Table of Contents
Introduction: Understanding Tirzepatide and Its Purpose
Tirzepatide is a prescription medicine used to help adults with type 2 diabetes control their blood sugar. In recent years, it has also been studied for weight management because of its effects on appetite and metabolism. What makes tirzepatide different from other diabetes medications is that it works on two important hormone systems in the body — the glucose-dependent insulinotropic polypeptide (GIP) and the glucagon-like peptide-1 (GLP-1) receptors. These hormones help the body regulate blood sugar after eating and play a role in how full a person feels after meals.
Understanding how to start tirzepatide correctly is important for both safety and effectiveness. This medicine works gradually in the body, and taking too much too soon can cause unpleasant side effects like nausea or stomach upset. On the other hand, starting too slowly or using the wrong schedule can delay progress toward better blood sugar control. This guide is designed to help beginners learn the correct way to start tirzepatide, increase the dose safely, and track their progress over time.
For people new to this medication, one of the first questions is usually, “What dose should I start with?” The answer depends on the manufacturer’s recommendations and a healthcare provider’s evaluation of each person’s needs. Most adults begin with a low weekly dose, which is later increased step by step. The gradual increase helps the body adjust while minimizing side effects. Because tirzepatide stays in the body for several days, it is only taken once a week, usually on the same day each week. This dosing schedule makes it easier for people to stay consistent.
Tirzepatide is part of a newer class of medications that do more than just lower blood sugar. It helps reduce appetite, slows digestion, and supports the pancreas in releasing insulin only when needed. These combined effects make it useful not only for diabetes management but also for improving metabolic health overall. However, it is not suitable for everyone, and it must be used under medical supervision. Some people with certain health conditions — such as a history of pancreatitis or thyroid cancer — may need alternative treatments.
The dosing process is not the same for every person. Factors such as body weight, blood sugar levels, other medications, and individual tolerance all play a role in how dosing is adjusted over time. Healthcare providers usually begin with a standard schedule but may personalize the plan if needed. For example, if a patient experiences nausea after a dose increase, their provider might suggest staying at the same dose a little longer before moving up again. This flexibility helps people continue treatment without discomfort or discouragement.
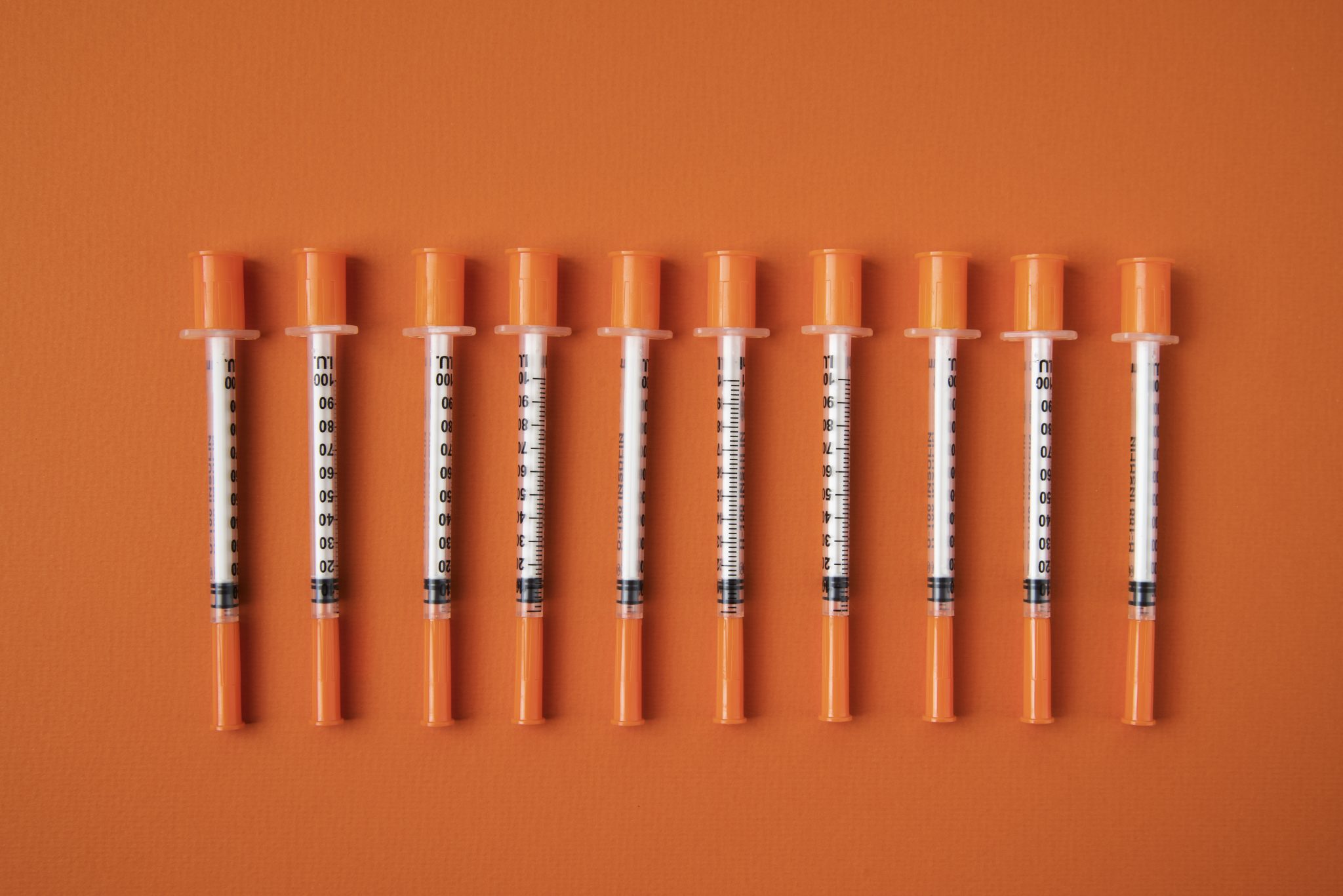
Learning to self-administer tirzepatide injections is another key part of starting this medication. The injection is given under the skin — usually in the abdomen, thigh, or upper arm. The pen device is designed for ease of use, but beginners may still feel nervous about giving themselves an injection. Nurses or pharmacists can provide training and reassurance during the first few doses. Rotating injection sites each week can prevent skin irritation and ensure the medicine is absorbed properly.
Understanding expectations is also important in the first few months. Tirzepatide does not work instantly. Most people notice gradual improvements in their blood sugar levels over several weeks, and weight changes typically appear after a few months of consistent use. During this time, it is important to track results, follow up with healthcare providers, and continue healthy eating and physical activity habits. Medication alone cannot replace lifestyle changes, but it can make them more effective and sustainable.
Because tirzepatide affects both blood sugar and appetite, regular monitoring helps ensure it is working as intended. Doctors may order blood tests such as fasting glucose and hemoglobin A1c every few months to measure progress. These tests provide a clear picture of long-term improvement and help determine whether it is time to adjust the dose.
Finally, patience is essential. Tirzepatide is a long-term treatment, not a quick fix. The goal is to help the body adapt and achieve stable results over time. Missing doses or increasing them too quickly can cause setbacks. Following a step-by-step plan, staying in touch with healthcare providers, and paying attention to how the body responds are the most effective ways to achieve success with tirzepatide.
This beginner’s guide will walk you through the full dosing journey — from the first injection to tracking ongoing results. It will explain how to start safely, when and how to increase the dose, how to handle side effects, and what to expect during treatment. By the end of this guide, you will have a clear understanding of how tirzepatide dosing works and how to use it responsibly for the best possible outcomes.
What Is Tirzepatide and How Does It Work?
Tirzepatide is a prescription medicine that helps people with type 2 diabetes and, in some cases, people who want to manage their weight. It belongs to a group of medicines called incretin-based therapies, which work by helping the body control blood sugar and appetite. What makes tirzepatide special is that it acts on two different hormone pathways in the body, not just one. These hormones are GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1).
Dual Hormone Action: GIP and GLP-1
When we eat, the gut releases hormones that signal the pancreas to release insulin. These hormones, called incretins, tell the body how to handle sugar from food. Tirzepatide mimics the effects of two incretins — GIP and GLP-1 — which makes it a dual agonist.
Here is what each one does:
- GLP-1 helps lower blood sugar by stimulating insulin release when glucose levels rise. It also slows down how fast food leaves the stomach and helps reduce appetite.
- GIP also helps release insulin but works through a slightly different pathway. It may improve how the body uses fat and energy, which can help with weight control.
By combining both of these effects, tirzepatide helps control blood sugar more effectively and supports gradual, healthy weight loss. This dual action gives it a unique advantage compared to medicines that target only GLP-1.
How Tirzepatide Affects Blood Sugar
Tirzepatide works in several ways to help people with type 2 diabetes keep their blood sugar within a healthy range.
- Increases insulin production: It tells the pancreas to release more insulin when sugar levels rise after meals.
- Lowers glucagon levels: It reduces the release of glucagon, a hormone that increases blood sugar, especially between meals.
- Slows stomach emptying: This means food is digested more slowly, preventing large spikes in blood sugar after eating.
- Improves insulin sensitivity: Over time, the body becomes more responsive to insulin, which helps lower glucose levels even further.
Together, these effects help keep blood sugar steady throughout the day, reducing both high spikes and sudden drops.
Effects on Appetite and Weight
One of the most talked-about effects of tirzepatide is its ability to help reduce appetite. People taking it often feel full sooner and stay full longer after eating. This can naturally lead to eating smaller portions and fewer calories.
Tirzepatide also affects brain areas that control hunger and food cravings. This change in appetite is not about willpower — it’s a biological response caused by the medication. Because of this, many people experience gradual, steady weight loss while using tirzepatide, especially when they follow a healthy diet and regular activity plan.
It’s important to understand that tirzepatide is not a “quick fix” for weight loss. It works best as part of a long-term plan that includes medical supervision, balanced nutrition, and consistent follow-up.
Differences from GLP-1–Only Medications
There are other medications, such as semaglutide and liraglutide, that act only on the GLP-1 receptor. Tirzepatide is different because it targets both GIP and GLP-1 receptors at the same time.
This dual mechanism:
- Enhances insulin secretion more effectively.
- Provides greater improvements in blood sugar control.
- May lead to more significant weight reduction in some studies.
Clinical research has shown that tirzepatide often produces larger decreases in HbA1c (a long-term blood sugar measure) and greater average weight loss compared with some GLP-1–only treatments.
However, since it works on two hormones, tirzepatide may also have slightly different side effect patterns, such as mild nausea or stomach upset when doses increase. These effects usually improve over time as the body adjusts.
Therapeutic Goals and Clinical Benefits
The main goals of tirzepatide treatment are to:
- Improve long-term blood sugar control in type 2 diabetes.
- Reduce the risk of diabetes-related complications, such as nerve damage or kidney disease.
- Support gradual and safe weight loss for people who need it.
Clinical studies have shown that many patients using tirzepatide can achieve:
- HbA1c reductions of up to 2% or more.
- Weight reductions of 10–20% of body weight, depending on the dose and duration.
These results are often accompanied by improvements in blood pressure, cholesterol levels, and overall metabolic health.
Tirzepatide helps the body use its natural hormones to better manage blood sugar and appetite. It copies two key gut hormones, GIP and GLP-1, to help the pancreas make insulin when needed, slow digestion, and reduce hunger. The dual-action design makes it an important option for people with type 2 diabetes who want better glucose control and additional benefits like weight management.
Starting Tirzepatide: Recommended Initial Dose
Starting tirzepatide can feel confusing at first, especially if you are new to injectable medicines. Understanding the correct starting dose and how to use it safely is very important. This section explains exactly how to begin treatment, why starting low is important, and how to take your first injections correctly.
What Is the Starting Dose of Tirzepatide?
The recommended starting dose of tirzepatide is 2.5 milligrams (mg) once per week. This means you take one injection every seven days, on the same day each week. For example, if you take your first dose on a Monday, you will continue to inject every Monday after that. The injection can be taken at any time of day, with or without food.
This 2.5 mg starting dose is not meant to control blood sugar or cause significant weight loss right away. Instead, it helps your body get used to the medication. Tirzepatide affects your digestive system and hormones, so beginning at a low dose reduces the chance of side effects such as nausea, vomiting, or stomach upset.
Why Starting Low Is Important
When you first begin tirzepatide, your body is adjusting to how the drug slows digestion and changes how your pancreas releases insulin. A small dose allows your system to adapt gradually.
Starting too high or increasing too quickly can make side effects stronger and harder to manage. The goal of the 2.5 mg dose is to build tolerance, not to reach full treatment strength. Most people stay at this starting dose for the first 4 weeks before increasing to the next level, which is usually 5 mg weekly.
This slow, careful approach helps ensure that your treatment continues safely and comfortably. It also gives your doctor time to check how you are responding before adjusting the dose.
How to Administer the Injection
Tirzepatide is given as a subcutaneous injection, which means the medicine is injected into the fatty layer under your skin. It should never be injected into a vein or muscle.
You can inject tirzepatide into three main areas of your body:
- The stomach (abdomen) — at least two inches away from the belly button.
- The thigh — either the front or outer part of your upper leg.
- The upper arm — this site is easier if someone else gives the injection for you.
It’s important to rotate your injection sites each week. For example, if you inject in your left thigh one week, you might use your right thigh or abdomen the next week. Rotating helps prevent skin irritation, lumps, or soreness in one area.
The injection comes in a single-use prefilled pen. Each pen contains one complete dose and is designed to make injections simple and safe. Most people find that the injection is quick and almost painless. Your healthcare provider or pharmacist can show you exactly how to use the pen before your first dose.
Best Time to Take Tirzepatide
You can take tirzepatide at any time of the day, but it’s best to choose a time that’s easy to remember. Many people set a phone reminder or link their dose day to a regular routine — for example, “every Sunday morning” or “every Wednesday night.”
You should aim to inject the medication on the same day each week. If you ever need to change your dose day, make sure there are at least 3 days (72 hours) between injections. Then you can start your new weekly schedule.
Tips for the First Few Weeks
The first month is about getting used to the medication. Here are some helpful steps to make the process easier:
- Eat smaller meals to reduce nausea.
- Avoid greasy or fried foods, which can make stomach symptoms worse.
- Drink plenty of water throughout the day.
- Take it slow — if you feel mild nausea, give your body time to adjust before making changes.
- Track how you feel in a notebook or app. This helps your healthcare provider understand your progress.
- Do not skip doses unless your doctor tells you to. Staying consistent helps your body adjust properly.
It is also normal if you do not notice major changes in weight or blood sugar during this starting phase. Remember, this stage is about letting your body get used to tirzepatide before increasing to higher doses that deliver stronger effects.
Common Mistakes to Avoid
Many people make small errors when starting tirzepatide. Here are the most common ones to watch out for:
- Skipping doses early on. Missing your weekly injection can make it harder for your body to adapt.
- Increasing the dose too soon. Always follow your healthcare provider’s timeline for dose changes.
- Injecting into the same spot repeatedly. This can cause irritation or small lumps under the skin.
- Storing pens incorrectly. Tirzepatide should be stored in the refrigerator, but you can keep it at room temperature for up to 21 days if needed. Never freeze the pens.
- Forgetting to check the label. Always double-check that you’re using the correct strength and pen before injecting.
The starting dose of tirzepatide is 2.5 mg once weekly. This low beginning helps your body adjust slowly, reduces side effects, and prepares you for dose increases later on. Take your dose on the same day each week, inject it just under the skin, and rotate injection sites regularly. Follow your healthcare provider’s instructions carefully, stay consistent, and be patient — the early weeks are about preparation, not rapid results.

Titration Schedule: How and When to Increase the Dose
One of the most common questions people have when starting tirzepatide is, “When do I increase my dose?”
Understanding when and how to raise your dose safely is a key part of getting good results while avoiding side effects. The process of increasing your dose step by step is called titration. This section explains what titration means, why it’s important, how your doctor decides when to increase, and what you can do to make the process go smoothly.
Why Tirzepatide Doses Increase Gradually
Tirzepatide works by activating two natural hormones in your body called GIP and GLP-1. These hormones help your body control blood sugar, manage appetite, and slow down digestion. While this is helpful for lowering blood sugar and reducing hunger, it can also cause side effects like nausea, bloating, or mild stomach upset when you first start the medication.
Because of this, everyone begins with a small dose. The first few weeks allow your body to adjust to the medication. This slow start helps reduce stomach-related side effects and makes it easier to stick with treatment long term. If your body has time to adapt, you are less likely to feel uncomfortable or have to stop taking the medication early.
Gradual increases also give your healthcare provider time to see how well tirzepatide is working for you. By tracking your blood sugar, weight, and symptoms over several weeks, they can decide whether you are ready for the next step.
The Typical Step-by-Step Dose Schedule
Most people start tirzepatide at 2.5 milligrams once a week. This first dose is not meant to control blood sugar or cause major weight changes. Its main purpose is to let your body get used to the medicine. You will usually stay at this dose for the first four weeks.
After the first month, your doctor may increase the dose to 5 milligrams once a week. If you tolerate this well, you may continue to move up every four weeks in 2.5 milligram steps. The available doses are 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, and 15 mg.
A typical titration might look like this:
- Weeks 1 to 4: 2.5 mg once a week
- Weeks 5 to 8: 5 mg once a week
- Weeks 9 to 12: 7.5 mg once a week
- Weeks 13 to 16: 10 mg once a week
- Weeks 17 to 20: 12.5 mg once a week
- Week 21 and beyond: 15 mg once a week (the maximum dose)
Not everyone will reach the highest dose. Some people feel well-controlled at 5 mg, 7.5 mg, or 10 mg. Your doctor will decide what dose is best for you based on your blood sugar levels, side effects, and overall progress.
How Doctors Decide When to Increase the Dose
Your healthcare provider does not raise the dose automatically after a set number of weeks. Instead, they look at how your body is reacting. The main things they consider are:
- Tolerability: If you are still having a lot of nausea, vomiting, or stomach pain, your provider may wait longer before increasing your dose.
- Blood sugar control: For people with diabetes, blood sugar readings and HbA1c levels show how well the medicine is working.
- Weight progress: For weight management, steady and safe weight loss over time helps guide dose changes.
- Comfort and daily function: If you are tolerating the current dose well and it is effective, your doctor may decide to keep you on that dose longer.
It’s important to remember that there is no rush. Tirzepatide works best when the body has time to adapt. Some people increase every four weeks as planned, but others may stay on a dose for six or even eight weeks before moving up.
Why Slow Titration Is Important
Increasing tirzepatide too quickly can cause uncomfortable side effects. The most common are nausea, vomiting, diarrhea, or bloating. These symptoms are usually mild, but they can become worse if your dose goes up before your body is ready.
By moving slowly, your provider can see how your system responds and make adjustments if needed. If you have side effects, your doctor might recommend staying at your current dose longer or temporarily lowering it. Sometimes just giving your body an extra few weeks at the same dose makes a big difference.
Another reason to go slowly is to avoid dehydration. If nausea or reduced appetite causes you to eat or drink less, it can affect your energy and kidney health. Your provider may suggest increasing fluids and eating smaller, lighter meals during this time.
Tips for Safe and Comfortable Titration
- Follow your provider’s instructions carefully. Never increase your dose on your own.
- Take your injection on the same day each week. Consistency helps your body adjust and prevents missed doses.
- Track your symptoms and progress. Keep notes about how you feel, your appetite, and any side effects.
- Eat smaller meals and avoid greasy foods. This helps reduce nausea during dose changes.
- Stay hydrated. Drink plenty of water throughout the day, especially if your appetite decreases.
- Give your body time. If a higher dose makes you uncomfortable, talk to your provider before taking the next injection.
Tirzepatide titration is not a race — it’s a careful process designed to help you get the most benefit with the fewest side effects. Most people start at 2.5 mg once a week and move up in small steps every four weeks, depending on how they feel and how their blood sugar or weight responds. The highest dose, 15 mg once a week, may be right for some, but not everyone needs it.
The most important thing is to listen to your body and work closely with your healthcare team. Taking your time during titration leads to a smoother experience and more sustainable long-term results.
Managing Side Effects During Dose Escalation
Starting tirzepatide is an important step toward better blood sugar control and weight management. However, like many medicines that affect the digestive system and metabolism, tirzepatide can cause side effects—especially during the first few months or when the dose is increased. Understanding why these side effects happen, what to expect, and how to manage them can help you stay consistent and comfortable with your treatment.
Why Side Effects Happen
Tirzepatide works by mimicking two natural hormones in the body: GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones help regulate how much insulin your body releases, how full you feel after eating, and how slowly food leaves your stomach. Because of these effects, your digestive system and appetite adjust during the early weeks of treatment.
This adjustment period is the main reason why people experience mild side effects. The most common ones involve the stomach and intestines, and they often improve as your body gets used to the medicine.
Common Side Effects
The most frequently reported side effects include:
- Nausea – feeling queasy or sick to your stomach, especially after eating large or fatty meals.
- Vomiting – sometimes occurs if the nausea is severe or if you eat too quickly.
- Diarrhea – loose or watery stools may appear during the first few weeks.
- Constipation – the opposite can also happen, especially as your eating patterns change.
- Loss of appetite – you may feel full faster or have less desire to eat.
These reactions are typically mild to moderate and temporary. They happen because tirzepatide slows how fast food moves through your stomach and affects how your brain signals hunger and fullness.
How to Manage Common Side Effects
Most people can ease discomfort by making small lifestyle changes. Here are some simple and effective strategies:
- Eat smaller meals.
Large meals can worsen nausea or stomach pressure. Instead, eat smaller portions more often throughout the day. - Avoid high-fat or greasy foods.
Fatty foods take longer to digest, which can increase nausea and bloating. Choose lean proteins, whole grains, and vegetables instead. - Stay hydrated.
Drink plenty of water, especially if you experience vomiting or diarrhea. Small sips throughout the day are easier on your stomach than large amounts at once. - Eat slowly and mindfully.
Eating too quickly can trigger nausea or stomach fullness. Take your time, chew food thoroughly, and stop eating when you feel comfortably full. - Avoid lying down after meals.
Wait at least 30 minutes before lying down to help your stomach empty more easily. - Use bland foods if feeling nauseous.
Crackers, toast, bananas, and rice are gentle on the stomach. Avoid spicy or acidic foods until symptoms improve.
When to Pause Dose Increases
The dosing schedule for tirzepatide usually involves increasing the dose every four weeks. However, if you are experiencing ongoing or severe side effects, your doctor may recommend staying on your current dose longer before increasing. This gives your body extra time to adjust.
Do not rush to move up to a higher dose. The goal is to find a balance where you are seeing benefits—such as better blood sugar levels or gradual weight loss—without significant discomfort. Communicate openly with your healthcare provider about any symptoms you experience before changing your dose.
When to Seek Medical Advice
While most side effects are mild, there are times when medical attention is necessary. You should contact your doctor right away if you experience any of the following:
- Severe or ongoing abdominal pain, especially if it spreads to your back (this could be a sign of pancreatitis).
- Persistent vomiting or diarrhea that leads to dehydration (symptoms include dizziness, dry mouth, or dark urine).
- Signs of an allergic reaction, such as rash, swelling, or difficulty breathing.
- Severe constipation that lasts more than a few days and does not improve with hydration or dietary changes.
- Sudden fatigue, yellowing of the skin, or dark urine, which could signal liver or gallbladder problems.
Always let your healthcare team know about any new or worsening symptoms. They may adjust your dose, suggest over-the-counter remedies, or recommend lab tests to ensure your safety.
Tips for Long-Term Comfort
Once your body adapts to tirzepatide, side effects usually fade or become very mild. To maintain comfort in the long run:
- Keep track of your side effects in a notebook or app to share with your healthcare provider.
- Continue healthy eating habits even after side effects improve.
- Remember that consistency is key—taking your injection on the same day each week helps your body maintain balance.
- Never stop the medication suddenly without medical guidance.
Side effects from tirzepatide are common during the first few weeks or after increasing the dose, but they are usually manageable and temporary. With patience, small lifestyle changes, and regular communication with your healthcare provider, most people adjust well to treatment. The focus should always be on steady progress and long-term safety, not rushing to the highest dose.
Monitoring Your Progress: What to Expect in the First 3–6 Months
Starting tirzepatide is an important step toward improving blood sugar control and supporting weight loss. But understanding what to expect and how to track progress is just as important as taking the medication itself. The first few months of treatment are when your body adjusts to the medicine, and most people begin to see noticeable changes. This section will explain what typically happens during the first 3–6 months, what results are realistic, and what to monitor with your healthcare provider.
How Fast Does Tirzepatide Work?
Tirzepatide does not work overnight. It acts gradually as your body adjusts to the incretin hormones it mimics — GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1). These hormones help control blood sugar, slow digestion, and reduce appetite.
In the first few weeks, the goal is not to achieve maximum results but to help your body adapt and avoid side effects. The initial dose (2.5 mg) is often too low to make a big change in blood sugar or weight, but it sets the foundation for future doses to work effectively.
By the second month, after one or two dose increases, many people start to notice:
- Better blood sugar readings, especially fasting glucose levels.
- A reduced appetite or smaller meal portions.
- Slight weight loss, usually a few pounds, depending on diet and activity.
By three to six months, the effects become more consistent. Blood sugar levels often stabilize, and weight loss tends to become more noticeable. Studies have shown that many users see significant improvements within this period, though individual results vary.
What Results Should You Expect?
Blood Glucose Changes
Tirzepatide’s main goal is to improve glucose control. During the first 3–6 months, your doctor may measure your HbA1c — a blood test that shows your average glucose level over three months.
- On average, people can expect a drop in HbA1c by about 1–2% after several months of steady use.
- Fasting glucose readings often decrease gradually, sometimes within the first 4–8 weeks.
Weight Management
Although tirzepatide is not only a weight-loss drug, many people experience weight reduction because it slows digestion and reduces appetite.
- In the first 3 months, you may notice a steady loss of 5–10 pounds.
- By 6 months, weight loss can be more significant if you maintain healthy eating and activity habits.
Remember that results differ for everyone, and progress may slow after the initial months as the body adjusts.
What to Monitor Regularly
Keeping track of certain measurements helps you and your doctor understand how well tirzepatide is working and whether any adjustments are needed.
At Home:
- Fasting blood glucose: Check your morning blood sugar regularly, especially if you have diabetes.
- Body weight: Weigh yourself once or twice a week, ideally at the same time of day.
- Appetite and portion sizes: Note changes in hunger or how quickly you feel full.
- Digestive symptoms: Track any nausea, bloating, or constipation.
At the Clinic:
- HbA1c test: Usually done every 3 months.
- Kidney and liver function tests: Your doctor may check these to ensure the medication is safe for continued use.
- Blood pressure and cholesterol: These often improve with tirzepatide, but regular monitoring is helpful.
Keeping a small journal or using a tracking app can make it easier to share accurate information during medical appointments.
The Role of Medical Follow-Ups
Regular check-ins with your healthcare provider are essential, especially during the first six months. At each visit, your doctor will review:
- Your glucose and weight progress.
- Any side effects or tolerability issues.
- Whether it’s time to increase your dose.
Sometimes, if side effects are bothersome, your provider may recommend staying at the current dose longer before moving up. Never adjust the dose on your own — titration should always be guided by a medical professional.
Supporting Progress with Lifestyle Habits
Tirzepatide is most effective when paired with a healthy lifestyle. Medication helps reduce appetite and control blood sugar, but your daily choices still play a major role.
- Diet: Focus on balanced meals with lean proteins, vegetables, and whole grains. Avoid high-fat or sugary foods that can worsen nausea and slow progress.
- Hydration: Drink plenty of water to ease digestion and reduce constipation.
- Physical activity: Gentle exercise such as walking, cycling, or swimming supports weight management and blood sugar control.
- Sleep: Good sleep helps regulate metabolism and reduces cravings.
Even small, steady lifestyle changes can make tirzepatide more effective and help results last longer.
What If You Don’t See Results Quickly?
Not everyone responds at the same pace. Some people see noticeable changes in the first month, while others need more time, especially if they start with lower doses. Be patient — the medication’s effects build over time.
If progress seems slow after several months, your doctor may:
- Increase your dose (as tolerated).
- Check for other factors such as diet, medication interactions, or hormone levels.
- Review your tracking data to assess patterns in glucose and weight.
Remember: slow, steady improvement is both normal and healthy.
In the first 3–6 months of tirzepatide treatment, progress happens in stages. Early on, your body is learning to adjust to the medicine. With consistent use, monitoring, and support from your healthcare provider, you can expect meaningful changes in blood sugar control, appetite, and overall well-being. Staying patient, tracking your results, and maintaining healthy habits will help you get the most out of your treatment journey.
What to Do If You Miss a Dose or Need to Restart
Starting a medication like tirzepatide can take time to get used to. Because it is given only once a week, it can be easy to forget a dose, especially during the first few months. Understanding what to do when this happens helps keep your treatment safe and effective. It also prevents unnecessary side effects that might happen if the medicine is restarted incorrectly or taken too close together. This section explains, step by step, what to do if you miss a dose, how to return to your schedule, and what happens if you have to stop for a while and start again.
If You Miss a Dose
Tirzepatide is designed to be injected once every seven days. If you miss a dose, the first thing to do is check how much time has passed since your scheduled injection day.
- If it has been less than 4 days (96 hours) since your usual injection time:
You should take the missed dose as soon as you remember. After that, you can return to your regular weekly schedule. For example, if you normally take your injection on Monday morning and remember on Wednesday night, it is still fine to inject it on Wednesday and continue the next dose on the following Monday as usual. - If it has been more than 4 days (over 96 hours) since the missed dose:
It is best to skip that dose entirely and wait until your next scheduled injection. Taking two doses too close together can increase your risk of nausea, vomiting, or other gastrointestinal side effects. It may also raise your chance of low blood sugar, especially if you use other diabetes medicines.
To stay on track, it can help to pick a fixed day each week and connect it with a simple reminder, like a phone alarm or calendar alert. Many people also mark their injection dates on a paper calendar or store their pen in a visible place as a cue.
If You Are Unsure Whether to Take the Dose
Sometimes, you might not remember if you actually gave yourself the injection or not. In that situation, it is safer not to take another dose until you confirm it. If possible, check your injection pen to see if the dose indicator has moved or contact your healthcare provider for advice. Accidentally taking an extra dose may cause unpleasant side effects such as severe nausea or vomiting.
Restarting After Missing Several Doses
If you have missed two or more doses in a row, you should contact your healthcare provider before restarting. The body can lose some of its tolerance to tirzepatide when the medication is stopped for several weeks. Restarting at the same high dose you were on before may increase the risk of strong gastrointestinal symptoms.
In most cases, your healthcare provider will have you restart at a lower dose, often the previous tolerated dose or even the initial 2.5 mg starting dose, and then gradually increase again over several weeks. This process is called re-titration. It allows your digestive system to adjust and helps prevent nausea, stomach pain, or loss of appetite that can happen when the medication is resumed too quickly.
Restarting After Taking a Break
There are times when people intentionally pause tirzepatide — for example, due to surgery, another illness, pregnancy, or cost issues. In these cases, restarting also requires a cautious approach.
Before restarting, discuss with your healthcare provider:
- How long you have been off the medication.
- Your most recent dose before the break.
- Any health changes or new medications you are taking.
- Whether you have experienced significant weight loss or gain during the break.
Your provider may recommend restarting at a lower dose than before or even repeating the full titration schedule. This is especially important if the break lasted more than four weeks, as your tolerance may have changed. A new start gives your body time to adjust again, reduces discomfort, and lowers the chance of gastrointestinal side effects.
How to Safely Resume Your Schedule
Once you have restarted tirzepatide, it helps to re-establish a steady rhythm. Try these tips:
- Choose a consistent injection day that fits your weekly routine.
- Set phone reminders or digital calendar alerts.
- Use a medication tracking app if available.
- Store your injection pens in a visible location (like near your toothbrush or breakfast area) to remind yourself each week.
- Note any side effects or changes in how you feel after restarting, and share them with your healthcare provider during follow-ups.
These small habits can prevent missed doses and make your weekly routine more consistent.
When to Call Your Healthcare Provider
Always contact your healthcare provider if:
- You have missed several doses in a row.
- You are unsure whether to resume your usual dose.
- You experience severe side effects after restarting.
- You have changes in other health conditions, like kidney or liver problems.
Your provider can guide you on whether you need to restart at a lower dose or delay increasing to the next level. They can also help you track your progress safely after any interruption.
Adjusting Doses Based on Individual Response
Tirzepatide is not a “one-size-fits-all” medication. While it follows a standard dosing schedule, each person’s body reacts differently. Some people respond well at lower doses, while others need higher ones to reach their blood sugar or weight goals. Adjusting tirzepatide correctly is important for both safety and effectiveness. This section explains how to know when to change doses, what signs to watch for, and how your healthcare provider makes these decisions.
How to Know if Your Dose Is Working
The main goal of tirzepatide is to help control blood sugar in adults with type 2 diabetes, and for some, to support weight loss. To know whether your dose is working, your healthcare provider will look at several things over time:
- Blood glucose readings: You may check your blood sugar at home, especially if you are using other diabetes medicines. A good response is usually seen as a drop in fasting or post-meal glucose levels within a few weeks.
- HbA1c (A1C) level: This test shows your average blood sugar over the past three months. Your provider will likely measure it every 3 to 6 months. A steady decrease in A1C shows the medicine is helping.
- Weight changes: For many people, tirzepatide also helps with weight loss by reducing appetite and slowing digestion. While weight loss varies, a gradual decrease of 1 to 3 pounds per week is common after the first month.
- Tolerability: Feeling comfortable on your dose is as important as the numbers. If you have frequent nausea or vomiting, it may mean your body needs more time before moving to the next dose.
If your blood sugar remains high, or if you have not seen any progress after several weeks, your healthcare provider may suggest increasing your dose. However, this must always be done carefully and under medical guidance.
When to Maintain or Increase the Dose
The standard dosing plan for tirzepatide increases the amount every four weeks until the desired maintenance dose is reached. Most people begin at 2.5 mg once a week, then go up gradually through 5 mg, 7.5 mg, 10 mg, 12.5 mg, and possibly 15 mg as tolerated.
You may stay longer at a certain level if you still have side effects like nausea, bloating, or fatigue. It is not a race — staying on a lower dose longer can actually help your body adjust and reduce discomfort later on.
Your provider may recommend an increase if:
- Your blood sugar remains above target after several weeks on your current dose.
- You tolerate your dose well with minimal or no side effects.
- You need additional weight control support and are stable on your current level.
- You have no contraindications or medical reasons to stay at a lower dose.
Dose increases should never happen faster than every four weeks unless directed by your healthcare provider. Increasing too quickly can lead to stronger side effects without better results.
Signs the Dose May Be Too High
Just as important as knowing when to increase is recognizing when your dose may be too high. Symptoms that may mean your dose needs to be lowered or paused include:
- Persistent nausea or vomiting that affects your ability to eat or drink.
- Dizziness, weakness, or fatigue that does not improve.
- Dehydration symptoms like dry mouth, dark urine, or rapid heartbeat.
- Ongoing diarrhea or abdominal pain.
- Blood sugar levels that drop too low (hypoglycemia), especially if used with insulin or sulfonylureas.
If you experience these issues, contact your healthcare provider before taking the next dose. They may recommend holding your current dose longer or stepping back to the previous lower dose until your body adjusts.
Individual Factors That Affect Dose Adjustments
Everyone’s medical situation is different. Here are some factors that can affect how your tirzepatide dose is managed:
- Kidney or liver function: People with reduced kidney or liver function may process the medication more slowly. Their dose increases may be spaced farther apart or kept at lower levels.
- Other medications: Some diabetes medications, such as insulin or sulfonylureas, increase the risk of low blood sugar when used with tirzepatide. In those cases, your doctor may reduce those other drugs instead of raising your tirzepatide dose.
- Age and body weight: Older adults or those with lower body weight may need a slower titration plan to avoid nausea or fatigue.
- Medical history: A history of pancreatitis, gallbladder disease, or stomach problems may lead your doctor to use extra caution during dose adjustments.
- Treatment goals: Some people use tirzepatide mainly for glucose control, while others use it primarily for weight management. The dose chosen will depend on which outcome is the main focus.
The Role of Your Healthcare Team
Adjusting tirzepatide is a joint effort between you and your healthcare provider. Regular check-ins allow your provider to review your progress, discuss side effects, and decide whether your current dose is right. Never change your dose on your own, even if you feel you need more or less. Medical supervision helps prevent side effects and ensures the medicine continues to work safely.
You can help your provider by keeping a simple record of your weekly doses, blood sugar readings, weight changes, and any symptoms. Bringing this information to each appointment helps guide dosing decisions more accurately.
Finding the right tirzepatide dose takes time, patience, and teamwork. The goal is to reach a balance — a dose that effectively controls blood sugar and supports healthy weight loss while keeping side effects minimal. By staying in close contact with your healthcare team, tracking your progress, and being honest about how you feel, you can safely reach the dose that works best for your body.
Safety Considerations and Monitoring Parameters
Tirzepatide is an effective medication for managing type 2 diabetes and helping with weight control, but like all prescription drugs, it must be used safely. Understanding the possible risks, knowing what to watch for, and working closely with a healthcare provider can make your treatment both safe and successful. This section explains the main safety points, who should be cautious when using tirzepatide, and what tests or check-ups are important while taking it.
General Safety Overview
Tirzepatide works by mimicking two natural hormones in the body: GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1). These hormones help control blood sugar levels and reduce appetite. Because tirzepatide acts on multiple systems in the body — including the digestive tract, pancreas, and brain — it can cause certain side effects, especially when you first start or increase your dose.
Most people tolerate tirzepatide well when it is introduced slowly. However, safety depends on monitoring your body’s response and reporting any unusual symptoms to your healthcare team.
Important Contraindications and Precautions
Some people should not use tirzepatide, and others need extra caution.
Below are the key medical situations where safety is most important:
- Personal or family history of medullary thyroid carcinoma (MTC):
People with this rare type of thyroid cancer, or with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), should not use tirzepatide. In animal studies, similar drugs caused thyroid tumors. Although this has not been proven in humans, the risk is taken seriously. - History of pancreatitis:
Tirzepatide may raise the risk of inflammation of the pancreas (pancreatitis). Symptoms include severe stomach or upper abdominal pain that may spread to your back, nausea, or vomiting. Anyone with past episodes of pancreatitis should use tirzepatide only under close medical supervision. - Severe gastrointestinal disease:
People with severe stomach or intestinal problems, such as gastroparesis (slow stomach emptying), may not tolerate tirzepatide well. The medicine can slow digestion further and worsen symptoms like bloating or nausea. - Pregnancy and breastfeeding:
There is not enough research on tirzepatide use during pregnancy or breastfeeding. It should only be used if the benefits clearly outweigh potential risks, and only after discussing it with a healthcare professional.
Regular Monitoring and Laboratory Tests
Safe use of tirzepatide requires ongoing monitoring. Doctors usually recommend certain tests and check-ins before and during treatment:
- Blood sugar levels:
Frequent glucose checks help measure how well tirzepatide is controlling diabetes. HbA1c tests every 3–6 months show your average blood sugar over time. - Kidney function (serum creatinine, eGFR):
Nausea, vomiting, or dehydration can sometimes affect kidney function. Monitoring kidney health ensures early detection of problems. - Liver enzymes:
Although rare, some people may develop mild liver enzyme changes. Periodic liver function tests help track any potential issues. - Pancreatic enzymes (amylase and lipase):
Elevated enzyme levels can indicate early signs of pancreatitis. If you experience stomach pain, your doctor may check these levels right away. - Body weight and appetite:
Tracking your weight helps evaluate how well tirzepatide supports your goals and ensures weight loss is occurring safely. - Blood pressure and heart rate:
Some people notice mild changes in heart rate or blood pressure. Regular measurements help ensure these changes stay within a safe range.
Recognizing Warning Signs
Always contact your healthcare provider if you notice any of the following:
- Persistent or severe abdominal pain (especially radiating to the back).
- Continuous nausea, vomiting, or inability to keep fluids down.
- Signs of allergic reaction such as rash, itching, swelling of the face or throat, or difficulty breathing.
- Sudden changes in mood or vision, or symptoms of low blood sugar (shaking, sweating, confusion, fast heartbeat).
- A lump or swelling in the neck that could suggest thyroid changes.
Prompt reporting allows your doctor to adjust your dose, pause treatment, or perform extra tests to ensure safety.
Medication Interactions
Tirzepatide can interact with other medicines, especially those that affect blood sugar or digestion. Common examples include:
- Insulin or sulfonylureas: These may increase the risk of low blood sugar (hypoglycemia). Your doctor might adjust the dose of these medicines when adding tirzepatide.
- Oral medications: Because tirzepatide slows stomach emptying, it can delay absorption of pills taken by mouth. Taking these medicines at a different time of day may help.
- Other GLP-1 receptor agonists: These should not be combined with tirzepatide, as their effects may overlap and cause side effects.
Always share a full list of medications, vitamins, and supplements with your healthcare provider before starting tirzepatide.
Long-Term Safety and Ongoing Studies
Tirzepatide is a relatively new medication, and researchers continue to study its long-term effects. Early data from large clinical trials show strong benefits for blood sugar control and weight loss with a good safety profile. Ongoing studies are evaluating whether tirzepatide may reduce risks for heart disease and other metabolic conditions. For now, continued follow-up with your doctor ensures that any potential long-term effects are monitored.
Staying Safe During Treatment
To stay safe while taking tirzepatide:
- Always inject it exactly as prescribed and on schedule.
- Do not skip follow-up appointments or lab work.
- Tell your healthcare provider if you plan major changes in diet, exercise, or other medications.
- Store the medication properly and never share it with others.
Tirzepatide is a powerful treatment that can improve both blood sugar and weight, but safety depends on consistent monitoring and communication. By following your doctor’s guidance, attending regular check-ups, and watching for warning signs, you can use tirzepatide effectively and reduce the risk of complications. Safe use is not just about taking the right dose — it’s about staying informed, careful, and proactive throughout your treatment journey.

Conclusion: Staying Consistent and Working with Your Healthcare Team
Starting tirzepatide is a big step toward better health, whether your goal is to manage blood sugar, lose weight, or both. Like any long-term treatment, success comes from understanding how the medicine works, how to take it correctly, and how to work closely with your healthcare team. Tirzepatide is a strong medication that affects your body’s natural hormones, so taking time to build good habits and follow your provider’s instructions is the best way to stay safe and see results.
When beginning tirzepatide, remember that progress takes time. The first few weeks are about helping your body adjust to the medicine. The starting dose is always low to lower the chance of stomach side effects like nausea or upset stomach. It can be tempting to want faster results or to increase your dose too soon, but patience is important. The gradual dosing plan is designed to protect your body and make sure you can stay on the medicine long enough to benefit from it. Most people will not see major changes right away, and that is normal. In the first month, your focus should be on learning how to give the injection, recognizing how your body responds, and following the dosing schedule without skipping.
Consistency is one of the most important parts of tirzepatide treatment. Taking the injection on the same day each week helps your body maintain steady levels of the medicine. If you miss a dose or take it at different times, the effects can become uneven, which might lead to more side effects or less predictable results. Using reminders on your phone or marking your calendar can help you stay on track. If you do miss a dose, follow your doctor’s guidance or the instructions on your prescription label about what to do next.
Monitoring is another key part of your treatment. Tirzepatide changes how your body manages sugar and insulin, so your doctor will likely ask you to check your blood sugar regularly, especially in the first few months. They may also order blood tests like HbA1c to see how well your long-term blood sugar control is improving. Tracking your weight, appetite, and how you feel day-to-day can also be helpful. Keeping a small notebook or digital log makes it easier to share information with your healthcare provider during appointments. These updates allow your doctor to decide when or if your dose should increase and how your overall progress is going.
Working with your healthcare team helps you stay safe and confident through each stage of treatment. Your doctor or nurse will guide you through dose increases and help you manage side effects. You might also work with a dietitian, diabetes educator, or pharmacist who can give you advice about meals, timing, and injection technique. Everyone’s experience is slightly different, so your team can help you make changes that fit your personal needs and health goals. Never change your dose on your own or stop taking tirzepatide without medical advice, as it can cause your symptoms to return or your blood sugar to rise suddenly.
Another important part of treatment is lifestyle support. Tirzepatide works best when it is combined with balanced eating, regular activity, and good sleep. Even small changes — like walking after meals, eating smaller portions, or drinking more water — can make a noticeable difference over time. Remember, this medication is a tool to help your body work better, not a replacement for healthy habits. Your doctor can help you set goals that are realistic and safe for your situation.
It is also important to be open and honest with your healthcare provider about how you feel. Tell them if you are having side effects, trouble injecting, or if your appetite and energy levels change too quickly. This information helps them make adjustments to your care plan and ensure your comfort. If you ever experience severe symptoms like sharp stomach pain, vomiting that doesn’t stop, or signs of dehydration, contact your healthcare provider immediately.
Over time, your body will adapt to tirzepatide, and you will learn what to expect each week. Many people find that with consistent use, careful dose increases, and medical supervision, tirzepatide becomes easier to manage. The biggest keys to success are patience, communication, and steady effort. Weight loss and blood sugar improvement usually happen gradually — often over several months — and every person’s timeline is different.
In summary, staying consistent, following the dosing plan, and keeping in touch with your healthcare team will help you get the most from tirzepatide. This medicine works best when you give it time and pair it with healthy daily habits. Keep track of your progress, be patient with yourself, and reach out to your doctor whenever you have questions. With steady use, support, and careful monitoring, tirzepatide can be an effective tool for improving long-term health and well-being.
Research Citations
Eli Lilly and Company. (2025, February 7). Zepbound (tirzepatide) injection, for subcutaneous use [Prescribing information]. U.S. Food and Drug Administration.
Eli Lilly and Company. (2022). Mounjaro (tirzepatide) injection, for subcutaneous use [Prescribing information]. U.S. Food and Drug Administration.
Frías, J. P., Davies, M. J., Rosenstock, J., Pérez Manghi, F. C., Fernández Landó, L., Bergman, B. K., et al. (2021). Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes (SURPASS-2). The New England Journal of Medicine, 385(6), 503–515.
Ludvik, B., Giorgino, F., Jódar, E., Frias, J. P., Fernández Landó, L., Brown, K., et al. (2021). Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in type 2 diabetes (SURPASS-3): A randomised, open-label, phase 3 trial. The Lancet, 398(10300), 583–598.
Del Prato, S., Kahn, S. E., Pavo, I., Weerakkody, G. J., Yang, Z., Doupis, J., et al. (2021). Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): A randomised, open-label, phase 3 trial. The Lancet, 398(10313), 1811–1824.
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., Wharton, S., Connery, L., Alves, B., et al. (2022). Tirzepatide once weekly for the treatment of obesity (SURMOUNT-1). The New England Journal of Medicine, 387(3), 205–216.
De Block, C., Bailey, C. J., Wysham, C., & D’Alessio, D. A. (2023). Tirzepatide for the treatment of adults with type 2 diabetes: An evidence review. Diabetes, Obesity and Metabolism, 25(1), 3–22.
Farzam, K., & Patel, P. (2025). Tirzepatide. In StatPearls. Treasure Island, FL: StatPearls Publishing.
Giorgino, F., Brown, K., Heise, T., et al. (2024). Effects of tirzepatide versus basal insulins in people with type 2 diabetes: Post hoc analyses of SURPASS-3 and SURPASS-4. Diabetes Care, 47(6), 1020–1029.
Inagaki, N., Takeuchi, M., Oura, T., Imaoka, T., Seino, Y., & Kadowaki, T. (2022). Tirzepatide monotherapy versus dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): A double-blind, multicentre, randomised, phase 3 trial. The Lancet Diabetes & Endocrinology, 10(9), 623–633.
Questions and Answers: Tirzepatide Starting Dose
The recommended starting dose of tirzepatide is 2.5 mg once weekly.
The 2.5 mg starting dose is intended to help the body adjust and minimize gastrointestinal side effects such as nausea, vomiting, and diarrhea.
Patients should take the 2.5 mg dose for 4 weeks before increasing to the next dose.
After 4 weeks at 2.5 mg, the dose is typically increased to 5 mg once weekly.
The 2.5 mg dose is not intended for long-term glycemic control; it’s primarily for treatment initiation and tolerance building.
No, it is recommended to wait at least 4 weeks before increasing the dose to ensure tolerance and reduce side effects.
Tirzepatide is given as a subcutaneous injection once weekly, and it can be injected in the abdomen, thigh, or upper arm.
If a dose is missed, it should be taken as soon as possible within 4 days (96 hours). If more than 4 days have passed, skip the missed dose and continue with the next scheduled dose.
Yes. Before starting, healthcare providers should evaluate renal function, history of pancreatitis, and potential contraindications such as medullary thyroid carcinoma or MEN2.
Generally, no dose adjustment is needed for age or mild-to-moderate renal impairment, but monitoring for tolerability is advised.

