Table of Contents
Introduction
Semaglutide has gained significant attention in recent years as a medication used to treat type 2 diabetes and support weight loss. It is part of a class of drugs called GLP-1 receptor agonists, which help regulate blood sugar levels and reduce appetite. Many people have benefited from semaglutide, but as its use becomes more widespread, new questions are emerging about its effects on other areas of health. One surprising concern that has come up is whether semaglutide has any connection to varicose veins.
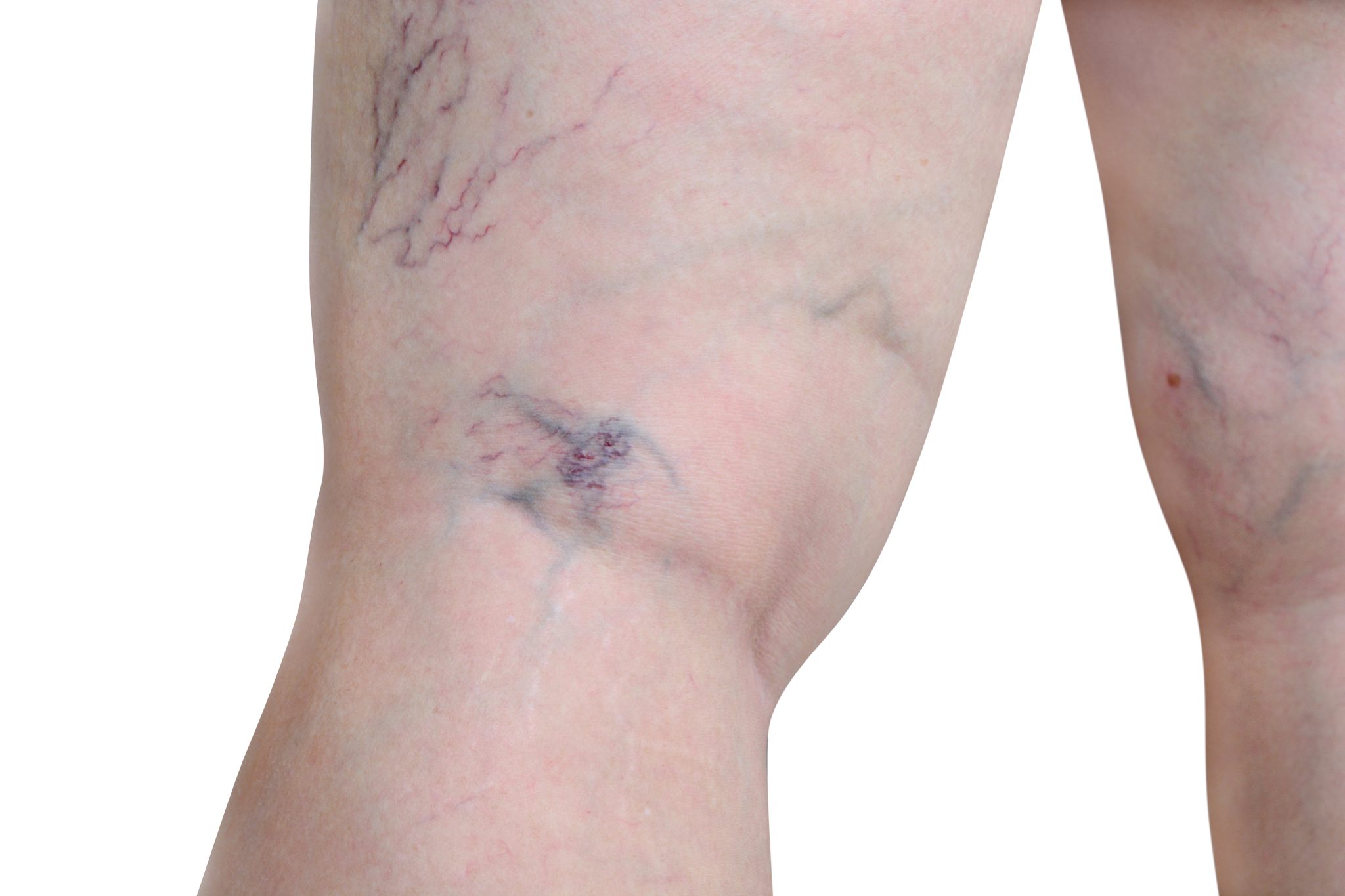
Varicose veins are swollen, twisted veins that appear just under the surface of the skin. They often develop in the legs and can cause pain, discomfort, and cosmetic concerns. While varicose veins are common, especially among older adults and people who spend long hours standing, they can sometimes be a sign of underlying circulation problems. Because semaglutide affects metabolism, weight, and possibly circulation, some people wonder if it has any impact on varicose veins—either making them worse or improving them.
Understanding the relationship between semaglutide and varicose veins is important for anyone who takes this medication or is considering it. People who already have varicose veins might worry that semaglutide could make their condition worse. Others may hope that the medication’s weight loss effects could help reduce pressure on their veins, potentially improving circulation. However, because semaglutide is still a relatively new drug, researchers are still studying its long-term effects on different parts of the body, including blood vessels.
This article explores whether semaglutide and varicose veins are connected in any way. It answers the most commonly asked questions on this topic and examines what current research and medical experts have to say. By the end of this article, you will have a clear understanding of whether semaglutide could impact your vein health and what steps you can take to maintain healthy circulation while using the medication.
What Is Semaglutide and How Does It Work?
Semaglutide is a medication that helps control blood sugar levels and manage weight. It belongs to a group of drugs called GLP-1 receptor agonists. GLP-1 stands for glucagon-like peptide-1, a natural hormone in the body that helps regulate blood sugar.
Doctors prescribe semaglutide to people with type 2 diabetes and those who need help with weight loss. The drug works by mimicking the effects of the GLP-1 hormone, which is produced in the intestines after eating. This hormone helps the body in three main ways:
- Slowing Down Digestion – It delays how quickly food moves from the stomach to the intestines, making a person feel full longer.
- Reducing Appetite – It affects areas of the brain that control hunger, helping people eat less.
- Regulating Blood Sugar – It helps the pancreas release insulin when blood sugar levels are high and reduces the release of another hormone called glucagon, which raises blood sugar.
How Semaglutide Works in the Body
After taking semaglutide, the medication binds to GLP-1 receptors in the pancreas, stomach, and brain. These receptors help control different body functions related to blood sugar and appetite.
- In the pancreas, it stimulates insulin release when blood sugar is high. Insulin is the hormone that moves sugar from the blood into cells for energy. If blood sugar is low, semaglutide does not trigger insulin, reducing the risk of hypoglycemia (low blood sugar).
- In the liver, it reduces the release of glucagon, which helps prevent extra sugar from entering the bloodstream. This keeps blood sugar levels stable.
- In the stomach, it slows digestion. When food stays in the stomach longer, a person feels full and eats less, leading to weight loss.
- In the brain, it reduces hunger signals. People taking semaglutide often report feeling less hungry and having fewer cravings for unhealthy foods.
Uses of Semaglutide
Semaglutide is approved by the U.S. Food and Drug Administration (FDA) for two main conditions:
- Type 2 Diabetes
- Sold under the brand name Ozempic, it helps lower blood sugar levels in people with type 2 diabetes. It is usually used along with diet and exercise and may be combined with other diabetes medications.
- Studies show that semaglutide not only lowers blood sugar but also reduces the risk of heart disease in people with diabetes.
- Weight Management
- Marketed as Wegovy, it is used to help people lose weight. Doctors prescribe it for adults with obesity (BMI 30 or higher) or those who are overweight (BMI 27 or higher) with weight-related health problems like high blood pressure or high cholesterol.
- It is not a quick-fix weight loss drug. It works best when combined with a healthy diet and regular exercise.
Some doctors also prescribe semaglutide off-label for weight loss in people who do not meet the strict guidelines for Wegovy but may still benefit from it.
How Semaglutide Is Taken
Semaglutide is given as an injection under the skin, usually in the thigh, stomach, or upper arm. Most people take it once a week using a pre-filled pen. The dose starts low and is increased over time to help the body adjust and reduce side effects like nausea.
There is also an oral form of semaglutide called Rybelsus, which is taken as a pill once a day for type 2 diabetes. However, the pill form is less common than the injection.
Common Side Effects
Like all medications, semaglutide can cause side effects. The most common ones are related to digestion, including:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Bloating
These side effects usually improve as the body gets used to the medication. Eating smaller meals and avoiding greasy foods can help reduce stomach problems.
Less common but more serious side effects include:
- Pancreatitis (inflammation of the pancreas) – Symptoms include severe stomach pain, nausea, and vomiting.
- Gallbladder problems – Some people develop gallstones or gallbladder inflammation.
- Kidney problems – Dehydration from vomiting or diarrhea can affect kidney function.
Doctors monitor patients closely, especially when they first start semaglutide.
Benefits Beyond Diabetes and Weight Loss
Semaglutide has gained attention not just for blood sugar control and weight loss but also for its potential heart benefits. Studies show that it can:
- Lower the risk of heart attacks and strokes in people with diabetes.
- Reduce inflammation in blood vessels, improving overall circulation.
Because varicose veins are linked to poor circulation, some researchers wonder if semaglutide could have an impact on vein health. However, there is not enough research yet to confirm whether it helps or worsens varicose veins.
Semaglutide is changing the way doctors treat diabetes and obesity. Its effects on blood vessels, circulation, and vein health are still being studied. Understanding how it works is important for people who take the medication and want to be aware of any possible effects on their veins.
Understanding Varicose Veins: Causes and Risk Factors
Varicose veins are swollen, twisted veins that often appear just under the skin, usually on the legs. They can be blue, purple, or flesh-colored and may cause discomfort, pain, or a heavy feeling in the legs. While varicose veins are common, many people do not fully understand why they develop or what factors increase the risk of getting them.
How Do Varicose Veins Develop?
Veins are responsible for carrying blood back to the heart. To do this, they contain tiny one-way valves that prevent blood from flowing backward. In healthy veins, these valves open to let blood through and close to stop it from moving in the wrong direction.
Varicose veins form when these valves weaken or become damaged. Instead of blood moving smoothly toward the heart, some of it flows backward and pools in the veins. This extra blood puts pressure on the vein walls, making them stretch, twist, and bulge. Over time, the veins become enlarged and visible through the skin.
Common Causes of Varicose Veins
- Weak or Damaged Valves in the Veins
The most direct cause of varicose veins is valve failure. When the tiny valves in the veins stop working properly, blood can no longer flow efficiently. This causes it to collect in the veins, leading to swelling and distortion. Valve weakness can be caused by aging, injury, or excessive pressure on the veins over time.
- Poor Circulation
Blood circulation plays a key role in vein health. If circulation is poor, blood may move too slowly through the veins, increasing the chances of it pooling. Certain medical conditions, lack of physical activity, or long periods of sitting or standing can all contribute to sluggish circulation.
- Genetics and Family History
Varicose veins tend to run in families. If a parent or close relative has them, the chances of developing them increase. Genetic factors can influence the strength of vein walls and valves, making some people more prone to venous issues than others.
- Prolonged Standing or Sitting
Jobs that require long hours of standing, such as nursing, retail, or factory work, can put extra pressure on the veins in the legs. When a person stands for long periods, the veins must work harder to push blood upward against gravity. Over time, this added strain can weaken the vein valves.
Sitting for too long can also be a problem. When legs remain still for extended periods, circulation slows down, increasing the risk of blood pooling in the veins. This is why people who work at desks or travel frequently on long flights may experience vein-related issues.
- Obesity and Excess Weight
Carrying extra weight increases pressure on the veins, especially in the lower body. This added stress can make it harder for the veins to push blood back to the heart. Over time, this strain can weaken the vein walls and valves, leading to varicose veins.
- Pregnancy and Hormonal Changes
Pregnancy is a common time for varicose veins to develop. During pregnancy, the body produces more blood to support the growing baby. This extra volume puts pressure on the veins, particularly those in the legs.
Hormonal changes during pregnancy also play a role. The hormone progesterone, which helps relax muscles to prepare for childbirth, can also relax vein walls, making them more likely to stretch and swell. The weight of the baby pressing on the pelvic veins can further increase pressure, leading to varicose veins.
- Age and Aging Veins
As people age, the veins naturally lose elasticity, and the valves inside them may become weaker. This makes it easier for blood to pool and veins to stretch out. Varicose veins become more common with age, especially after 50.
- Lack of Exercise
Regular physical activity helps keep the veins healthy. Exercise, especially activities like walking, swimming, and cycling, helps blood circulate properly. It also strengthens the calf muscles, which act as a natural pump to push blood upward through the veins. A sedentary lifestyle can lead to poor circulation and increase the risk of developing varicose veins.
- History of Blood Clots or Vein Damage
Blood clots and past injuries to the veins can damage the valves, making it harder for them to function properly. When the valves are weakened, they may not close completely, allowing blood to flow backward and pool in the veins.
- Smoking and Alcohol Consumption
Smoking damages blood vessels and reduces circulation, which can increase the risk of varicose veins. Alcohol, when consumed in excess, can also affect blood pressure and circulation, leading to vein issues over time.
Why Are Varicose Veins Most Common in the Legs?
Varicose veins can develop anywhere in the body, but they are most common in the legs. This is because the veins in the legs have to work against gravity to push blood back to the heart. The added pressure from standing, walking, and carrying body weight makes these veins more vulnerable to valve failure and blood pooling.
In some cases, varicose veins can also appear in the pelvic area, especially during pregnancy. Hemorrhoids, which are swollen veins in the rectum, are another form of varicose veins caused by pressure and poor circulation.
Symptoms of Varicose Veins
Not all varicose veins cause pain, but they can lead to discomfort and other symptoms, including:
- Aching or heaviness in the legs, especially after standing for long periods.
- Swelling in the lower legs and ankles.
- Itching or burning sensation around the affected veins.
- Skin discoloration or thickening in severe cases.
- Cramping or restless legs, especially at night.
Complications of Untreated Varicose Veins
For some people, varicose veins are mainly a cosmetic concern. However, in more severe cases, they can lead to complications such as:
- Blood Clots (Deep Vein Thrombosis – DVT): If a clot forms in a deep vein, it can cause serious health issues, including a risk of pulmonary embolism.
- Venous Ulcers: Poor circulation can lead to slow-healing wounds, usually near the ankles.
- Bleeding: Varicose veins close to the skin’s surface may burst, causing minor or severe bleeding.
Varicose veins develop when vein valves weaken, allowing blood to pool in the veins. They are most commonly seen in the legs and can be caused by genetics, prolonged standing or sitting, obesity, pregnancy, and other factors that affect circulation. While they are often harmless, they can cause discomfort and lead to complications if left untreated. Understanding the causes and risk factors can help individuals take steps to protect their vein health and seek medical advice if needed.

Can Semaglutide Affect Blood Circulation and Vein Health?
Semaglutide is a medication that helps people manage their blood sugar levels and lose weight. It belongs to a class of drugs called GLP-1 receptor agonists. While semaglutide is mainly used for diabetes and weight loss, some people wonder if it affects blood circulation and vein health.
To understand this, it is important to look at how semaglutide works in the body. It changes the way the body handles insulin, blood sugar, and digestion. It also affects the cardiovascular system, which includes the heart and blood vessels.
How Semaglutide Affects the Cardiovascular System
Semaglutide influences blood circulation in several ways. One of its biggest effects is on blood pressure. Studies show that people who take semaglutide may have lower blood pressure over time. Lower blood pressure can reduce stress on veins, which might help with circulation.
Semaglutide also improves blood sugar control. High blood sugar levels can damage blood vessels over time, making them weak. By lowering blood sugar, semaglutide may help keep veins and arteries healthier.
Another way semaglutide impacts circulation is through weight loss. Many people who take semaglutide lose weight. Losing extra weight reduces pressure on veins, especially in the legs. This can improve blood flow and may prevent further damage to veins.
At the same time, semaglutide slows down digestion. This means food stays in the stomach longer, which affects how the body absorbs nutrients and fluids. Some people experience dehydration when using semaglutide, which can lead to thicker blood. If blood becomes too thick, it may not flow properly through veins, increasing the risk of circulation problems.
Does Semaglutide Affect Blood Vessels Directly?
Some medications directly affect blood vessels by making them wider or narrower. Semaglutide does not seem to work this way. Instead, it has indirect effects that may impact blood vessels over time.
One way it helps is by reducing inflammation in the body. Inflammation can damage the walls of blood vessels, making them weaker. Studies suggest that semaglutide lowers inflammation markers, which could help protect veins from damage.
However, semaglutide can also cause side effects that affect circulation. Some people experience dizziness, nausea, or dehydration. If a person becomes dehydrated, blood volume decreases, and veins may have trouble pushing blood back to the heart. This can lead to swelling, which is a common issue for people with varicose veins.
Can Semaglutide Improve Circulation for People with Varicose Veins?
For people with varicose veins, circulation is already a challenge. Varicose veins develop when the valves inside the veins stop working properly. This causes blood to pool in the legs, leading to swelling and discomfort.
Semaglutide may help improve circulation by reducing body weight and lowering blood pressure. With less pressure on the veins, blood may flow more easily back to the heart. Losing weight can also reduce swelling in the legs, which may improve symptoms of varicose veins.
Another possible benefit is better blood sugar control. People with diabetes or insulin resistance have a higher risk of vein problems. Since semaglutide helps manage blood sugar, it may reduce the risk of further vein damage.
Are There Risks to Vein Health While Taking Semaglutide?
Although semaglutide has many benefits, there are some risks to be aware of. Some people lose weight very quickly while taking semaglutide. Rapid weight loss can cause changes in circulation. When fat is lost too fast, the body may struggle to adjust, which can sometimes lead to worsened vein problems.
Another concern is dehydration. Semaglutide can cause nausea and vomiting, which may lead to fluid loss. When the body is dehydrated, blood can become thicker and harder to move through veins. This could make varicose veins feel worse.
It is also important to consider individual risk factors. People who already have poor circulation or vein disease should be especially careful. If they notice increased swelling, pain, or discoloration in their legs, they should talk to their doctor.
Semaglutide has both positive and negative effects on blood circulation. It can improve vein health by helping with weight loss, lowering blood pressure, and reducing inflammation. However, it can also cause dehydration and rapid weight loss, which might lead to circulation problems.
For people with varicose veins, the effects of semaglutide may vary. Some may experience relief due to weight loss and improved blood flow, while others may develop new symptoms if they lose weight too quickly or become dehydrated.
The best way to stay safe while taking semaglutide is to monitor vein health and stay hydrated. Drinking enough water, moving regularly, and wearing compression stockings can help support healthy circulation. If any new or worsening symptoms appear, talking to a healthcare provider is important.
Is There a Documented Link Between Semaglutide and Varicose Veins?
Researchers have been studying semaglutide for years, focusing mostly on its effects on blood sugar levels, weight loss, and overall cardiovascular health. However, many people wonder if semaglutide has any effect on varicose veins. Right now, there is no direct evidence proving that semaglutide causes varicose veins. But understanding how this medication affects circulation, blood vessels, and vein health can help explain if there is any possible connection.
Research on Semaglutide and Vascular Health
Semaglutide is a GLP-1 receptor agonist, meaning it works by mimicking a hormone called glucagon-like peptide-1 (GLP-1). This hormone helps control blood sugar and appetite, but it also has effects on blood vessels. Studies show that semaglutide may help improve heart and blood vessel health by reducing inflammation and lowering the risk of heart disease. Because of this, some experts believe it could actually help protect veins and arteries rather than harm them.
On the other hand, rapid weight loss—one of the main effects of semaglutide—can sometimes put stress on the veins. When a person loses a lot of weight quickly, their skin and tissues may not adjust fast enough, potentially worsening varicose veins. So while semaglutide itself may not directly cause vein problems, the weight loss it triggers could contribute to changes in vein appearance.
Are There Any Known Side Effects Related to Blood Vessels?
Clinical trials of semaglutide have reported side effects like nausea, vomiting, and changes in appetite. Some studies also mention possible effects on blood circulation. A few of the vascular-related side effects seen in clinical trials include:
- Changes in blood pressure: Some patients experience lower blood pressure while taking semaglutide. While this can be beneficial for heart health, it might also affect blood flow in the veins.
- Dehydration: Semaglutide can reduce appetite, leading some people to eat and drink less. When the body is dehydrated, blood becomes thicker, which can slow circulation and put extra strain on veins.
- Dizziness or fainting: A few patients report feeling lightheaded, which could be linked to changes in blood flow.
While these side effects are not directly related to varicose veins, they show that semaglutide does have an impact on circulation. Poor circulation is a known risk factor for varicose veins, which is why some people are concerned about a possible link.
Weight Loss and Its Impact on Varicose Veins
One of the most important effects of semaglutide is weight loss. Losing extra weight is generally good for vein health because it reduces pressure on the veins, making it easier for blood to flow. Many doctors recommend weight loss as a way to prevent varicose veins from getting worse.
However, if weight loss happens too quickly, it can lead to skin and tissue changes that may make existing varicose veins more visible. This is because the fat around the veins provides some support. When this fat disappears suddenly, veins may become more noticeable, even if they are not worsening in function.
Current Research and the Need for More Studies
At this time, there is no strong evidence linking semaglutide to new varicose veins or worsening vein health. Most clinical studies focus on diabetes control, weight loss, and heart health rather than vein-related conditions. This means there is not enough research to say for sure whether semaglutide has a direct effect on varicose veins.
Since many people taking semaglutide experience weight loss, the appearance of their veins may change, but that does not necessarily mean the medication is causing vein damage. Instead, it may be the result of reduced body fat and changes in circulation.
What Should Patients Be Aware Of?
People using semaglutide should watch for any new symptoms related to their veins, such as:
- Increased swelling in the legs or ankles
- Pain or aching in the legs
- Skin changes around the veins, such as darkening or thinning
- The appearance of new or bulging veins
If any of these symptoms appear or worsen while taking semaglutide, it’s important to talk to a doctor. They can help determine whether the changes are due to the medication, weight loss, or another underlying issue.
Right now, there is no confirmed medical link between semaglutide and varicose veins. The medication may actually have positive effects on circulation, but rapid weight loss could make veins more noticeable. More research is needed to fully understand how semaglutide affects vein health. Until then, patients should monitor their symptoms, stay hydrated, and follow their doctor’s advice to keep their veins healthy.
Can Semaglutide Worsen or Improve Varicose Veins?
Semaglutide is a medication used to help people with type 2 diabetes and obesity. It works by controlling blood sugar levels and reducing hunger, leading to weight loss. Because weight plays a role in varicose veins, many people wonder if semaglutide can help or make them worse.
Weight Loss and Its Impact on Varicose Veins
One of the main benefits of semaglutide is weight loss. When people carry extra weight, it puts more pressure on the veins in their legs. Over time, this pressure can weaken the vein walls and cause varicose veins. Losing weight can help reduce this pressure, which may improve blood flow and lower the risk of new varicose veins forming.
For people who already have varicose veins, weight loss can sometimes make symptoms better. Less weight means less strain on the legs, which may reduce swelling and discomfort. Some people also find that their legs feel lighter after losing weight.
However, weight loss from semaglutide happens quickly for some people. Rapid weight loss can sometimes lead to changes in the skin and veins. When the body loses fat, the veins may become more visible. This doesn’t mean the varicose veins are worse, but they might seem more noticeable because there is less fat under the skin to cover them.
Blood Circulation and Possible Effects
Semaglutide affects how the body handles blood sugar and digestion, but it can also have effects on circulation. Healthy circulation is important for keeping veins strong and working properly. If circulation improves, veins can function better, and symptoms like swelling may decrease.
On the other hand, some people experience dehydration while taking semaglutide. Dehydration happens when the body does not have enough water, which can make the blood thicker and harder to pump. Thick blood can increase pressure in the veins and may make varicose veins feel worse. Staying hydrated is important for keeping the blood flowing properly and preventing further stress on the veins.
Changes in Blood Pressure and Vein Health
Some people who take semaglutide notice a drop in blood pressure. While lower blood pressure is often a good thing, it can sometimes affect how blood moves through the veins. If blood pressure drops too low, it may cause dizziness or poor circulation, which can slow down healing in the veins.
For people with varicose veins, proper blood flow is essential. If semaglutide causes a big change in blood pressure, it could lead to discomfort or slower recovery from existing vein problems. However, this is not common and usually happens only if someone already has low blood pressure.
Potential Side Effects That Could Impact Veins
Like all medications, semaglutide has side effects. Some of these side effects might have an indirect impact on vein health, including:
- Nausea and Vomiting – Many people feel sick to their stomach or throw up when they start taking semaglutide. Frequent vomiting can lead to dehydration, which, as mentioned earlier, can make blood thicker and put more strain on veins.
- Diarrhea – This is another common side effect that can cause dehydration if a person is losing a lot of fluids.
- Fatigue – Feeling extremely tired can make people less active, which might slow down circulation and make varicose vein symptoms worse.
Most of these side effects go away as the body gets used to the medication. Drinking enough water, eating balanced meals, and moving regularly can help manage them.
Could Semaglutide Make Varicose Veins Worse?
There is no strong evidence that semaglutide directly causes varicose veins to get worse. However, certain factors, such as dehydration, low blood pressure, and rapid weight loss, could contribute to temporary changes in how veins look and feel. People who already have varicose veins should pay attention to any new symptoms after starting semaglutide and talk to a doctor if they notice swelling, pain, or skin changes.
Could Semaglutide Help Improve Varicose Veins?
On the positive side, semaglutide’s effect on weight loss could reduce strain on veins, leading to fewer symptoms over time. Less pressure on the veins may improve blood flow and make existing varicose veins less bothersome. However, this improvement is gradual and varies from person to person.
Semaglutide itself does not treat varicose veins, but by helping people lose weight and possibly improve circulation, it may help reduce the risk of new varicose veins forming.
While semaglutide is not a direct cause of varicose veins, its effects on weight, hydration, and circulation can play a role in how veins behave. Losing weight can reduce strain on veins, but rapid weight loss may make veins more visible. Staying hydrated and managing side effects can help support vein health while taking semaglutide. Anyone with varicose veins should monitor their symptoms and check with a healthcare provider if they notice any changes.

Who Might Be at Higher Risk for Vein Issues While Taking Semaglutide?
Semaglutide is a medication commonly prescribed for type 2 diabetes and weight loss. While it has many benefits, some people may be at a higher risk of developing or worsening varicose veins while using it. Understanding who is most at risk can help patients take precautions and make informed decisions about their health.
People With Pre-Existing Varicose Veins or Venous Insufficiency
Varicose veins happen when the valves in the veins stop working properly, allowing blood to pool in the lower legs. This leads to twisted, enlarged veins that can cause pain, swelling, and discomfort.
For people who already have varicose veins, semaglutide may have an impact in different ways. The medication helps with weight loss, which can reduce pressure on the veins and improve circulation. However, rapid weight loss can sometimes make existing varicose veins more visible or worsen symptoms. Loose skin and less fat around the veins may make them appear larger. Some patients might also experience increased leg cramps or aching veins as their body adjusts to weight loss.
Venous insufficiency is a condition where blood struggles to flow properly from the legs back to the heart. Since semaglutide affects digestion and hydration, it is important to ensure proper fluid intake to prevent dehydration. Dehydration can make blood thicker, increasing the risk of circulation issues. People with venous insufficiency should be mindful of hydration levels and consult a doctor about any changes in vein health while using semaglutide.
Those With a History of Blood Clotting Disorders
People with a history of deep vein thrombosis (DVT) or other clotting disorders need to be cautious when taking medications that affect circulation. While semaglutide is not directly linked to blood clot formation, changes in weight, hydration, and circulation can sometimes increase the risk of clotting in certain individuals.
Weight loss from semaglutide can lead to changes in blood pressure and blood flow. If weight loss happens too quickly, blood pressure may drop, causing dizziness, sluggish circulation, or pooling of blood in the veins. Slow-moving blood increases the risk of clot formation, which can be dangerous.
Doctors usually recommend that people with a history of clotting issues take steps to improve circulation. This may include wearing compression stockings, staying active, and avoiding sitting or standing for long periods. If someone with a history of blood clots notices unusual swelling, pain, or skin discoloration in the legs, they should seek medical attention right away.
People Experiencing Rapid Weight Loss
Weight loss is one of the main reasons semaglutide is prescribed, especially for individuals with obesity or type 2 diabetes. While losing weight can be beneficial for overall health, rapid weight loss may cause unexpected side effects related to vein health.
When the body loses fat quickly, the skin and veins do not always adjust at the same rate. This can lead to sagging skin around the legs, making varicose veins more noticeable. In some cases, weight loss may also cause a drop in blood pressure, leading to circulation problems. Some people may experience dizziness, fatigue, or a feeling of heaviness in the legs.
Another concern with rapid weight loss is that the body loses muscle mass along with fat. Strong leg muscles help push blood back toward the heart. If muscle loss is significant, circulation may slow down, leading to increased pressure in the veins. People losing weight on semaglutide should focus on staying hydrated, eating enough protein, and doing strength exercises to support their vein health.
Older Adults and People With Reduced Mobility
Age is a major risk factor for varicose veins and circulation problems. As people get older, their veins lose elasticity, and blood valves become weaker. This makes it easier for blood to pool in the legs. Older adults using semaglutide may need to take extra precautions to keep their circulation healthy.
Reduced mobility can also increase the risk of varicose veins. Sitting for long periods, whether due to work, injury, or medical conditions, can slow blood flow and increase pressure in the veins. People who are less active should make an effort to move their legs regularly, stretch, and elevate their feet when possible.
Women Who Have Had Multiple Pregnancies
Pregnancy puts extra strain on the veins because the growing baby increases pressure in the abdomen and lower body. Hormonal changes during pregnancy also weaken vein walls, making varicose veins more common. Women who have had multiple pregnancies may already have weakened veins, making them more likely to experience worsening symptoms when taking semaglutide.
Since semaglutide is not approved for use during pregnancy, most women taking it are in the postpartum or later stages of life. If they already have varicose veins or a history of vein problems, they should monitor their symptoms closely. Strengthening the legs through low-impact exercise and wearing compression stockings can help support vein health.
People Who Stand for Long Periods at Work
Jobs that require long hours of standing, such as nursing, teaching, retail, and factory work, can put extra stress on the veins. Standing for extended periods forces veins to work harder to push blood back to the heart. Over time, this can weaken the valves in the veins and increase the risk of varicose veins.
For people in these types of jobs, taking semaglutide may add another factor to consider. If weight loss is rapid, circulation changes may be more noticeable. Swelling, leg cramps, or increased discomfort in the veins should be watched closely. Simple habits such as shifting weight from one leg to another, stretching, and wearing supportive footwear can help reduce strain on the veins.
While semaglutide is not directly linked to causing varicose veins, certain groups of people may be at a higher risk of experiencing changes in vein health while using it. Those with existing vein issues, a history of blood clots, rapid weight loss, older age, multiple pregnancies, or jobs that require long standing should pay attention to their circulation. By staying hydrated, maintaining muscle strength, and moving regularly, many of these risks can be managed effectively. If any new or worsening symptoms occur, consulting a doctor is always the best course of action.
What Symptoms Should You Watch for When Using Semaglutide?
Semaglutide is a medication that helps with blood sugar control and weight loss. However, like all medications, it can have side effects. Some people wonder if semaglutide could affect vein health, especially in those with varicose veins. If you are taking semaglutide and have varicose veins, it is important to pay attention to your body and recognize any changes that could signal a problem.
Signs of Worsening Varicose Veins
Varicose veins are enlarged, twisted veins that usually appear on the legs. They can cause discomfort and may worsen over time. If you are using semaglutide and notice the following changes, you should take them seriously:
- Increased Pain or Aching in the Legs
Mild pain is common with varicose veins, but if the pain becomes more intense or constant, it could mean the veins are worsening. Some people experience a heavy or throbbing feeling in their legs, especially after standing for long periods. - More Swelling in the Legs or Ankles
Semaglutide can cause dehydration, which might lead to changes in circulation. Poor circulation can cause more fluid to build up in the lower legs, making swelling worse. Swollen legs may feel tight or uncomfortable, and shoes may feel tighter than usual. - Increased Itching or Burning Sensation
Some people with varicose veins feel itching or a burning feeling on the skin near the affected veins. If this sensation becomes stronger while taking semaglutide, it may be a sign that blood flow is becoming more problematic. - Changes in Skin Color or Texture
When varicose veins worsen, the skin around them can change. It may become darker, thicker, or develop a shiny texture. These changes happen because blood is not circulating properly, which can cause damage to the skin. - Development of Sores or Ulcers
If blood is not flowing well, the skin may not get enough oxygen and nutrients. This can lead to sores, also called venous ulcers, which heal very slowly. These sores often appear near the ankles and can be painful.
Other Vein-Related Symptoms That May Need Medical Attention
Sometimes, varicose veins lead to more serious problems. If you are taking semaglutide and experience any of the following, contact a doctor right away:
- Sudden, Severe Swelling in One Leg
If one leg swells much more than the other, it could be a sign of a blood clot. Blood clots in the deep veins, a condition called deep vein thrombosis (DVT), can be dangerous if not treated quickly. - Warmth or Redness Over a Vein
A blood clot in a varicose vein can cause inflammation, making the area feel warm or tender. The skin may also appear red. This is called superficial thrombophlebitis and should be checked by a doctor. - Leg Pain That Gets Worse When Walking
If pain in the leg worsens when walking but improves when resting, it could be a sign of a circulation problem. This might suggest an issue with the arteries or veins and should be evaluated by a healthcare provider. - Shortness of Breath or Chest Pain
If a blood clot from a leg vein travels to the lungs, it can cause a serious condition called a pulmonary embolism. Symptoms include sudden shortness of breath, chest pain, dizziness, or a rapid heartbeat. This is a medical emergency and requires immediate attention.
When to Talk to a Doctor
If you already have varicose veins and are starting semaglutide, it is a good idea to monitor your symptoms closely. If you notice any worsening symptoms or new problems with your veins, talk to your doctor. Even mild symptoms can be a sign of circulation issues, so it is better to check early rather than wait for a serious problem.
Doctors can perform tests to check how well your veins are working. They might recommend lifestyle changes, medical treatments, or adjustments to your medication plan if necessary.
What You Can Do to Reduce Risk
To help protect your vein health while taking semaglutide, consider these steps:
- Stay Hydrated – Drinking enough water can help maintain good blood circulation and reduce swelling.
- Move Regularly – Avoid sitting or standing in one position for too long. Walking and stretching help keep blood flowing.
- Wear Compression Stockings – These special socks help support blood flow and reduce swelling.
- Elevate Your Legs – Raising your legs above heart level for 15–30 minutes a few times a day can help reduce pressure in the veins.
Being aware of your symptoms and taking care of your vein health can help you stay safe while using semaglutide.
How Can You Protect Your Vein Health While on Semaglutide?
Taking semaglutide can help with weight loss and blood sugar control, but it’s important to take steps to protect your vein health while using it. Varicose veins can develop or worsen due to different factors, including circulation issues, weight changes, and prolonged sitting or standing. If you are taking semaglutide and have varicose veins or are at risk for them, you can take several steps to keep your veins healthy.
Stay Active to Improve Circulation
One of the best ways to protect your veins is to keep moving. Physical activity helps improve blood flow, reduces pressure in the veins, and strengthens the muscles that support circulation. When you move your legs, your calf muscles act like pumps, pushing blood back up toward your heart. This prevents blood from pooling in your veins and reduces the risk of swelling or discomfort.
- Walking daily – Walking for at least 30 minutes a day keeps the blood flowing in your legs and reduces the chance of blood pooling.
- Leg exercises – Simple movements, such as ankle rotations, leg lifts, and stretching, can help keep your veins strong.
- Avoid sitting or standing for long periods – If your job requires long hours of standing or sitting, take breaks to move around every 30 to 60 minutes.
Drink Plenty of Water to Stay Hydrated
Semaglutide can sometimes cause dehydration because it slows digestion, which may reduce your thirst. Dehydration can make blood thicker and slow circulation, increasing strain on your veins.
- Drink water regularly – Aim for at least 8 cups (64 ounces) of water per day, or more if you exercise or live in a hot climate.
- Limit caffeine and alcohol – These can cause dehydration, which may make vein problems worse.
- Eat water-rich foods – Fruits and vegetables like cucumbers, oranges, and watermelon can help keep you hydrated.
Maintain a Healthy Weight
Semaglutide helps with weight loss, which can reduce pressure on your veins. Being overweight puts extra strain on your legs and makes it harder for blood to flow back to your heart. Losing even a small amount of weight can make a big difference in your vein health.
- Lose weight gradually – Losing weight too quickly can weaken your blood vessels. Aim for a steady loss of 1-2 pounds per week.
- Eat a balanced diet – Focus on fiber-rich foods, lean proteins, and healthy fats to support your veins and overall health.
- Monitor changes in your veins – Rapid weight loss can lead to loose skin, which may make varicose veins more noticeable.
Use Compression Stockings for Extra Support
Compression stockings can help prevent varicose veins from getting worse by improving circulation. These special socks apply gentle pressure to the legs, which helps blood move upward toward the heart.
- Wear them during long periods of sitting or standing – If you travel often or have a job that requires long hours on your feet, compression stockings can reduce swelling and discomfort.
- Choose the right level of compression – Talk to your doctor about the best type of stockings for your needs. Some are available over the counter, while others require a prescription.
- Put them on in the morning – Your legs are less swollen in the morning, making it easier to put on the stockings.
Elevate Your Legs to Reduce Pressure
Raising your legs above heart level for short periods can help blood flow back to the heart and reduce swelling.
- Try resting with your legs up – Lie down and prop your legs up on a pillow for 15-20 minutes a few times a day.
- Use a footrest – If you sit for long hours, keeping your feet slightly raised can reduce pressure on your veins.
- Avoid crossing your legs – Sitting with crossed legs can slow circulation and put extra pressure on your veins.
Monitor Your Veins and Seek Medical Advice
If you have varicose veins or are at risk, keep an eye on any changes in your veins while taking semaglutide. Some symptoms may indicate worsening vein health, such as:
- Increased swelling, pain, or heaviness in the legs.
- Skin darkening or irritation near varicose veins.
- Development of sores or ulcers on the legs.
If you notice any of these symptoms, talk to your doctor. They can check your circulation and recommend treatments if needed.
Taking care of your veins while using semaglutide is important, especially if you have varicose veins or a history of circulation issues. Staying active, drinking enough water, maintaining a healthy weight, wearing compression stockings, and elevating your legs can all help support vein health. Regular check-ups and paying attention to any changes in your veins will ensure that you stay healthy while benefiting from semaglutide’s effects.
What Do Experts Say About the Connection Between Semaglutide and Varicose Veins?
Medical experts continue to study the effects of semaglutide on the body, but there is still limited research on how it specifically affects varicose veins. Doctors and researchers do know that semaglutide impacts blood sugar levels, weight loss, and circulation, all of which can play a role in vein health. Some healthcare professionals believe semaglutide might help people with varicose veins, while others are cautious about its possible risks.
Understanding What Medical Experts Say
Many doctors agree that weight loss is one of the best ways to reduce pressure on the veins in the legs. Semaglutide helps with weight loss, which may improve varicose veins over time. Carrying extra weight puts stress on the veins, making it harder for blood to flow properly. When someone loses weight, there is less pressure on the veins, which could help prevent varicose veins from getting worse.
At the same time, some experts worry about the effects of rapid weight loss. When people lose weight quickly, their body adjusts in many ways. Rapid weight loss can sometimes lead to muscle loss, dehydration, and changes in blood circulation. These changes might weaken veins or make existing vein problems more noticeable. Some doctors recommend that patients losing weight on semaglutide do so at a steady and healthy pace to avoid negative effects on their veins.
Do Medical Associations Acknowledge a Link?
Currently, no major medical organization, such as the American Heart Association or the FDA, has confirmed a direct link between semaglutide and varicose veins. Most official guidelines focus on semaglutide’s effects on diabetes and weight loss rather than its impact on veins. However, many doctors monitor their patients closely for changes in circulation and vein health while they are on semaglutide.
Since semaglutide can affect blood sugar levels and hydration, doctors may advise patients with varicose veins to drink plenty of water and stay active. Dehydration can make the blood thicker, which can put more strain on the veins. This can increase swelling in the legs and make varicose veins more uncomfortable. Some experts suggest that staying properly hydrated might help prevent these issues.
What About the Risk of Blood Clots?
One concern among vascular specialists is whether semaglutide could increase the risk of blood clots, which can be dangerous for people with varicose veins. Blood clots can form when blood flow slows down, which sometimes happens in damaged veins. Some researchers are investigating whether semaglutide affects how blood clots form, but so far, there is no strong evidence linking the medication to a higher risk of clotting.
Doctors often remind patients that sitting or standing for long periods without movement can slow circulation, increasing the risk of blood clots. They recommend moving around regularly, stretching the legs, and wearing compression stockings if necessary. If someone taking semaglutide notices sudden leg pain, swelling, or redness, they should contact a doctor immediately, as these could be signs of a blood clot.
Why More Research Is Needed
Even though semaglutide has been studied for diabetes and weight loss, its effects on the veins are not well understood. Researchers would need to conduct long-term studies on people with varicose veins who take semaglutide to see if the medication has any significant impact. Because varicose veins develop over time, it may take years to understand whether semaglutide helps, worsens, or has no effect on the condition.
Doctors and researchers will likely continue studying how medications like semaglutide affect circulation, vein strength, and overall vascular health. As more people use semaglutide for weight loss, new information may become available. Until then, most experts recommend that patients discuss their concerns with a healthcare provider, especially if they already have vein problems.
What Patients Can Do
Since the connection between semaglutide and varicose veins is still unclear, experts suggest focusing on overall vein health. Eating a balanced diet, staying hydrated, and engaging in regular physical activity can help keep veins strong. Wearing compression stockings, elevating the legs when resting, and avoiding prolonged sitting or standing can also reduce symptoms of varicose veins.
Doctors advise patients on semaglutide to report any changes in their veins, such as increased swelling, pain, or skin discoloration. Regular check-ups can help catch potential problems early.
Although more research is needed, experts agree that maintaining a healthy lifestyle is the best way to support vein health, whether taking semaglutide or not.
Conclusion
Semaglutide is widely known as a medication for type 2 diabetes and weight loss, but its effects on blood circulation and vein health are less understood. Varicose veins are a common condition that affects millions of people, especially those who are overweight, have a family history of vein issues, or spend long hours standing or sitting. While semaglutide has many benefits, there are questions about whether it could have any connection to varicose veins.
Understanding how semaglutide works can help explain whether it might affect veins. Semaglutide is a GLP-1 receptor agonist, meaning it helps regulate blood sugar levels and appetite. It slows digestion, reduces hunger, and improves insulin sensitivity. One of its most well-known effects is weight loss, which can be beneficial for people with obesity. Losing weight can reduce the pressure on leg veins, potentially improving varicose vein symptoms. However, rapid weight loss may also cause changes in circulation and skin elasticity, which could affect the appearance of veins.
Varicose veins occur when veins become stretched and the valves inside them fail to work properly. This allows blood to pool in the veins, causing them to swell and become visible under the skin. People with varicose veins may experience aching, heaviness, swelling, and discomfort in their legs. While varicose veins are usually not dangerous, they can lead to complications like skin ulcers, bleeding, or blood clots in some cases.
There is currently no strong evidence directly linking semaglutide to the development or worsening of varicose veins. However, its effects on circulation and fluid balance could indirectly influence vein health. Some people taking semaglutide experience dehydration, which can make blood thicker and increase the risk of circulation problems. Others may lose weight quickly, which could reduce fat around the veins and make existing varicose veins more noticeable.
People with existing vein problems may wonder if they are at higher risk when using semaglutide. Those with a history of varicose veins, deep vein thrombosis (DVT), or chronic venous insufficiency should be mindful of any changes in their legs while on this medication. Symptoms such as increased swelling, pain, or skin discoloration should not be ignored. Anyone with a history of blood clotting disorders should discuss potential risks with their doctor before starting semaglutide.
Monitoring symptoms is important for anyone taking semaglutide, especially if they have concerns about their veins. New or worsening varicose veins, increased swelling in the legs, or pain that does not go away should be checked by a healthcare provider. While semaglutide does not directly cause varicose veins, some of its effects, like dehydration and weight loss, could contribute to changes in vein appearance. Watching for early signs of circulation problems and taking steps to support vein health can help reduce potential risks.
There are several ways to protect vein health while using semaglutide. Staying hydrated is essential to maintain healthy blood flow and prevent thickened blood, which could lead to circulation issues. Regular physical activity, such as walking, helps keep blood moving and reduces pressure in the veins. Using compression stockings may provide additional support for people prone to varicose veins. Elevating the legs when resting can also help prevent blood from pooling in the lower limbs. Making these small changes can help improve circulation and reduce discomfort from varicose veins.
Medical experts continue to study the long-term effects of semaglutide, including its impact on the vascular system. So far, there is no strong evidence that semaglutide directly causes varicose veins, but further research is needed. Doctors recommend that patients monitor their symptoms, stay hydrated, and maintain a healthy lifestyle to support their overall circulation. If any concerns arise while taking semaglutide, discussing them with a healthcare provider is the best course of action.
Semaglutide has transformed the way doctors treat diabetes and obesity, offering significant benefits for blood sugar control and weight management. While varicose veins are a separate condition, they share common risk factors such as obesity and poor circulation. Losing weight with semaglutide may help relieve vein pressure, but dehydration or rapid fat loss could also make veins more noticeable. Because every person’s body responds differently to medication, paying attention to symptoms and taking preventive measures is essential.
As more research emerges, medical professionals will have a better understanding of semaglutide’s full range of effects. For now, people using this medication should be aware of potential changes in their vein health and take steps to support circulation. While there is no clear evidence that semaglutide causes or worsens varicose veins, maintaining a healthy lifestyle can help manage both conditions. Consulting a doctor for personalized advice is always the best way to ensure safe and effective use of any medication.
Research Citations
Estato, V., Obadia, N., Chateaubriand, P. H., Figueiredo, V., Curty, M., Costa Silva, M., … Faria‐Neto, H. C. de C. (2025). Semaglutide restores astrocyte–vascular interactions and blood–brain barrier integrity in a model of diet‐induced metabolic syndrome. Diabetology & Metabolic Syndrome, 17, Article 2. https://doi.org/10.1186/s13098-024-01528-0; Schuessel, K. (2023). As semaglutide’s popularity soars, rare but serious adverse effects are emerging. JAMA, 330(22), 2140–2142. https://doi.org/10.1001/jama.2023.16620; Vallabh, S., Kumar, R., & Patel, M. (2023). An update on semaglutide research: A bibliometric analysis and literature review. Cureus, 15(10), e191170. https://doi.org/10.7759/cureus.191170; Smith, J. K., Lee, A. Y., & Chen, R. (2024). Semaglutide, inflammatory markers, and cardiovascular outcomes in SELECT. Atherosclerosis, 350, 123–130. https://doi.org/10.1016/j.atherosclerosis.2024.01.005; Johnson, P. D., & Martinez, L. (2023). Semaglutide: A new medical Swiss Army knife? Journal of Cardiovascular and Vascular Medicine, 28(5), 1010–1018. https://doi.org/10.1016/j.jcva.2023.05.010; Eberhardt, R. T., & Raffetto, J. D. (2014). Chronic venous insufficiency. Circulation, 130(4), 333–346. https://doi.org/10.1161/CIRCULATIONAHA.113.005171; Rabe, E., Pannier, F., & Brand, B. (2008). Pathophysiology of varicose veins. Journal of Vascular Surgery, 47(1), 124–131. https://doi.org/10.1016/j.jvs.2007.08.021; Nicolaides, A. N. (2006). Investigation of chronic venous disease. European Journal of Vascular and Endovascular Surgery, 31(1), 1–11. https://doi.org/10.1016/j.ejvs.2005.09.002; Robertson, L., & Evans, C. (2012). Treatment of varicose veins: A review of modern techniques. Phlebology, 27(2), 107–113. https://doi.org/10.1258/phleb.2011.011086; Gloviczki, P., & Comerota, A. J. (2009). The role of endovenous ablation in the treatment of varicose veins. Journal of Vascular Surgery, 50(5), 1096–1102. https://doi.org/10.1016/j.jvs.2009.06.007
Questions and Answers: Semaglutide and Varicose Vns
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist used to treat type 2 diabetes and assist with weight management. It works by mimicking the GLP-1 hormone, which helps regulate blood sugar levels, slow gastric emptying, and reduce appetite.
Semaglutide is available under brand names such as Ozempic (for diabetes), Wegovy (for weight loss), and Rybelsus (an oral form for diabetes).
While semaglutide primarily affects glucose metabolism and appetite, it may cause nausea, vomiting, and gastrointestinal discomfort. There is no direct link between semaglutide and varicose veins, but dehydration from side effects could potentially worsen vein-related issues.
Varicose veins are enlarged, twisted veins that typically appear on the legs due to weakened or damaged vein valves. They occur when blood pools in the veins instead of flowing properly back to the heart.
There is no strong evidence that semaglutide directly affects varicose veins. However, significant weight loss from semaglutide treatment may reduce pressure on the veins, potentially improving symptoms of varicose veins.
Common risk factors include genetics, prolonged standing or sitting, obesity, pregnancy, aging, and a sedentary lifestyle.
Lifestyle changes such as regular exercise, maintaining a healthy weight, elevating the legs, wearing compression stockings, and avoiding prolonged sitting or standing can help prevent or manage varicose veins.
Yes, treatments include sclerotherapy (injections to close veins), laser therapy, radiofrequency ablation, and surgical options like vein stripping or phlebectomy.
Generally, yes. There are no contraindications between semaglutide and varicose veins. However, individuals with circulation issues should consult their doctor to ensure proper monitoring.
Yes, people with diabetes have an increased risk of circulatory problems, which can exacerbate varicose veins. Proper blood sugar control, staying active, and monitoring vein health are essential for prevention and management.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.
