Table of Contents
Introduction
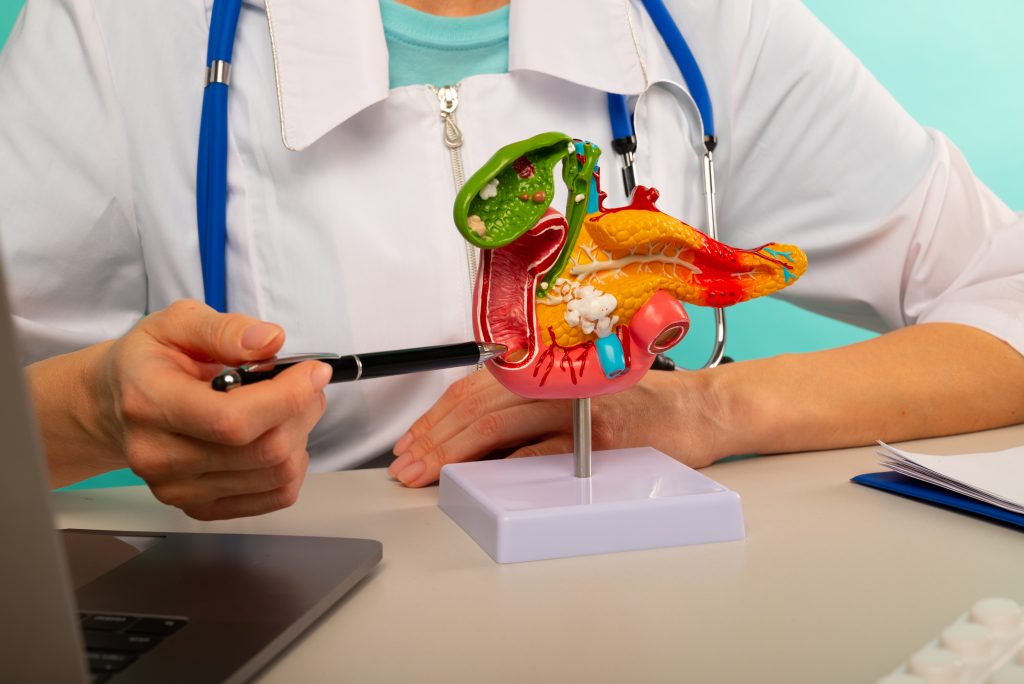
Gallbladder removal, or cholecystectomy, is a common surgical procedure primarily performed to relieve the severe pain and complications caused by gallstones or other gallbladder conditions. The gallbladder, a small organ beneath the liver, stores bile—a digestive fluid essential for breaking down fats. When the gallbladder is inflamed, infected, or blocked by gallstones, it can lead to significant digestive discomfort and necessitate its removal.
Cholecystectomy is performed millions of times worldwide each year, effectively resolving gallbladder issues. However, many individuals experience changes in digestion and weight management after the procedure, with weight loss being a frequent outcome. This weight loss can result from various physiological changes and lifestyle adjustments following surgery.
To understand weight loss post-gallbladder removal, it’s crucial to grasp the gallbladder’s role in digestion. Bile, produced by the liver and stored in the gallbladder, is released into the small intestine when fatty foods are consumed, aiding in fat digestion and absorption. Without a gallbladder, bile drips continuously into the intestine, disrupting the delicate balance of fat digestion and absorption.
Moreover, changes in bile flow and composition after cholecystectomy can impair the absorption of essential nutrients, leading to potential malnutrition. This disruption, along with altered appetite regulation and metabolism, can significantly influence weight post-surgery.
This article explores the complex phenomenon of weight loss after gallbladder removal, providing practical insights and strategies to manage these changes effectively. By examining the physiological shifts that occur post-surgery, we aim to equip individuals with the knowledge to navigate their health and well-being.
We will delve into the digestive changes that occur without a gallbladder, identify the key factors driving post-surgery weight loss, discuss common challenges, and offer evidence-based strategies for healthy weight management. Additionally, we will cover medical interventions, lifestyle changes, and the importance of long-term health monitoring to ensure comprehensive care for those who have undergone cholecystectomy.
This guide is designed for individuals who have had their gallbladder removed, healthcare professionals involved in their care, and anyone interested in understanding the complexities of weight management after cholecystectomy. By addressing the unique challenges and opportunities posed by post-surgery physiology, we aim to support individuals in achieving and maintaining optimal health and quality of life.
Understanding Digestion Without a Gallbladder
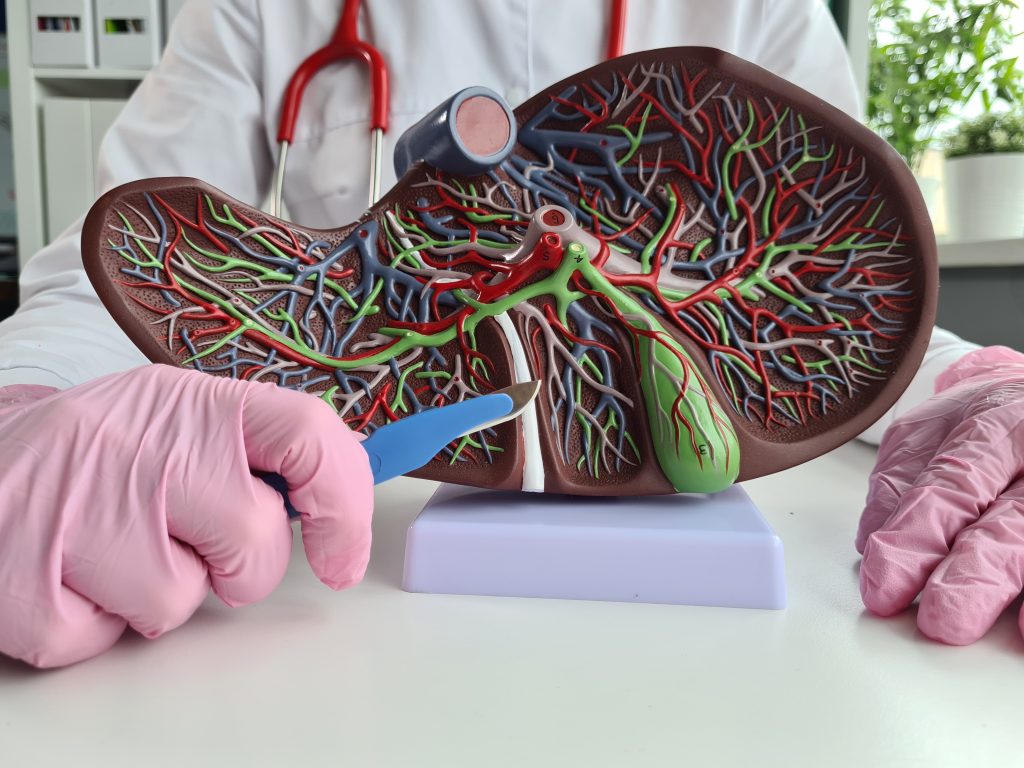
Digestion is a vital process that transforms food into nutrients and energy. Central to this is bile, a digestive fluid produced by the liver and typically stored in the gallbladder. Bile, composed of bile salts, cholesterol, bilirubin, and phospholipids, plays a crucial role in breaking down and absorbing fats.
In a normal digestive system, the gallbladder stores and concentrates bile, releasing it into the small intestine when fatty foods are consumed. This release is triggered by the hormone cholecystokinin (CCK), which signals the gallbladder to contract. The bile then emulsifies fats, making them easier to digest and absorb. This process is also vital for the absorption of fat-soluble vitamins such as A, D, E, and K.
However, when the gallbladder is removed, the liver continuously drips bile into the small intestine. This can disrupt the digestion of fats, leading to symptoms like bloating, gas, diarrhea, and abdominal discomfort, collectively known as post-cholecystectomy syndrome (PCS). The absence of a gallbladder also alters bile composition and flow, potentially impairing the digestion and absorption of fats and fat-soluble vitamins, increasing the risk of nutritional deficiencies over time.
Beyond fat digestion, bile influences broader metabolic processes. It activates receptors that regulate lipid and glucose metabolism, appetite, and energy expenditure. Therefore, changes in bile acid metabolism after gallbladder removal can have significant implications for overall metabolic health and weight management.
Effectively managing digestion without a gallbladder requires understanding these changes. Individuals who have undergone gallbladder removal can benefit from dietary modifications, such as reducing fat intake immediately after surgery and gradually reintroducing healthy fats like those found in avocados, nuts, seeds, and fatty fish. These adjustments can support digestion and minimize discomfort.
Healthcare providers may also recommend bile acid sequestrants or digestive enzyme supplements to aid in fat digestion. These treatments bind to bile acids or provide enzymes to improve fat breakdown and absorption, though their effectiveness can vary, emphasizing the need for personalized care plans.
Managing digestion post-cholecystectomy involves recognizing and addressing the challenges of altered bile metabolism. With targeted dietary adjustments, supplementation, and ongoing medical support, individuals can achieve better symptom control and maintain their nutritional health after gallbladder removal, ultimately enhancing their quality of life.
Key Factors Contributing to Weight Loss After Gallbladder Removal
Weight loss after gallbladder removal, or cholecystectomy, is common and driven by several interconnected physiological and lifestyle factors. Recognizing these elements is vital for managing weight and promoting overall health in individuals post-surgery.
Disruption of Bile Flow and Metabolism
The gallbladder is crucial for bile storage and release, which is essential for digesting and absorbing fats. Without the gallbladder, bile is released directly from the liver into the small intestine, disrupting the normal flow and composition of bile. This disruption can impair fat digestion, leading to malabsorption, reduced caloric intake, and subsequent weight loss. Additionally, symptoms like bloating, gas, and diarrhea may arise from inefficient fat digestion, further impacting nutrient absorption and appetite.
Altered Appetite Regulation and Gut Hormone Signaling
Cholecystokinin (CCK), a hormone that stimulates gallbladder contraction and bile release in response to fat ingestion, also promotes feelings of fullness. After cholecystectomy, the absence of this regulatory mechanism may disrupt appetite control, leading to changes in eating behaviors and contributing to weight loss.
Impact on Gut Microbiota
The gut microbiota, which plays a critical role in digestion, nutrient absorption, and energy regulation, can be altered after gallbladder removal. Changes in the composition and function of gut bacteria may affect metabolism and energy balance, influencing weight management. Dysbiosis, or an imbalance in gut microbiota, is linked to metabolic disorders, including weight gain and obesity, and may affect weight loss after surgery.
Lifestyle and Dietary Adjustments
Many individuals modify their diets after cholecystectomy, often reducing the intake of fatty or greasy foods to avoid discomfort. While these adjustments may ease symptoms, they can also lead to unintended weight loss if alternative nutrient sources are not adequately incorporated.
Psychological and Emotional Factors
Stress, anxiety, and emotional eating may also play significant roles in weight changes post-surgery. The stress of undergoing surgery and concerns about future health can affect eating patterns and adherence to dietary recommendations, influencing weight outcomes.
Weight loss after gallbladder removal results from a complex interaction of physiological changes, dietary adjustments, and psychological factors. Healthcare providers must understand these factors to create personalized strategies that address the unique challenges faced by individuals post-cholecystectomy. By focusing on managing physiological changes, encouraging healthy eating habits, and addressing psychological well-being, healthcare providers can help patients achieve and maintain a healthy weight after gallbladder removal.

Common Challenges and Complications After Gallbladder Removal
Post-cholecystectomy syndrome (PCS) can significantly impact patients after gallbladder removal. Despite the surgery often being performed to relieve symptoms like gallstones or biliary colic, some patients continue to face digestive issues or develop new symptoms. A thorough understanding of PCS is crucial for healthcare providers to offer effective management and support.
Persistent and New Abdominal Pain
Abdominal pain is a key symptom of PCS, often mirroring pre-surgery discomfort or manifesting as new pain. This pain typically localizes in the upper right abdomen and may be accompanied by bloating, gas, and indigestion. The underlying cause of PCS-related pain varies, potentially involving bile reflux, sphincter of Oddi dysfunction, or leftover gallstones or bile duct stones.
Gastrointestinal Distress
PCS often brings gastrointestinal symptoms such as nausea, vomiting, and diarrhea. Diarrhea is particularly common and is linked to changes in bile flow and composition, leading to impaired fat digestion and malabsorption. These symptoms can disrupt daily life and reduce overall quality of life.
Nutritional Deficiencies
Patients with PCS are at an increased risk of nutritional deficiencies, especially in fat-soluble vitamins like A, D, E, and K, due to impaired fat absorption. Deficiencies in these vitamins can result in serious health issues, including bone disorders, vision problems, and weakened immune function. It’s vital for healthcare providers to monitor for these deficiencies and recommend appropriate supplementation.
Psychological Impact
The psychological toll of PCS should not be overlooked. Ongoing symptoms can lead to anxiety, depression, and frustration, which in turn can affect treatment adherence and overall well-being. Addressing these mental health challenges is essential for comprehensive care.
Multidisciplinary Management
Effective management of PCS requires a multidisciplinary approach. Dietary changes, such as reducing fat intake and avoiding trigger foods, can alleviate symptoms. Bile acid sequestrants or digestive enzyme supplements may be prescribed to aid fat digestion and control diarrhea.
For patients with severe or persistent symptoms unresponsive to conservative treatment, further diagnostic evaluation, including ERCP, MRCP, or other imaging studies, may be necessary. These assessments help identify residual stones, bile duct strictures, or other complications. In select cases, surgical interventions like sphincterotomy or revisional surgery may be required to address specific issues.
PCS presents a complex array of challenges that require vigilant and personalized care. By adopting a multidisciplinary approach, healthcare providers can effectively manage PCS, improve symptoms, and enhance the quality of life for individuals after gallbladder removal.
Strategies for Effective Weight Loss After Gallbladder Surgery
Weight management after gallbladder removal demands a focused, strategic approach, combining diet, lifestyle, and behavioral changes. By embracing evidence-based methods customized to your specific needs, you can effectively control your weight post-surgery and enhance your overall health.
Adopt a Balanced, Nutrient-Rich Diet
Post-surgery, a well-rounded diet is crucial for optimal digestion and nutrient absorption. While avoiding fats entirely may seem tempting, it’s vital to include healthy fats in moderation. Focus on sources of monounsaturated and polyunsaturated fats, like avocados, nuts, seeds, olive oil, and fatty fish. These not only ease digestion but also support heart health.
Prioritize fiber-rich foods such as fruits, vegetables, whole grains, and legumes. These promote fullness, regulate blood sugar, and support digestive health. Fiber also helps bulk up stools, promoting regular bowel movements—an essential factor if you’re experiencing gastrointestinal symptoms after surgery.
Lean on Protein
Incorporate lean proteins like poultry, fish, tofu, legumes, and low-fat dairy. Protein aids in muscle repair and maintenance, and it also enhances feelings of fullness, helping to reduce overall calorie intake. Including protein in each meal stabilizes blood sugar levels and prevents overeating.
Practice Portion Control
Mindful eating is key to preventing overeating. Pay close attention to hunger and fullness cues, eat slowly, and savor each bite. Consider using smaller plates to help control portion sizes and prevent overindulgence.
Stay Hydrated
Proper hydration is fundamental to weight management and overall well-being. Water supports digestion, nutrient absorption, and metabolism. Aim for consistent water intake throughout the day, and steer clear of sugary drinks and alcohol, which can derail your weight loss goals. Opt for water, herbal teas, or water infused with fruits and herbs for a refreshing twist.
Engage in Regular Physical Activity
Physical activity is a cornerstone of effective weight management. Engage in both cardiovascular exercises (like walking, cycling, or swimming) and strength training (like weightlifting or bodyweight exercises) to build muscle and support fat loss.
Incorporate physical activity into your daily routine by choosing activities you enjoy and sticking with them. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week, alongside muscle-strengthening exercises on two or more days. Remember, every bit of movement counts—take the stairs, walk during breaks, and stay active throughout the day.
Implement Behavioral Strategies
Mindful eating and keeping a food diary can significantly enhance your weight loss efforts. By tracking your eating habits and recognizing patterns, you can make informed adjustments to support your goals.
Seek Professional Support
Consult with healthcare professionals like dietitians, nutritionists, or weight loss counselors. They can offer personalized guidance, support, and accountability, helping you achieve and maintain a healthy weight while improving your overall well-being.
Take Charge of Your Health
By following these targeted strategies—balanced nutrition, regular exercise, portion control, hydration, and behavioral adjustments—you can successfully manage your weight post-surgery and enjoy a healthier, more vibrant life. Take action now to make lasting changes for your well-being.
Medical Interventions for Post-Cholecystectomy Weight Loss
After gallbladder removal, lifestyle changes are essential for weight management, but some individuals may require medical interventions to enhance their efforts. These include pharmaceutical options and, in some cases, surgical procedures. Understanding these interventions is crucial for both healthcare providers and patients after cholecystectomy.
Pharmaceutical Interventions
One effective pharmaceutical approach for weight management post-gallbladder removal is the use of medications targeting appetite regulation and energy metabolism. A leading class of these medications is GLP-1 (glucagon-like peptide-1) receptor agonists. These drugs mimic GLP-1, a hormone that stimulates insulin secretion, reduces appetite, and slows gastric emptying.
Semaglutide, a prominent GLP-1 receptor agonist, has demonstrated significant efficacy in promoting weight loss, especially in individuals with obesity or overweight conditions. Clinical trials have shown that semaglutide, administered as a once-weekly injection, leads to substantial and sustained weight reduction. Its mechanism—reducing food intake, enhancing satiety, and improving glycemic control—makes it a promising option for weight management after cholecystectomy.
However, using semaglutide in individuals without a gallbladder warrants careful consideration. GLP-1 receptor agonists slow gastric emptying and suppress appetite, which may alter gastrointestinal motility and nutrient absorption in post-cholecystectomy patients. These changes could affect food tolerance and nutrient uptake, posing potential challenges.
Moreover, there is limited research specifically focusing on semaglutide’s effects in individuals without a gallbladder. Healthcare providers should therefore prescribe it cautiously, closely monitoring for adverse effects or complications. It’s imperative to assess each patient’s medical history, underlying conditions, and dietary habits before initiating semaglutide therapy.
Potential Side Effects and Considerations
Patients considering semaglutide or other GLP-1 receptor agonists should be informed about possible side effects, including nausea, vomiting, diarrhea, and pancreatitis. Additionally, these medications may interact with other drugs or supplements, necessitating a thorough review of current medications with a healthcare provider before beginning treatment.
Surgical Interventions
For individuals with severe obesity or obesity-related health conditions unresponsive to lifestyle and medical interventions, surgical options may be considered. Bariatric surgery, including gastric bypass or sleeve gastrectomy, is a viable option that can significantly reduce calorie intake and lead to improved weight loss outcomes.
Bariatric surgery works by either limiting the stomach’s capacity or altering the digestive process, thereby facilitating weight loss. While it can be highly effective, the procedure is not without risks. Patients considering bariatric surgery must undergo a comprehensive evaluation to determine their suitability and fully understand the potential benefits and risks.
Medical interventions, including pharmaceutical options like semaglutide and surgical procedures such as bariatric surgery, can be effective in managing weight after gallbladder removal. However, their use in post-cholecystectomy patients requires careful consideration and close monitoring. Healthcare providers should collaborate with patients to develop personalized treatment plans that address individual needs while minimizing risks and optimizing outcomes.
Lifestyle Modifications for Optimal Health Post-Gallbladder Removal
After gallbladder removal, adopting specific lifestyle modifications is essential for achieving and maintaining healthy weight management and overall well-being. These changes, which include adjusting meal timing, increasing physical activity, managing stress, and improving sleep habits, can significantly enhance recovery and long-term health.
Establish Regular Meal Timing
Consistent meal timing is crucial. Eating every 3-4 hours helps regulate appetite, stabilize blood sugar, and prevent overeating. Skipping meals can lead to erratic eating and increased hunger later, which may result in overeating. Ensure each meal is well-balanced, with portion sizes controlled to prevent excessive calorie intake. Use simple visual cues, like comparing portions to the size of your palm, to keep servings in check.
Practice Mindful Eating
Mindful eating is vital for weight management. Focus on the eating experience: chew thoroughly, savor the flavors, and be present at the moment. Avoid distractions like television or phones, as they can lead to mindless eating and overeating. This approach not only enhances digestion but also helps you recognize when you’re full, preventing unnecessary calorie intake.
Prioritize Regular Physical Activity
Engaging in regular physical activity is a cornerstone of post-cholecystectomy health. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous activity each week, coupled with strength training exercises twice a week. Activities like walking, jogging, cycling, or swimming boost cardiovascular health and support weight maintenance. Choose exercises you enjoy to ensure consistency.
Manage Stress Effectively
Chronic stress can derail weight management efforts by increasing cortisol levels, which stimulate appetite and promote fat storage. Incorporate stress-reducing practices into your daily routine, such as yoga, meditation, deep breathing, or spending time in nature. Managing stress effectively helps prevent emotional eating and promotes overall well-being.
Ensure Quality Sleep
Adequate sleep is a key component of weight management and overall health. Aim for 7-9 hours of quality sleep each night. Establish a relaxing bedtime routine, avoiding stimulants like caffeine and electronic devices close to bedtime. Good sleep hygiene not only supports weight management but also enhances mood, energy levels, and overall health.
Maintain Proper Hydration
Staying hydrated is essential for digestion, nutrient absorption, and overall well-being. Drink plenty of water throughout the day, and listen to your body’s thirst signals. Limit sugary drinks and alcohol, as they can add unnecessary calories and hinder weight loss efforts.
Take Action for Long-Term Health
These lifestyle modifications are not just temporary adjustments; they should be personalized and adopted as part of a long-term commitment to your health. By incorporating regular meal timing, portion control, mindful eating, physical activity, stress management, adequate sleep, and proper hydration into your daily routine, you can optimize your recovery and improve your quality of life after gallbladder removal. Take charge of your health today and make these practices an integral part of your journey to well-being.
Long-Term Health Monitoring After Gallbladder Removal
Long-term health monitoring is crucial for anyone who has undergone gallbladder removal to ensure optimal recovery and prevent complications. Regular follow-ups with healthcare providers are vital for assessing overall health, tracking weight, evaluating nutritional status, and adjusting care strategies as needed.
Key Focus Areas in Long-Term Monitoring
- Weight Management:
Post-cholecystectomy, weight changes are common—some individuals may lose weight due to altered digestion, while others might gain due to dietary habits or underlying conditions. Regular weight checks allow healthcare providers to detect concerning trends early and intervene when necessary. - Nutritional Assessment:
The gallbladder plays a role in fat absorption, which is essential for processing fat-soluble vitamins (A, D, E, K). Without it, deficiencies may occur. Regular blood tests can help detect these deficiencies, and healthcare providers can recommend appropriate supplementation. - Symptom Monitoring:
Many patients experience gastrointestinal issues post-surgery, such as bloating, gas, diarrhea, or nausea. Persistent symptoms can impact daily life and well-being. Healthcare providers should conduct thorough evaluations to determine the cause and provide effective management strategies. - Lifestyle Guidance:
Follow-up visits provide an opportunity for healthcare providers to reinforce healthy habits, such as balanced eating, regular physical activity, and stress management. These visits are also a chance to address patient concerns and provide ongoing support. - Complication Surveillance:
Although rare, complications like bile duct injuries or bile leakage can occur after gallbladder removal. Early detection through regular monitoring can prevent these issues from becoming serious.
Active Patient Involvement
Patients should take an active role in their health monitoring by:
- Maintaining open communication with healthcare providers.
- Attending all follow-up appointments.
- Reporting any new or persistent symptoms immediately.
- Tracking their diet, exercise, and overall health.
By prioritizing long-term health monitoring and staying engaged in their care, patients can proactively manage their health and well-being, ensuring the best possible outcomes after gallbladder removal.
Conclusion
Weight management after gallbladder removal is a complex challenge that demands a strategic, holistic approach. The physiological changes post-surgery—such as altered digestion, nutrient absorption, and appetite regulation—can be effectively managed with the right strategies. By adopting specific dietary adjustments, making lifestyle changes, and considering medical interventions when necessary, individuals can maintain a healthy weight and enhance their overall well-being.
This article has explored the critical aspects of post-cholecystectomy weight management. We’ve detailed how changes in bile metabolism and gastrointestinal function impact digestion and how tailored dietary modifications can support nutrient absorption. Understanding these digestive changes is vital for optimizing post-surgery health.
Lifestyle modifications play a pivotal role in this journey. Regular physical activity, stress management, and mindful eating are essential practices that not only aid in weight control but also improve quality of life after gallbladder removal. These practices should be an integral part of the daily routine for those seeking to maintain their health post-surgery.
For some, medical interventions might be necessary. Options like GLP-1 receptor agonists or bariatric surgery offer additional support for weight management. These interventions should be considered within the framework of a comprehensive, personalized care plan, ensuring they align with individual needs and goals.
Long-term health monitoring is crucial. Regular check-ups with healthcare providers enable ongoing assessment of weight, nutritional status, and overall health, helping to prevent complications and optimize outcomes. Active participation in this monitoring process empowers individuals to take charge of their health post-surgery.
In essence, managing weight after gallbladder removal requires a coordinated effort involving dietary changes, lifestyle adjustments, potential medical interventions, and consistent health monitoring. By addressing these elements with personalized, evidence-based strategies, individuals can successfully manage their weight and significantly improve their quality of life.
Collaboration with healthcare providers is key. With the right support and resources, navigating the challenges of post-surgery weight management is not only possible but can lead to sustained health and well-being.
Research Citations:
Certainly, here are some research citations related to weight loss after gallbladder removal:
Shiffman, M. L., Sugerman, H. J., Kellum, J. M., Moore, E. W. (1995). Changes in gallbladder bile composition following gallstone formation and weight reduction. Gastroenterology, 109(2), 545-554.
Buchwald, H., Avidor, Y., Braunwald, E., Jensen, M. D., Pories, W., Fahrbach, K., … & Schoelles, K. (2004). Bariatric surgery: a systematic review and meta-analysis. JAMA, 292(14), 1724-1737.
Padidar, S., Farzaneh, N., Lotfi, M. H., Amini, M., & Ebrahimian, M. (2017). The effect of laparoscopic cholecystectomy on serum lipid parameters. Annals of Medical and Health Sciences Research, 7(1), 44-47.
Everhart, J. E., & Khare, M. (1993). Long-term survival after cholecystectomy: a population-based study. Gastroenterology, 104(3), 1147-1156.
Teng, L., Chen, H. J., Huang, C. C., Lin, J. K., & Lin, T. C. (2017). The risk of cholecystectomy after laparoscopic gastric bypass surgery: a population-based study in Taiwan. Obesity Surgery, 27(1), 96-103.
Fenger, R. V., Stenbæk, J., Vestergaard, E. M., Rosenstock, S., & Jørgensen, L. N. (2018). Laparoscopic cholecystectomy for biliary dyskinesia in the elderly: A systematic review and meta-analysis. Surgical Endoscopy, 32(1), 329-336.
Shiffman, M. L., Sugerman, H. J., Kellum, J. M., & Moore, E. W. (1992). Changes in gallbladder bile composition and crystal detection time following gallstone lithotripsy and dissolution therapy. Hepatology, 16(5), 1295-1302.
Delgado, J. R., Cooper, J. N., Liu, D. C., Kelleher, C. M., Brindle, M. E., Deans, K. J., & Minneci, P. C. (2020). Cholecystectomy rates in children with short bowel syndrome: an analysis of the kids’ inpatient database. Journal of Surgical Research, 248, 332-338.
Ruhl, C. E., Everhart, J. E., & The National Institutes of Health Gallbladder Disease Conference Planning Panel. (2003). Gallstone disease is associated with increased mortality in the United States. Gastroenterology, 125(1), 147-155.
Acalovschi, M. (2003). Biliary sludge as a cause of acute pancreatitis. Journal of Gastroenterology and Hepatology, 18(11), 1324-1332.
These citations cover various aspects of weight loss after gallbladder removal, including changes in bile composition, effects of bariatric surgery, alterations in serum lipid parameters, long-term survival post-cholecystectomy, risk factors for cholecystectomy, and complications associated with gallstone disease.
Questions and Answers: Weight loss after gallbladder removal
Weight loss after gallbladder removal can occur due to various factors, including changes in digestion, nutrient absorption, and appetite regulation. The absence of the gallbladder can disrupt the process of fat digestion and absorption, leading to malabsorption of fats and potentially reduced calorie intake. Additionally, alterations in appetite hormones and gastrointestinal motility may influence food intake and energy balance, contributing to weight changes post-surgery.
Weight regain after gallbladder removal is possible but not inevitable. Individuals may experience fluctuations in weight due to factors such as dietary habits, lifestyle choices, and underlying health conditions. By adopting healthy eating habits, regular physical activity, and lifestyle modifications, individuals can maintain a healthy weight and prevent weight regain post-surgery.
Dietary modifications after gallbladder removal may include reducing fat intake, particularly saturated and trans fats, to minimize symptoms such as diarrhea and abdominal discomfort. Focus on incorporating healthy fats from sources such as avocados, nuts, seeds, and fatty fish. Additionally, prioritize fiber-rich foods, lean protein sources, and adequate hydration to support digestive health and overall well-being.
While individuals post-gallbladder removal may tolerate fatty foods differently, it is generally advisable to limit high-fat and greasy foods to prevent digestive symptoms such as diarrhea and bloating. Instead, focus on consuming moderate amounts of healthy fats from sources such as avocados, nuts, seeds, and fatty fish, which provide essential nutrients and support overall health.
Depending on individual needs and dietary habits, healthcare providers may recommend supplements to support nutrient absorption and prevent deficiencies post-gallbladder removal. Common supplements include fat-soluble vitamins (A, D, E, and K), bile acid sequestrants, and digestive enzyme supplements. It is essential to consult with a healthcare provider before starting any new supplements to ensure safety and efficacy.
To prevent digestive symptoms such as diarrhea, bloating, and abdominal discomfort after gallbladder removal, individuals can adopt dietary modifications such as reducing fat intake, avoiding trigger foods, and eating smaller, more frequent meals. Additionally, staying hydrated, practicing mindful eating, and managing stress can help support digestive health and minimize symptoms post-surgery.
While gallbladder removal can affect digestion and nutrient absorption, its impact on metabolism may vary among individuals. Some individuals may experience changes in metabolic rate and energy expenditure post-surgery, while others may not notice significant differences. By adopting healthy lifestyle habits, including regular physical activity and balanced nutrition, individuals can support metabolic health and overall well-being post-gallbladder removal.
Weight loss plateaus are common during any weight loss journey, including post-gallbladder removal. Plateaus occur when the body adjusts to changes in diet and activity levels, resulting in a temporary stall in weight loss progress. To overcome a weight loss plateau, individuals can try adjusting their dietary habits, increasing physical activity, or seeking support from healthcare providers or weight loss professionals.
Some medications, such as GLP-1 receptor agonists like semaglutide, may be prescribed to aid in weight management post-gallbladder removal. These medications work by reducing appetite, promoting satiety, and improving glycemic control, making them a potential option for individuals seeking to manage their weight. However, medication should be used in conjunction with lifestyle modifications and under the guidance of a healthcare provider.
The frequency of follow-up appointments after gallbladder removal may vary depending on individual needs and health status. Generally, individuals may have a follow-up appointment with their surgeon or healthcare provider within a few weeks to assess post-operative recovery and address any concerns. Subsequent follow-up appointments may be scheduled as needed to monitor weight, nutritional status, and overall health. It is essential to communicate with your healthcare provider and attend scheduled appointments to ensure ongoing support and monitoring post-surgery.

Dr. Kevin Kargman
Dr. Kevin J. Kargman is a pediatrician in Sewell, New Jersey and is affiliated with multiple hospitals in the area, including Cooper University Health Care-Camden and Jefferson Health-Stratford, Cherry Hill and Washington Township. (Learn More)
