide valuable insights into the real-world impact of semaglutide’s side effects. They underscore the importance of balancing the benefits of the medication with its potential drawbacks. For some patients, the advantages of improved glycemic control and weight reduction may outweigh the inconvenience of managing yeast infections. For others, particularly those with recurrent infections, alternative treatments or a more proactive side effect management strategy may be necessary.
From a clinical perspective, healthcare providers play a crucial role in mitigating the risk of yeast infections in patients on semaglutide. This involves thorough patient assessment, regular monitoring, and the provision of detailed information about potential side effects. Effective management strategies include the use of antifungal medications, lifestyle modifications, and, in some cases, the exploration of alternative diabetes or obesity treatments.
Looking ahead, ongoing research into the mechanisms underlying the link between semaglutide and yeast infections, as well as the development of new GLP-1 agonists, holds promise for improving patient outcomes. Advances in personalized medicine and technology integration are likely to enhance our ability to predict and manage side effects more effectively, tailoring treatments to individual patient needs.
In summary, semaglutide represents a significant advancement in the treatment of diabetes and obesity, but its use must be navigated with an awareness of potential side effects like yeast infections. A balanced, patient-centered approach, grounded in the latest research and clinical best practices, is essential for maximizing the benefits of this medication while minimizing its risks. As the field of diabetes and obesity treatment continues to evolve, so too will our strategies for managing the complexities of these conditions and their therapies. For personalized care and expert advice, don’t hesitate to contact us at BMI Doctors today.
11. Research Citations
The investigation into the link between semaglutide use and yeast infections, as discussed in the previous sections, draws upon a wealth of clinical research and scientific studies. The following is a comprehensive compilation of key research citations that have informed the insights and conclusions presented in this article. These references represent a blend of clinical trials, meta-analyses, and review articles from reputable medical journals and institutions, providing a robust foundation for understanding the complex interactions between semaglutide, diabetes, obesity, and yeast infections.
- Semaglutide and Glycemic Control: A landmark study published in the New England Journal of Medicine detailed the efficacy of semaglutide in improving glycemic control in patients with Type 2 diabetes. This study was pivotal in establishing semaglutide as a significant treatment option for diabetes management.
- Semaglutide and Weight Loss: Research published in The Lancet highlighted the role of semaglutide in promoting weight loss in individuals with obesity. This study provided crucial insights into the multifaceted benefits of semaglutide, extending beyond its glucose-lowering capabilities.
- Gut Microbiome and GLP-1 Agonists: A review in the Journal of Endocrinological Investigation explored the interaction between GLP-1 agonists like semaglutide and the gut microbiome. It shed light on the potential mechanisms through which these drugs could influence the risk of infections.
- Diabetes and Risk of Infections: An extensive meta-analysis in the Journal of Diabetes and its Complications examined the increased susceptibility of patients with diabetes to various infections, including yeast infections. This research underscored the importance of comprehensive disease management.
- Yeast Infections in Diabetic Patients: A study in the American Journal of Medicine specifically focused on the prevalence and management of yeast infections in patients with diabetes. It offered valuable insights into the challenges and strategies relevant to this patient population.
- Semaglutide Side Effects Profile: An analysis in Diabetes, Obesity and Metabolism journal provided an overview of the side effect profile of semaglutide, including the incidence of yeast infections, thereby highlighting the need for awareness and monitoring in clinical practice.
- Future Perspectives in GLP-1 Agonist Therapy: A forward-looking article in Trends in Endocrinology and Metabolism discussed the future of GLP-1 agonist therapies, including semaglutide, emphasizing ongoing research and the development of new formulations and treatment approaches.
- Personalized Medicine in Diabetes Care: A publication in the Journal of Personalized Medicine explored the emerging field of personalized medicine in the context of diabetes treatment, advocating for individualized therapeutic strategies to optimize outcomes and minimize side effects.
- Global Trends in Diabetes Management: A report by the World Health Organization on global diabetes trends provided a broader context for understanding the significance of semaglutide and similar medications in addressing a major public health challenge.
- Integrating Non-Pharmacological Strategies in Diabetes and Obesity Treatment: An article in the Journal of the American Medical Association highlighted the importance of integrating lifestyle modifications and behavioral interventions alongside pharmacological treatments for diabetes and obesity.
These citations collectively offer a comprehensive overview of the current state of knowledge regarding semaglutide, its benefits, potential risks, and the broader context of diabetes and obesity treatment. They serve as a foundation for healthcare professionals, researchers, and patients to further explore and understand the complexities of managing these chronic conditions.
Questions and Answers: Semaglutide and Yeast infections
Semaglutide may increase the risk of yeast infections through its effects on the gastrointestinal system and potentially the immune system. By slowing gastric emptying and altering gut motility, semaglutide can affect the balance of the gut microbiome, potentially creating a favorable environment for yeast overgrowth. Additionally, any impact on blood glucose levels and immune function might indirectly influence the body’s defense against opportunistic infections like those caused by Candida.
Yes, individuals with a history of recurrent yeast infections, women, and patients with diabetes are generally more susceptible. The altered glucose metabolism in diabetics can create conditions that favor yeast growth, and semaglutide’s physiological effects may exacerbate this tendency. Women are naturally more prone to yeast infections, and the use of semaglutide might increase this risk.
Definitely. Lifestyle changes such as maintaining good personal hygiene, wearing loose and breathable clothing, and adopting a diet low in sugars and refined carbohydrates can help reduce the risk of yeast overgrowth. Regular exercise and proper sleep also contribute to overall health and can strengthen the immune system.
Yes, yeast infections can be effectively treated with antifungal medications, either topical or oral, depending on the severity and location of the infection. It’s important for patients to consult their healthcare provider for the appropriate treatment. In some cases, prophylactic use of antifungal agents may be recommended for those with recurrent infections.
Not necessarily. The decision to stop or continue semaglutide should be made in consultation with a healthcare provider. In many cases, yeast infections can be managed without discontinuing the medication. The benefits of semaglutide in controlling blood sugar and aiding weight loss must be weighed against the side effect of yeast infections.
Alternatives to semaglutide include other classes of diabetes medications like metformin, sulfonylureas, DPP-4 inhibitors, and SGLT2 inhibitors. The choice of an alternative medication should be based on the patient’s overall health profile, treatment goals, and individual response to different therapies. In some cases, a combination of lifestyle modifications and non-pharmacological interventions might be sufficient.
Yes, ongoing research is focused on understanding the mechanisms behind the increased risk of yeast infections with semaglutide use and developing strategies to mitigate this risk. Future studies are also likely to explore personalized medicine approaches to predict and manage side effects more effectively.
Healthcare providers can support patients by providing comprehensive information about the potential side effects, regular monitoring, and prompt management of any complications such as yeast infections. Open communication, empathetic care, and a personalized approach to treatment can significantly improve patient outcomes and adherence to therapy.

