Table of Contents
Section 1: Introduction
In recent years, the medical community has witnessed significant advancements in the treatment of type 2 diabetes and obesity, two conditions that pose considerable health risks globally. Among these advancements, semaglutide stands out as a groundbreaking pharmaceutical agent, offering not just improved glycemic control but also promising benefits for weight management. However, as with any potent medication, understanding its broader implications, especially on vital organs like the kidneys, is essential for both patients and healthcare providers. This article, titled “The Impact of Semaglutide on Kidney Function: What You Need to Know,” aims to shed light on this critical aspect of semaglutide’s profile.
Semaglutide belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of an endogenous hormone involved in glucose regulation. By enhancing insulin secretion, delaying gastric emptying, and suppressing appetite, semaglutide effectively manages blood sugar levels and promotes weight loss. Its utility in treating type 2 diabetes and, more recently, as a weight loss aid in non-diabetic individuals, has been well-documented, marking it as a versatile addition to the pharmacological arsenal against these conditions.
However, the kidneys’ role in filtering and eliminating waste products, including excess glucose, makes them particularly susceptible to damage from chronic high blood sugar and obesity-related stress. Consequently, medications like semaglutide that influence glucose metabolism and body weight could inherently affect kidney function. Given the prevalence of kidney-related complications among individuals with diabetes and obesity, understanding the impact of semaglutide on kidney health is not just a matter of academic interest but a practical necessity for optimizing patient care.
This article delves into the complex interplay between semaglutide and kidney function, guided by the latest research and clinical guidelines. By exploring how semaglutide affects the kidneys, its potential benefits and risks, and how it compares to other treatments, we aim to provide a comprehensive overview that informs and empowers patients and healthcare practitioners alike. Additionally, through real-life testimonials and expert analyses, readers will gain insights into the practical aspects of managing kidney health while on semaglutide, including monitoring protocols and precautionary measures.
The significance of kidney health cannot be overstated, as it underpins the overall well-being of individuals. By examining the impact of semaglutide within this context, we hope to highlight the importance of informed decision-making in the management of diabetes and obesity. As we navigate through the various sections of this article, keep in mind the ultimate goal: to enhance understanding and facilitate better outcomes for those relying on semaglutide as part of their treatment regimen.
Section 2: What Is Semaglutide?
Semaglutide represents a pivotal development in the pharmacological management of type 2 diabetes and obesity, two intertwined conditions that have reached epidemic proportions worldwide. As a glucagon-like peptide-1 (GLP-1) receptor agonist, semaglutide has been heralded for its dual ability to regulate blood sugar levels and facilitate weight loss, offering a beacon of hope for millions struggling with these health challenges. This section delves into the nature of semaglutide, its mechanism of action, and its application in clinical practice, providing a solid foundation for understanding its broader health implications.
Introduced to the market after rigorous clinical trials, semaglutide operates by mimicking the effects of the GLP-1 hormone, which plays a critical role in glucose metabolism. GLP-1, naturally secreted in response to food intake, enhances insulin secretion from the pancreas in a glucose-dependent manner, thereby lowering blood sugar levels. Additionally, it slows gastric emptying, contributing to a sensation of fullness and reduced appetite. Semaglutide’s action on GLP-1 receptors amplifies these effects, making it an effective tool for managing hyperglycemia in type 2 diabetes and aiding weight loss efforts.
The journey of semaglutide from its development to its approval by regulatory agencies underscores its significance in modern medicine. Available in injectable form (Ozempic) for diabetes management and oral formulation (Rybelsus) for both diabetes and as a separate injectable dose (Wegovy) for obesity, semaglutide offers flexibility and convenience to meet diverse patient needs. Its efficacy in lowering HbA1c levels, a marker of long-term glucose control, and promoting substantial weight reduction has been validated in numerous studies, making it a preferred option for individuals who have not achieved desired outcomes with other treatments.
Beyond its primary benefits, semaglutide’s impact on cardiovascular health, evidenced by reduced risks of major adverse cardiovascular events in patients with type 2 diabetes, positions it as a multifaceted therapeutic agent. Such findings reflect the drug’s potential not just in addressing specific conditions but in improving overall health outcomes, aligning with the holistic approach increasingly embraced in medical practice.
However, the introduction of semaglutide into clinical use also raised questions about its long-term effects, particularly on organs like the kidneys, which bear the brunt of metabolic disorders. As we explore the relationship between semaglutide and kidney function in subsequent sections, it is crucial to remember the drug’s mechanism of action and its systemic effects. Understanding the scientific principles underlying semaglutide’s operation will provide invaluable insights into its potential benefits and limitations, guiding optimal use in clinical settings.
Through a detailed examination of semaglutide’s attributes, this section aims to equip readers with a thorough understanding of the drug, setting the stage for a deeper investigation into its implications for kidney health. As semaglutide continues to play a significant role in managing diabetes and obesity, staying informed about its characteristics and effects is essential for both healthcare professionals and patients navigating these complex conditions.
Section 3: How Does Semaglutide Affect the Body?
Semaglutide’s impact on the body extends beyond its primary roles in glucose regulation and weight management, encompassing a broad range of physiological effects that contribute to its therapeutic benefits and side effect profile. Understanding these systemic effects is crucial for both healthcare providers and patients, as it informs treatment decisions, monitoring strategies, and patient education efforts. This section explores the multifaceted ways in which semaglutide influences bodily functions, highlighting its mechanism of action, metabolic effects, and potential implications for overall health.
At its core, semaglutide operates by activating GLP-1 receptors in the pancreas, stimulating the release of insulin in response to elevated blood glucose levels. This insulinotropic effect directly addresses the insulin deficiency or insensitivity characteristic of type 2 diabetes, leading to improved glycemic control. Simultaneously, semaglutide suppresses the secretion of glucagon, a hormone that increases blood glucose levels by promoting glycogen breakdown and glucose production in the liver. By reducing glucagon levels, semaglutide further contributes to lowering blood sugar.
The drug’s effects on gastric motility and appetite regulation are equally significant. By slowing gastric emptying, semaglutide prolongs the feeling of fullness after eating, which can lead to a reduction in food intake and, consequently, weight loss. This property is particularly beneficial for individuals with obesity, as it addresses one of the fundamental challenges in weight management: controlling caloric intake. Furthermore, semaglutide’s action on brain centers that regulate appetite and food cravings enhances its weight loss efficacy, offering an integrated approach to obesity treatment.
Beyond its direct metabolic effects, semaglutide has been associated with cardiovascular benefits, such as a decrease in systolic blood pressure, improvement in lipid profiles, and reduction in markers of inflammation. These effects may contribute to the observed reduction in cardiovascular events in patients treated with semaglutide, underscoring its potential as a cardioprotective agent in the context of type 2 diabetes and obesity, conditions that significantly increase cardiovascular risk.
However, the systemic nature of semaglutide’s action also means that its effects can extend to various organs and systems, with implications for kidney function, gastrointestinal health, and possibly the immune system. Understanding these effects, both beneficial and adverse, is essential for optimizing treatment outcomes and minimizing risks. For instance, while the drug’s impact on weight and metabolic control can indirectly benefit kidney health by reducing the burden of diabetes and hypertension, direct effects on renal physiology warrant careful consideration, as explored in the following section.
Semaglutide affects the body through a complex interplay of mechanisms that influence glucose metabolism, appetite regulation, gastrointestinal function, and cardiovascular health. Its role in modern therapeutic strategies for diabetes and obesity reflects the integration of these multifaceted effects, highlighting the importance of comprehensive management approaches that consider the patient’s overall health and coexisting conditions. As research continues to unravel the full spectrum of semaglutide’s actions, healthcare providers must remain attuned to emerging data to guide its use in clinical practice effectively.
Section 4: Common Kidney Diseases and Conditions
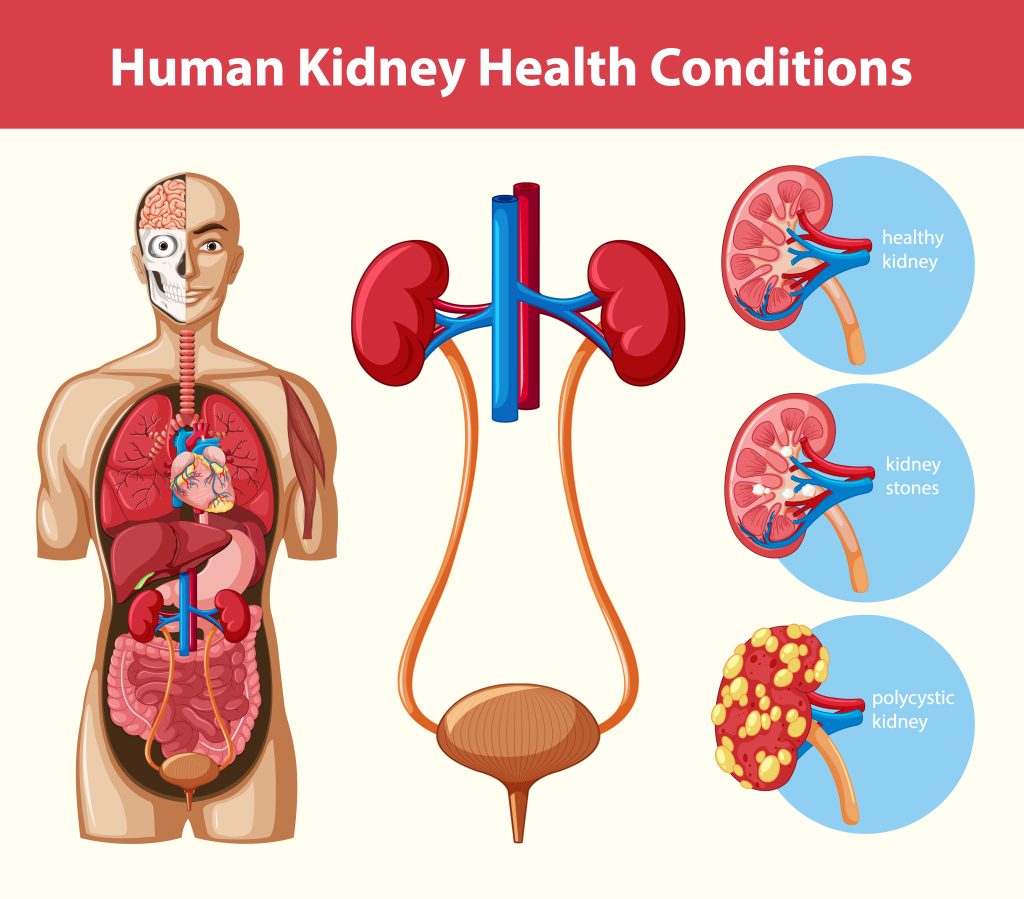
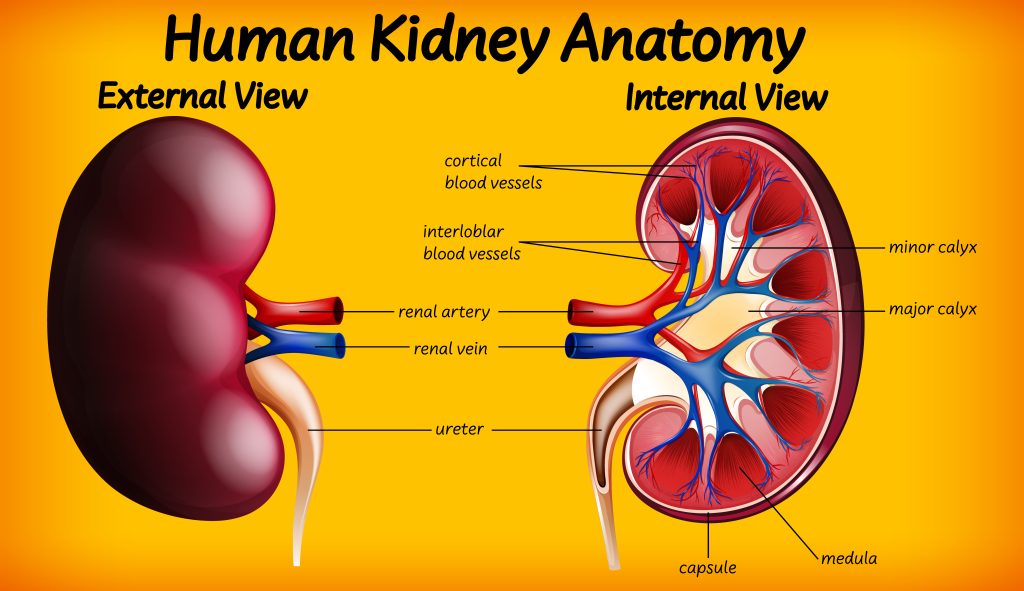
Understanding the landscape of common kidney diseases and conditions is essential for contextualizing the impact of semaglutide on kidney function. The kidneys play a pivotal role in filtering waste from the blood, regulating blood pressure, electrolyte balance, and red blood cell production. When kidney function is compromised, through either acute or chronic conditions, the consequences can be life-altering. This section provides an overview of prevalent kidney diseases and conditions, setting the stage for a detailed exploration of how semaglutide interacts with kidney health.
Chronic Kidney Disease (CKD): CKD is characterized by a gradual loss of kidney function over time. It often progresses silently, eventually leading to end-stage renal disease (ESRD) where dialysis or a kidney transplant is required. Diabetes and hypertension are the leading causes of CKD, making the management of these conditions critical in preventing CKD progression.
Acute Kidney Injury (AKI): AKI is a sudden episode of kidney failure or kidney damage that happens within a few hours or days. It causes waste products to build up in the blood and can be caused by factors such as severe dehydration, infection, and significant blood loss during surgery. Unlike CKD, AKI can be reversible if treated early and appropriately.
Diabetic Nephropathy: This condition is a complication of diabetes characterized by high protein levels in the urine, high blood pressure, and gradually worsening kidney function. It’s a leading cause of CKD and ESRD among diabetic patients, underscoring the importance of tight glucose control in preventing kidney damage.
Glomerulonephritis: This term refers to a group of diseases that cause inflammation and damage to the kidney’s filtering units, the glomeruli. It can be acute or chronic and can lead to CKD if not managed properly.
Polycystic Kidney Disease (PKD): PKD is a genetic disorder characterized by the growth of numerous cysts in the kidneys. These cysts can lead to enlarged kidneys and impair their function over time, potentially resulting in CKD.
Kidney Stones: Kidney stones are hard deposits of minerals and salts that form inside the kidneys. While they do not directly cause chronic kidney disease, they can lead to infections and obstructions, which, if recurrent or untreated, can damage kidney tissue.
Hypertension-Related Kidney Disease: High blood pressure can damage the blood vessels in the kidneys, reducing their ability to function properly. Managing blood pressure is crucial in preventing kidney damage in hypertensive patients.
Given this backdrop of kidney-related conditions, the question arises: how does semaglutide, a medication primarily used to treat diabetes and obesity, impact kidney function? The next sections will delve into the benefits and potential risks of semaglutide on kidney health, drawing on current research findings and clinical experiences. This discussion aims to provide a nuanced understanding of semaglutide’s role in the context of kidney disease, highlighting its therapeutic potential while acknowledging the complexities of managing patients with pre-existing kidney conditions.
Section 5: Benefits of Semaglutide on Kidney Health
The intersection of semaglutide’s therapeutic use in diabetes and obesity management with kidney health is a critical area of clinical interest, especially given the high prevalence of renal complications in these patient populations. Semaglutide, through its innovative mechanism of action, not only offers glycemic control and aids in weight reduction but also presents potential renal benefits that could significantly alter the landscape of chronic kidney disease (CKD) management, particularly among those with diabetic nephropathy. This section explores the evidence supporting the renal protective effects of semaglutide, its impact on various renal risk factors, and the potential underlying mechanisms that contribute to these outcomes.
5.1 Effectiveness in Slowing Diabetic Nephropathy Progression
Diabetic nephropathy, a leading cause of CKD, poses a significant challenge in diabetes management, with few treatment options directly addressing the renal damage caused by hyperglycemia. Semaglutide has emerged as a promising agent in this context, with studies indicating its ability to reduce markers of kidney damage, such as albuminuria, which signifies the leakage of albumin into the urine due to kidney damage. Clinical trials have shown that patients on semaglutide experience a notable reduction in albuminuria levels, suggesting a slowdown in the progression of diabetic nephropathy and potentially delaying the onset of end-stage renal disease (ESRD).
5.2 Indirect Renal Benefits through Risk Factor Modification
Beyond direct effects on the kidneys, semaglutide’s role in mitigating key risk factors for CKD, such as hypertension and poor glycemic control, offers additional pathways through which it benefits renal health. By improving insulin sensitivity and promoting weight loss, semaglutide can lead to better blood pressure control and lower blood glucose levels, both of which are crucial for reducing the strain on the kidneys. Moreover, weight loss associated with semaglutide use can decrease proteinuria, a condition characterized by excessive protein in the urine and a risk factor for CKD progression.
5.3 Potential Protective Mechanisms
The mechanistic basis for semaglutide’s renal benefits is thought to extend beyond its metabolic effects. Research suggests that GLP-1 receptor agonists like semaglutide may exert anti-inflammatory and antioxidative effects, reducing oxidative stress and inflammation within the kidneys, which are key drivers of CKD progression. Furthermore, the activation of GLP-1 receptors on renal tissues may enhance natriuresis (the excretion of sodium in urine), thereby improving blood pressure and reducing kidney hyperfiltration, a condition that can lead to long-term kidney damage.
5.4 Clinical Implications and Future Directions
The renal benefits of semaglutide underscore the importance of incorporating this medication into the treatment regimen for patients with type 2 diabetes at risk of CKD. Clinical guidelines are increasingly recognizing the value of GLP-1 receptor agonists in this context, recommending their use not only for glycemic control and weight management but also for their potential to confer renal protection. Ongoing and future studies focused on elucidating the long-term impact of semaglutide on kidney function and its efficacy in preventing CKD progression are crucial for refining treatment protocols and optimizing patient outcomes.
Semaglutide represents a multifaceted therapeutic agent with significant potential to benefit kidney health, particularly in the context of diabetes-related renal complications. Its ability to slow the progression of diabetic nephropathy, coupled with indirect benefits through risk factor modification and potential protective mechanisms, positions semaglutide as an important tool in the management of CKD.
Section 6: Risks and Side Effects Related to Kidney Function
While semaglutide has been celebrated for its benefits in managing diabetes and aiding in weight loss, understanding its safety profile, particularly regarding kidney function, is crucial. Semaglutide, like any potent medication, may have potential risks and side effects that could impact the kidneys, an aspect of paramount importance given the organ’s critical role in filtering and detoxifying the body. This section examines the reported adverse effects of semaglutide on kidney health, drawing upon clinical research, post-marketing surveillance, and pharmacovigilance reports to provide a comprehensive overview of its renal safety.
6.1 Reported Renal Adverse Effects
Instances of acute kidney injury (AKI) and other renal complications have been reported in patients using semaglutide. AKI, characterized by a sudden decrease in kidney function, has been observed in some cases, raising concerns about the drug’s impact on renal health. These incidents, while relatively rare, prompt a closer examination of semaglutide’s side effect profile and its mechanism of potentially influencing kidney function. The dehydration resulting from semaglutide’s gastrointestinal side effects, such as nausea and vomiting, is a proposed mechanism that may predispose patients to renal stress, potentially leading to AKI in vulnerable individuals.
6.2 Monitoring and Management of Renal Risks
Given the potential for renal adverse effects, healthcare providers are urged to exercise caution when prescribing semaglutide, especially to patients with pre-existing kidney conditions or those at high risk for renal impairment. Regular monitoring of kidney function through blood tests and urine analysis is recommended to detect any early signs of deterioration in renal health. Adjustments to the dosage of semaglutide or discontinuation of the medication may be necessary for patients who experience significant renal side effects.
6.3 Comparison with Other Glucose-Lowering Agents
When considering the renal safety of semaglutide, it is essential to compare it with other antidiabetic medications. While some glucose-lowering agents have a neutral or even beneficial effect on kidney function, others may carry a higher risk of renal complications. The risk-benefit profile of semaglutide, especially in the context of renal health, appears favorable when compared with medications that have a more pronounced risk of nephrotoxicity. However, individual patient factors, such as the stage of CKD and other comorbidities, play a critical role in determining the most appropriate therapy.
6.4 Implications for Clinical Practice
The potential renal risks associated with semaglutide underscore the importance of personalized medicine in diabetes care. Patients on semaglutide should be thoroughly evaluated for any history of kidney disease, and their renal function should be closely monitored throughout treatment. Educating patients about the signs and symptoms of kidney problems and the importance of staying hydrated can help mitigate some of the risks associated with semaglutide use.
While semaglutide offers significant benefits for individuals with diabetes and those seeking weight loss, attention to its renal side effects is necessary. By incorporating regular kidney function monitoring and considering the individual patient’s risk factors, healthcare providers can optimize the benefits of semaglutide while minimizing its potential risks to kidney health. Further research into the long-term renal effects of semaglutide will be invaluable in refining treatment guidelines and ensuring patient safety.

Section 7: Comparing Semaglutide with Other Treatments
In the realm of diabetes and obesity management, semaglutide emerges as a formidable player, offering a dual benefit of glycemic control and weight management. Its distinct mechanism as a GLP-1 receptor agonist sets it apart from other therapeutic agents, making it a subject of keen interest for both clinicians and patients. This section endeavors to dissect how semaglutide compares with other treatments, focusing on its efficacy, safety, and impact on renal health, to provide a nuanced perspective on its role in the therapeutic landscape.
Efficacy in Glycemic Control
Semaglutide’s ability to significantly lower HbA1c levels is well-documented, with studies showcasing its superiority over traditional antidiabetic agents like sulfonylureas and even some insulin therapies. Unlike sulfonylureas, which increase insulin production with a risk of hypoglycemia and weight gain, semaglutide enhances insulin secretion in a glucose-dependent manner, minimizing these risks. Compared to metformin, the first-line treatment for type 2 diabetes, semaglutide offers additional benefits in terms of weight reduction, although metformin is known for its safety profile and protective effects against cardiovascular diseases.
Impact on Weight Loss
The weight loss efficacy of semaglutide is a significant advantage, particularly when compared to other obesity treatments. Orlistat, which reduces fat absorption, and bupropion-naltrexone, which targets central pathways to decrease appetite, are effective but often limited by their side effect profiles and the extent of weight loss achieved. Semaglutide’s mechanism of mimicking GLP-1 not only suppresses appetite but also slows gastric emptying, contributing to substantial weight loss. This makes it a preferred option for individuals with obesity, especially those with concomitant type 2 diabetes, where weight management is crucial.
Cardiovascular Outcomes
The cardiovascular benefits of semaglutide present a compelling case for its use, particularly in contrast to other diabetes medications that may not confer such advantages. Semaglutide has been shown to reduce the risk of major adverse cardiovascular events, a benefit not universally observed with other antidiabetic agents. This positions semaglutide as a valuable option for patients with diabetes at high risk for cardiovascular diseases, offering a therapeutic choice that addresses both glycemic control and cardiovascular risk reduction.
Renal Health Comparisons
When considering the impact on renal health, semaglutide demonstrates a protective potential against the progression of kidney disease, particularly in the context of diabetic nephropathy. This is in contrast to medications such as NSAIDs used for pain management, which may exacerbate kidney problems, or even some SGLT2 inhibitors, which, while offering renal protection, come with their own set of risks and side effects. The ability of semaglutide to improve markers of kidney function and reduce albuminuria places it in a favorable position relative to other treatments that may lack these renal benefits.
Clinical Considerations and Patient Selection
Choosing the appropriate treatment requires a holistic view of the patient’s health status, preferences, and potential risk factors. Semaglutide’s profile makes it an attractive option for a broad spectrum of patients, including those with type 2 diabetes seeking to improve glycemic control and reduce weight, as well as those at risk for cardiovascular and renal complications. However, the decision to use semaglutide must be balanced with considerations of its side effects, cost, and the patient’s overall treatment goals.
Semaglutide distinguishes itself from other diabetes and obesity treatments through its dual benefits, favorable impact on cardiovascular and renal outcomes, and substantial weight loss efficacy. Its comparison with other treatments highlights the importance of individualized patient care and the need for a comprehensive approach to managing complex conditions like diabetes and obesity. As more data emerge, semaglutide’s role in treatment regimens will continue to evolve, underscoring the need for ongoing research and clinical vigilance.
Section 8: Monitoring Kidney Function: Guidelines for Patients on Semaglutide
The introduction of semaglutide into the therapeutic arsenal for diabetes and obesity management has been a significant advancement. However, its implications for kidney health necessitate a vigilant approach to monitoring kidney function in patients undergoing treatment. Given the kidneys’ critical role in filtering waste from the blood, maintaining electrolyte balance, and regulating blood pressure, understanding the guidelines for kidney function monitoring is paramount for optimizing patient outcomes and ensuring the safe use of semaglutide. This section outlines the recommended practices for monitoring kidney function in patients treated with semaglutide, integrating current research insights and clinical recommendations.
Importance of Baseline Assessment
Before initiating semaglutide, a comprehensive baseline assessment of kidney function is essential. This evaluation typically includes serum creatinine measurements to estimate the glomerular filtration rate (eGFR), a key indicator of kidney health. Additionally, assessing urine albumin-to-creatinine ratio (UACR) can help identify early signs of kidney damage, particularly useful in patients with diabetes, where diabetic nephropathy is a concern. This initial assessment establishes a reference point against which future changes in kidney function can be measured.
Regular Monitoring Schedule
After starting semaglutide, regular monitoring of kidney function is advised. The frequency of these assessments should be tailored to the individual patient’s risk factors, such as existing kidney disease, diabetes severity, and concurrent medications that may impact kidney function. For most patients, checking eGFR and UACR every 3 to 6 months is recommended. However, more frequent monitoring may be necessary for patients with established CKD or those showing signs of renal impairment.
Recognizing Signs of Renal Adverse Effects
Patients on semaglutide should be educated about the signs of potential kidney problems, including decreased urine output, swelling in the legs or feet (edema), and unexplained fatigue, which could indicate worsening kidney function. Early detection of these symptoms allows for prompt adjustment of treatment, which may include modifying the semaglutide dose or temporarily discontinuing its use until kidney function stabilizes.
Managing Risks and Adjustments in Therapy
In cases where a decline in kidney function is observed, a thorough evaluation is required to determine the cause and appropriate management strategy. This may involve adjusting the dose of semaglutide or considering alternative treatments, especially if the decline is significant and directly attributed to the medication. Collaboration with a nephrologist may be beneficial for patients with advanced CKD or those experiencing significant renal adverse effects.
Integration with Patient Care Plans
Monitoring kidney function in patients on semaglutide should be an integral part of a comprehensive care plan that includes glycemic control, blood pressure management, and lifestyle interventions. This holistic approach ensures that while patients benefit from semaglutide’s effects on diabetes and weight loss, their renal health is also protected and preserved.
Vigilant monitoring of kidney function is crucial for patients on semaglutide, involving baseline assessments, regular follow-ups, and patient education on the signs of kidney problems. By adhering to these guidelines, healthcare providers can maximize the benefits of semaglutide while minimizing its risks, ensuring patient safety and optimal outcomes in the management of diabetes and obesity.
Section 9: Patient Testimonials and Case Studies
The real-world impact of semaglutide on individuals with diabetes and obesity provides invaluable insights into its effectiveness and safety, including its implications for kidney health. Patient testimonials and case studies not only humanize the clinical data but also offer a nuanced understanding of how semaglutide can be integrated into diverse treatment regimes. This section delves into the experiences of patients who have been prescribed semaglutide, highlighting their journeys, the benefits they’ve observed, and the challenges they’ve faced, particularly concerning kidney function.
Personal Narratives: Weight Loss and Improved Glycemic Control
One of the most compelling aspects of semaglutide therapy is its dual action in promoting significant weight loss and enhancing glycemic control. For instance, John, a 52-year-old with type 2 diabetes and obesity, began semaglutide treatment as part of a comprehensive lifestyle modification plan. Over six months, John experienced a remarkable weight loss of 20% from his initial body weight and saw his HbA1c levels drop from 8.5% to 6.2%, effectively bringing his diabetes under better control. More importantly, John reported an improvement in his energy levels and overall well-being, underscoring the multifaceted benefits of semaglutide beyond mere numbers on a scale or lab reports.
Navigating Side Effects: Gastrointestinal Discomfort and Renal Concerns
While semaglutide’s benefits are significant, navigating its side effects presents a challenge for some patients. Sarah, a 45-year-old patient with a history of mild chronic kidney disease (CKD), experienced nausea and vomiting in the initial weeks of semaglutide treatment. Concerned about the potential impact on her kidney function, her healthcare team closely monitored her renal parameters, adjusting her semaglutide dosage to mitigate the gastrointestinal side effects while ensuring her CKD did not worsen. Sarah’s case highlights the importance of personalized treatment plans and the need for vigilance in monitoring kidney function, especially in patients with pre-existing renal conditions.
Case Study: Semaglutide and Renal Function Improvement
An intriguing case study involves Alex, a 60-year-old with type 2 diabetes, obesity, and early-stage diabetic nephropathy. After initiating semaglutide, not only did Alex report significant weight loss, but follow-up tests also indicated a stabilization of his kidney function, with a reduction in albuminuria levels. This case exemplifies the potential renal protective effects of semaglutide, suggesting that, in some patients, its use could contribute to slowing the progression of diabetic nephropathy.
A Spectrum of Experiences
These patient stories and case studies reflect a spectrum of experiences with semaglutide, from transformative health improvements to the careful management of side effects. They highlight the drug’s potential to significantly impact patients’ lives positively while also reminding us of the critical need for individualized care approaches. Importantly, these narratives underscore the value of integrating patient feedback into the ongoing evaluation and optimization of semaglutide as a treatment option, ensuring that its benefits are maximized across diverse patient populations.
Section 10: Future Directions in Research
The advent of semaglutide has marked a significant leap forward in the management of type 2 diabetes and obesity, with promising implications for kidney health. However, the journey of understanding its full potential and optimizing its use is far from complete. As we look to the future, several key areas of research are emerging, promising to deepen our understanding of semaglutide’s impact, refine its application, and potentially unveil new therapeutic avenues. This section explores the promising horizons in research that are set to shape the future of semaglutide in clinical practice.
Expanding Understanding of Mechanisms
While the current understanding of how semaglutide impacts glycemic control, weight loss, and kidney function is substantial, there remains a frontier of knowledge yet to be explored. Future studies aimed at elucidating the precise molecular mechanisms by which semaglutide exerts its renal protective effects could uncover new pathways for intervention. Research focusing on its anti-inflammatory and anti-fibrotic properties may provide insights into how semaglutide could be used to mitigate the progression of chronic kidney disease (CKD) beyond its effects on diabetes and obesity.
Longitudinal Studies on Kidney Health
One of the most critical areas for future research involves longitudinal studies tracking the long-term impact of semaglutide on kidney function. While current data suggest potential benefits, comprehensive studies spanning years, if not decades, are necessary to fully understand the extent to which semaglutide can prevent or slow the progression of CKD, particularly in patients with diabetic nephropathy. These studies will also be crucial in identifying any long-term renal risks associated with semaglutide use, ensuring a balanced and informed approach to its prescription.
Comparative Effectiveness Research
As the therapeutic landscape continues to evolve, comparative effectiveness research (CER) will play a pivotal role in positioning semaglutide within the broader context of diabetes and obesity management options. CER focusing on semaglutide versus other GLP-1 receptor agonists, SGLT2 inhibitors, and traditional therapies will help delineate its relative advantages and disadvantages, guiding clinicians in personalized treatment decision-making.
Exploration of New Indications
The versatility of semaglutide, evidenced by its impact on weight management and glycemic control, raises the question of its potential in treating other conditions. Future research may explore its application in non-alcoholic fatty liver disease (NAFLD), cardiovascular diseases, and even certain forms of cancer where obesity and metabolic dysregulation play a role. Investigating these possibilities could expand the therapeutic reach of semaglutide, offering new hope to patients with these conditions.
Patient-Centered Outcomes Research
Finally, patient-centered outcomes research will be vital in tailoring semaglutide treatment to individual needs and preferences. Understanding patient experiences, quality of life changes, and adherence factors will enhance the practical application of semaglutide, making its use more effective and patient-friendly. This research will also inform the development of support systems and educational resources to maximize treatment benefits for patients.
The future of semaglutide research holds the promise of not only enhancing our understanding of its benefits and risks but also broadening its therapeutic applications. By pursuing these avenues of research, the medical community can continue to refine and expand the use of semaglutide, improving outcomes for patients with diabetes, obesity, and potentially other conditions linked to metabolic dysregulation.
Section 11: Conclusion
The exploration of semaglutide’s impact on kidney function within the broader scope of its therapeutic benefits for individuals with type 2 diabetes and obesity has unveiled a complex and promising landscape. As we have navigated through the multifaceted aspects of semaglutide’s effects, from its significant potential in glycemic control and weight management to its implications for kidney health and beyond, a nuanced understanding of this medication emerges. This conclusion seeks to encapsulate the key insights gleaned from our journey, highlighting the critical takeaways and the forward path in optimizing semaglutide’s use in clinical practice.
Semaglutide represents a paradigm shift in managing conditions traditionally fraught with complications and limited therapeutic options. Its efficacy in lowering blood glucose levels and facilitating weight loss has been well documented, underscoring its value as a versatile tool in the treatment arsenal against diabetes and obesity. Furthermore, the potential renal benefits of semaglutide, including its protective effects against the progression of diabetic nephropathy, offer a beacon of hope for patients at risk of chronic kidney disease (CKD). However, the medication’s journey from a novel therapeutic agent to a cornerstone of treatment is marked by the need for vigilance regarding its renal implications.
The importance of comprehensive monitoring strategies cannot be overstated, as they ensure that patients derive the maximum benefit from semaglutide while mitigating potential risks. Baseline assessments and regular follow-ups are crucial in identifying any adverse effects on kidney function early, allowing for timely interventions. Moreover, the individualization of treatment, considering each patient’s unique health profile and risk factors, is paramount in leveraging semaglutide’s benefits fully.
Looking ahead, the horizon of semaglutide research promises to expand our knowledge further, exploring not only its long-term effects on kidney health but also its potential applications in addressing other conditions associated with metabolic dysregulation. Comparative effectiveness research will continue to refine its place within the therapeutic landscape, guided by a commitment to patient-centered outcomes and evidence-based practice.
In conclusion, semaglutide stands as a significant advancement in the management of type 2 diabetes and obesity, with promising implications for kidney health. As we move forward, the integration of ongoing research, personalized treatment approaches, and vigilant monitoring will be key in harnessing its full potential. The journey of semaglutide, from a promising therapeutic agent to a mainstay of treatment, reflects the evolving nature of medical science—a journey marked by continuous learning, adaptation, and an unwavering focus on patient well-being. Click to learn about the exclusionary conditions for our semaglutide program!
Section 12: Research Citations
The investigation into semaglutide’s impact on kidney function, alongside its broader implications for treating type 2 diabetes and obesity, is underpinned by a wealth of clinical research and scientific inquiry. This section aims to collate and reference key studies, reviews, and clinical trials that have been instrumental in shaping our current understanding of semaglutide. These citations not only provide a foundation for the insights shared throughout this article but also serve as a resource for healthcare professionals, researchers, and patients seeking to delve deeper into the evidence behind semaglutide’s therapeutic potential and safety profile.
- Semaglutide and Glycemic Control: A landmark study by Marso, S.P., et al., published in the New England Journal of Medicine, demonstrated the efficacy of semaglutide in reducing HbA1c levels in patients with type 2 diabetes, highlighting its superior performance compared to placebo and other antidiabetic agents.
- Weight Management Benefits: The SUSTAIN-6 trial, as reported in the Lancet, explored the cardiovascular and metabolic outcomes of semaglutide treatment, including significant weight loss among participants, underscoring its dual benefit for patients with diabetes who are also battling obesity.
- Renal Protective Effects: A comprehensive review by Heerspink, H.J.L., et al., in the Journal of the American Society of Nephrology, delved into the potential renal benefits of GLP-1 receptor agonists like semaglutide, suggesting a promising avenue for CKD prevention and management in the diabetic population.
- Cardiovascular Outcomes: The cardiovascular outcomes trial for semaglutide, known as SUSTAIN-6, provided robust evidence of its cardioprotective benefits, reducing the risk of major adverse cardiovascular events in a high-risk diabetic population. This study, published in the New England Journal of Medicine, has been pivotal in positioning semaglutide as a preferred option for patients with cardiovascular concerns.
- Comparative Effectiveness Research: A meta-analysis by Ahmann, A.J., in Diabetes, Obesity and Metabolism, compared the efficacy and safety of semaglutide with other GLP-1 receptor agonists and SGLT2 inhibitors, offering valuable insights into its relative performance and patient selection criteria.
- Long-Term Safety and Efficacy: The ongoing commitment to understanding semaglutide’s long-term impact is exemplified by extension studies and post-marketing surveillance reports, which continue to monitor its effects on kidney function, cardiovascular health, and overall safety in diverse patient populations.
These citations represent just a fraction of the extensive body of research on semaglutide, each contributing valuable insights into its mechanisms of action, therapeutic benefits, and potential risks. For healthcare providers and patients alike, staying informed of the latest evidence is crucial for making informed decisions about incorporating semaglutide into treatment plans. As research progresses, the expanding literature on semaglutide will undoubtedly continue to refine our understanding and application of this significant therapeutic agent.
Questions and Answers: Semaglutide and kidney function
Semaglutide has been studied for its safety and efficacy in individuals with type 2 diabetes, some of whom had varying degrees of kidney disease. Clinical trials, such as those referenced in earlier sections, suggest that semaglutide can be used safely in patients with mild to moderate kidney disease, with careful monitoring. It’s important to adjust the dosage according to renal function and closely monitor any changes in kidney health throughout the treatment.
Research indicates that semaglutide may have beneficial effects on kidney function in diabetic patients, particularly in slowing the progression of diabetic nephropathy. By improving glycemic control and reducing blood pressure and body weight, semaglutide can indirectly contribute to kidney health. However, direct improvements in kidney function, such as reversal of existing kidney damage, require further study.
While semaglutide is generally well-tolerated, patients should be aware of potential signs of kidney issues, such as reduced urine output, swelling in the legs or feet, and unexplained fatigue. These symptoms could indicate worsening kidney function, necessitating immediate medical evaluation to adjust treatment as necessary.
Semaglutide, similar to other GLP-1 receptor agonists, shows promise in providing renal protective effects in addition to its metabolic benefits. Comparative studies have begun to evaluate these agents side by side, with semaglutide often showing superior efficacy in glycemic control and weight loss, which indirectly benefits kidney health. Direct comparisons on renal outcomes are still an area of ongoing research.
Long-term studies are crucial for understanding the full impact of semaglutide on kidney health. While initial data from trials like SUSTAIN-6 provide insights into cardiovascular and renal outcomes, ongoing studies aim to offer more definitive evidence on long-term kidney effects. These studies will help clarify the duration and magnitude of semaglutide’s renal benefits and risks.
The frequency of kidney function testing should be individualized based on the patient’s baseline renal health, the presence of coexisting conditions, and the overall risk of kidney disease progression. Generally, monitoring kidney function every 3 to 6 months is recommended, with more frequent assessments for patients with existing kidney disease or those who exhibit symptoms of renal impairment during treatment.
There is no direct evidence to suggest that semaglutide causes kidney failure in patients without pre-existing severe kidney disease. However, like any medication, it can have side effects that, if not managed properly, may contribute to renal stress. For example, the medication can cause dehydration due to gastrointestinal side effects, which, in turn, could potentially affect kidney function. It’s crucial for patients to stay hydrated and for healthcare providers to monitor renal function closely, especially in those with existing kidney disease, to mitigate any risks.
Yes, weight loss has been shown to have several benefits for kidney health, particularly in patients with obesity-related kidney disease. Reducing body weight can decrease the workload on the kidneys, reduce blood pressure, and improve metabolic parameters, all of which contribute to a lower risk of chronic kidney disease progression. Since semaglutide is effective in promoting weight loss, it can indirectly benefit kidney health through these mechanisms.
For patients with renal impairment, several precautions should be taken when using semaglutide. These include starting at a lower dose and gradually increasing it based on tolerance and renal function, closely monitoring kidney function before and during treatment, and being vigilant for signs of worsening renal function. It’s also important to ensure adequate hydration and to adjust the dosage or discontinue the medication as needed, based on the patient’s response and any side effects experienced.
The effects of semaglutide on kidney function, particularly any adverse effects, are generally reversible upon discontinuation of the medication, especially if identified early. This underscores the importance of regular monitoring of kidney function in patients taking semaglutide. If renal function declines, prompt adjustment of the treatment regimen can help prevent permanent kidney damage. However, the potential long-term benefits of semaglutide on slowing the progression of diabetic nephropathy may represent a lasting positive impact on renal health.

