Table of Contents
Introduction
Over the last few decades, the treatment of type 2 diabetes and obesity has changed in major ways. Doctors used to rely mostly on insulin or older oral medicines like metformin and sulfonylureas. While these medicines helped lower blood sugar, many people still struggled with weight gain, long-term complications, and the risk of heart problems. As researchers learned more about how the body processes food and regulates hormones, new medicines were created that work with the body’s own natural signals. One of the most exciting recent advances is a drug called tirzepatide.
Tirzepatide belongs to a group of medicines called “incretin-based therapies.” Incretins are hormones that the gut releases after eating to help control blood sugar. These hormones tell the pancreas to release insulin when sugar levels are high, reduce the liver’s release of stored sugar, and slow down how quickly food leaves the stomach. They also play a role in appetite and weight. By copying the effects of these hormones, incretin-based drugs help improve blood sugar and support weight loss in people who have type 2 diabetes or obesity.
Until recently, most of the focus was on GLP-1 receptor agonists. These drugs act like a natural hormone called glucagon-like peptide-1 (GLP-1). Medicines such as semaglutide and liraglutide showed strong results for lowering blood sugar and helping patients lose weight. However, tirzepatide is different. It does not work on just one incretin pathway but on two. Tirzepatide activates both GLP-1 receptors and GIP receptors. GIP, short for glucose-dependent insulinotropic polypeptide, is another hormone with important effects on insulin release and fat metabolism. By combining both pathways, tirzepatide gives a stronger and broader response than drugs that act only on GLP-1.
The discovery and testing of tirzepatide have created excitement not just in medical research but also in public health. Obesity and diabetes are two of the biggest health challenges worldwide. According to the World Health Organization, more than 400 million people live with diabetes, and millions more are at risk due to rising rates of obesity. These conditions often go together and raise the risk of heart disease, kidney disease, nerve damage, and early death. Because tirzepatide targets both blood sugar and body weight at the same time, it represents a new step forward in how doctors may manage these linked conditions.
The interest in tirzepatide has also grown because of early clinical trial results. In large international studies, patients who received tirzepatide lost a significant amount of weight—sometimes more than 20 percent of their starting weight. They also had large improvements in blood sugar control, with many reaching levels that are close to normal. These results are much stronger than what has been seen with many older medicines. Because of this, tirzepatide has been studied not only for type 2 diabetes but also for people with obesity who do not have diabetes. The research so far suggests benefits for both groups.
Another reason tirzepatide has attracted attention is its possible effects beyond blood sugar and weight. Studies have started to show improvements in blood pressure, cholesterol, and fat in the liver. These are important because people with type 2 diabetes and obesity often struggle with multiple risk factors that affect heart and metabolic health. If tirzepatide continues to show benefits across these areas, it may become a central medicine in long-term disease prevention.
This article will explain in detail how tirzepatide works, what the clinical studies show, and what patients and healthcare providers can expect in terms of effectiveness and outcomes. The goal is to give a clear and reliable overview of the evidence so far. We will look at how the medicine is used, who it is for, its side effects, and what research says about long-term outcomes. We will also explore how compounded tirzepatide, which is made in specialized pharmacies, compares with the approved brand version.
Understanding tirzepatide is important not only for doctors and scientists but also for patients who want to make informed choices about their care. Medicines like this are not a cure for diabetes or obesity, but they offer powerful new tools to help people manage these chronic conditions. By bringing together the latest knowledge from clinical studies, this article will show how tirzepatide could change the future of metabolic health.
What is Tirzepatide?
Tirzepatide is a new kind of medicine that has changed how doctors treat type 2 diabetes and obesity. It belongs to a group of drugs called “incretin-based therapies.” These medicines copy the effects of hormones that the body naturally makes after eating. These hormones help control blood sugar, appetite, and weight. Tirzepatide is different from older medicines because it acts on two different hormone pathways at the same time. For this reason, scientists call it a “dual incretin receptor agonist.”
A Dual-Pathway Drug
Most medicines in this class work only on one hormone called GLP-1 (glucagon-like peptide-1). GLP-1 is important because it helps the pancreas release insulin when blood sugar is high, slows down how fast the stomach empties food, and makes people feel full after eating. This is why GLP-1 drugs can lower blood sugar and also help with weight loss.
Tirzepatide is special because it does not only work on GLP-1. It also works on another hormone called GIP (glucose-dependent insulinotropic polypeptide). GIP also helps the pancreas release insulin after meals. But scientists have found that GIP may also play a role in how the body handles fat and regulates appetite. By acting on both GLP-1 and GIP receptors, tirzepatide combines the benefits of both hormones.
In simple terms, tirzepatide “turns on” two switches instead of one. This double action gives stronger effects on lowering blood sugar and reducing weight compared to drugs that only use the GLP-1 pathway.
How Tirzepatide Differs from Other GLP-1 Medicines
Many people have heard of other incretin medicines such as semaglutide or liraglutide. These drugs are GLP-1 receptor agonists, meaning they copy only the GLP-1 hormone. Tirzepatide, by adding GIP activity, may offer broader benefits.
Studies show that patients on tirzepatide often lose more weight and see bigger drops in blood sugar than with GLP-1 drugs alone. Doctors believe this is because the GIP effect works together with GLP-1 to improve metabolism in a more natural way. Instead of forcing one pathway, tirzepatide gives the body two different signals that balance each other out.
FDA Approval and Current Uses
The United States Food and Drug Administration (FDA) has approved tirzepatide under the brand names Mounjaro® (for type 2 diabetes) and Zepbound™ (for chronic weight management).
- For type 2 diabetes: Tirzepatide is used to help adults lower their blood sugar when diet and exercise are not enough. It can be prescribed alone or together with other diabetes medicines.
- For weight management: Tirzepatide is also approved for adults who are obese, or overweight with at least one related health problem such as high blood pressure, sleep apnea, or high cholesterol.
This makes tirzepatide one of the few drugs officially approved to treat both diabetes and obesity, two conditions that often go hand in hand.
Why Doctors and Patients Are Interested
Obesity and type 2 diabetes are both major public health problems. They affect millions of people worldwide and often occur together. Many older diabetes medicines lower blood sugar but do not help with weight loss. In fact, some can even cause weight gain. Tirzepatide is different because it can do both at once:
- Lower blood sugar to healthier levels.
- Help patients lose a significant amount of body weight.
Because of these combined benefits, tirzepatide has drawn attention not only from doctors but also from researchers studying heart disease, fatty liver disease, and other conditions linked to obesity. Early evidence suggests it may have positive effects beyond blood sugar control, though more studies are needed to confirm this.
Tirzepatide is a new kind of medicine that works on two natural hormone pathways, GLP-1 and GIP. By combining these effects, it helps control blood sugar and supports weight loss better than many older drugs. The FDA has approved tirzepatide for both type 2 diabetes and chronic weight management, making it a unique option for people who face both conditions. Its dual action is what sets it apart from traditional GLP-1 medicines and why it is considered a breakthrough in the treatment of metabolic disease.
How Does Tirzepatide Work in the Body?
Tirzepatide is a new type of medicine that helps people with type 2 diabetes and obesity. To understand how it works, it is helpful to know about two special hormones in the body: GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide). These hormones are called incretins, and they are released in the gut after eating. Their main job is to help control blood sugar and regulate appetite.
Tirzepatide is different from older drugs because it activates both of these hormone pathways at the same time. This is why it is often called a “dual incretin” or a “twin agonist.” By targeting both GLP-1 and GIP receptors, tirzepatide creates stronger effects on blood sugar and body weight than drugs that only act on one hormone.
The GLP-1 Pathway
GLP-1 is one of the most studied incretin hormones. Medicines like semaglutide and liraglutide already use this pathway. Tirzepatide also works here, but it adds another layer by targeting GIP.
GLP-1 helps the body in several important ways:
- Increases insulin release – After eating, GLP-1 tells the pancreas to release insulin. Insulin lowers blood sugar by moving glucose from the blood into the body’s cells.
- Decreases glucagon release – Glucagon is a hormone that raises blood sugar by signaling the liver to release stored glucose. Too much glucagon makes blood sugar rise. GLP-1 helps reduce glucagon levels, which improves blood sugar control.
- Slows stomach emptying – GLP-1 makes food leave the stomach more slowly. This helps prevent sharp spikes in blood sugar after meals. It also makes people feel full longer, which helps reduce how much they eat.
- Acts on the brain – GLP-1 affects appetite centers in the brain, lowering hunger and cravings.
The GIP Pathway
GIP is another incretin hormone. For many years, doctors thought it was less useful because it did not seem to work as well in people with type 2 diabetes. But new research showed that, when used together with GLP-1, it creates a powerful effect.
GIP works in several ways:
- Boosts insulin release – Like GLP-1, GIP also helps the pancreas release insulin after meals.
- Improves fat metabolism – GIP may help the body use and store fat differently, which could play a role in weight loss and energy balance.
- May support appetite control – Some studies suggest GIP helps the brain respond better to signals of fullness, working together with GLP-1 to reduce food intake.
The Dual Effect of Tirzepatide
Tirzepatide is the first medicine to act strongly on both GLP-1 and GIP receptors. This dual action is what makes it stand out compared to other treatments.
- Better blood sugar control: By combining both hormone signals, tirzepatide helps the body release insulin more effectively, reduce glucagon more strongly, and manage glucose after meals with greater precision.
- Stronger weight reduction: Because both GLP-1 and GIP affect appetite and digestion, patients taking tirzepatide often experience more weight loss than those on GLP-1 medicines alone.
- Metabolic improvements: Beyond blood sugar and weight, tirzepatide may improve cholesterol, lower blood pressure, and reduce liver fat. These are important benefits for people with type 2 diabetes, who often have several related health problems.
Metabolic Benefits Beyond Glucose Lowering
The effects of tirzepatide extend beyond just lowering blood sugar. Clinical studies show improvements in several other areas:
- Weight management: By acting on the brain and slowing digestion, tirzepatide leads to significant weight loss in many patients. Weight loss improves insulin sensitivity and reduces the strain on organs like the heart and liver.
- Cardiovascular health: Early data suggests tirzepatide helps improve blood pressure and cholesterol levels, lowering overall heart risk.
- Liver fat reduction: Some patients with type 2 diabetes also have fatty liver disease. Tirzepatide has been shown to reduce fat stored in the liver, which could help prevent long-term liver damage.
Why the Dual Pathway Matters
Older drugs focused only on the GLP-1 pathway. These drugs are effective but may reach a limit in how much they can lower blood sugar or reduce weight. By adding the GIP pathway, tirzepatide gives an extra push to the body’s natural processes.
Think of it like this: GLP-1 and GIP are two different “keys” that unlock the body’s ability to handle food and sugar. Using just one key works, but using both at the same time opens more doors. That is why tirzepatide is often described as a new generation of incretin therapy.
What Do Clinical Studies Show About Tirzepatide?
Tirzepatide is one of the most studied new medicines for both type 2 diabetes and obesity. Much of what we know about how well it works comes from two large groups of studies: the SURPASS trials and the SURMOUNT trials. These studies were carried out in thousands of people across many countries. They were designed to test not only how well tirzepatide lowers blood sugar but also how much weight it helps people lose, and what other health effects it may have.
The SURPASS Trials: Focus on Type 2 Diabetes
The SURPASS trial program was created to answer a basic question: How effective is tirzepatide for people with type 2 diabetes?
- Who participated?
More than 13,000 people with type 2 diabetes were enrolled across several SURPASS studies. Most participants had struggled to keep their blood sugar in control despite using other medicines such as metformin, insulin, or sulfonylureas. - What was tested?
Patients were given different doses of tirzepatide (5 mg, 10 mg, or 15 mg once weekly) and compared to other treatments like insulin degludec (a long-acting insulin) or semaglutide (a GLP-1 receptor agonist). - Key findings:
- Blood sugar control: On average, participants lowered their HbA1c (a measure of average blood sugar over three months) by 2.0% to 2.4%. This is a very strong effect, often better than standard insulin therapy.
- Weight reduction: Unlike insulin, which often causes weight gain, tirzepatide helped participants lose weight. In many studies, people lost 5 to 12 kilograms depending on the dose.
- More patients reached normal blood sugar levels: Up to 40–50% of participants achieved HbA1c levels below 5.7%, which is considered in the non-diabetic range.
- Blood sugar control: On average, participants lowered their HbA1c (a measure of average blood sugar over three months) by 2.0% to 2.4%. This is a very strong effect, often better than standard insulin therapy.
- Significance:
These findings suggest tirzepatide is not only effective for diabetes but also provides an additional benefit of weight loss. This is important because many people with diabetes also struggle with obesity, and losing weight improves both blood sugar and long-term health.
The SURMOUNT Trials: Focus on Obesity
The SURMOUNT trial program was built to test tirzepatide in people who did not have diabetes but were overweight or obese.
- Who participated?
Thousands of adults with a body mass index (BMI) of 27 or higher (overweight) or 30 or higher (obese) took part. Most had related health problems like high blood pressure, high cholesterol, or sleep apnea. - What was tested?
Participants were given tirzepatide injections once weekly in the same three doses (5 mg, 10 mg, 15 mg) and compared to a placebo group (no active medicine). - Key findings:
- Weight loss: After 72 weeks (about a year and a half), people on the highest dose of tirzepatide (15 mg) lost an average of 21% of their body weight. This is the most weight loss ever seen in a large trial of an injectable diabetes or obesity drug.
- Dose-response relationship: Lower doses (5 mg and 10 mg) also produced significant weight loss, though less than the 15 mg dose. Even at the smallest dose, patients lost far more weight than with placebo.
- Health improvements beyond weight: Participants also showed better cholesterol levels, lower blood pressure, and reduced waist size.
- Weight loss: After 72 weeks (about a year and a half), people on the highest dose of tirzepatide (15 mg) lost an average of 21% of their body weight. This is the most weight loss ever seen in a large trial of an injectable diabetes or obesity drug.
- Significance:
The SURMOUNT program showed that tirzepatide could be a major tool in obesity treatment. It helped people achieve levels of weight loss close to what is seen after some types of bariatric surgery, but without surgery.
Other Measured Outcomes
In both SURPASS and SURMOUNT studies, researchers also looked at health outcomes beyond just blood sugar and weight:
- Cardiovascular markers: Early results suggest tirzepatide improves cholesterol, triglycerides, and blood pressure. This could lower the risk of heart disease, which is very common in people with diabetes and obesity.
- Liver fat reduction: Some studies found tirzepatide reduced fat in the liver, which is linked to non-alcoholic fatty liver disease (NAFLD). This condition is common in people with obesity and diabetes.
- Quality of life: Patients reported improved energy levels, mobility, and general health scores.
Duration and Diversity of Participants
The trials lasted from 40 weeks to 2 years, which is long enough to see sustained effects. Importantly, participants came from many backgrounds, including different ages, races, and geographic regions. This helps make the results more reliable and more generalizable to real-world populations.
How Effective is Tirzepatide for Weight Loss?
Tirzepatide has attracted major attention because of its strong effects on weight loss. Many medications for diabetes can also cause a small amount of weight loss, but tirzepatide stands out because the results are much larger and consistent. In this section, we will look closely at what the clinical studies show, how much weight patients typically lose, and why the results are important for people who struggle with obesity and related health problems.
Evidence from the SURMOUNT Trials
The main clinical studies on tirzepatide and weight loss are called the SURMOUNT trials. These are large, carefully designed studies that included thousands of participants. The people who took part were mostly adults with obesity or who were overweight with at least one health condition related to their weight, such as high blood pressure, high cholesterol, or type 2 diabetes.
In the SURMOUNT-1 trial, patients without diabetes but who were overweight or obese took tirzepatide for 72 weeks (about a year and a half). The results showed dramatic weight loss compared to those who received only a placebo. Depending on the dose, participants lost an average of 15% to 21% of their starting body weight. For example, a person weighing 230 pounds at the start of the trial could expect to lose between 35 and nearly 50 pounds after using tirzepatide.
In the SURMOUNT-2 trial, the participants were adults who had both obesity and type 2 diabetes. This group often has a harder time losing weight. Even in this group, tirzepatide still showed strong results, with average weight loss ranging from about 12% to 15% of body weight, much higher than the placebo group.
These findings are important because most approved weight loss medications lead to a weight loss of only 5% to 10% of body weight. Tirzepatide’s results were nearly double or more.
Weight Loss Compared to Other Medications
Before tirzepatide, the medication semaglutide (a GLP-1 receptor agonist) was one of the most effective drugs for weight loss. Clinical trials for semaglutide showed average weight loss of around 12% to 15% of body weight in people without diabetes. Tirzepatide’s results, reaching up to 21%, suggest that the dual action of both GIP and GLP-1 receptor agonism may provide an additional benefit.
Head-to-head studies have also shown that tirzepatide leads to greater weight loss compared to semaglutide, especially at higher doses. This makes tirzepatide one of the most powerful medications currently studied for weight reduction.
Differences Across Dosing Levels
Tirzepatide comes in different doses: 5 mg, 10 mg, and 15 mg injected once weekly. Clinical studies show that the amount of weight loss increases with the dose.
- 5 mg dose: Patients lost an average of 15% of body weight.
- 10 mg dose: Patients lost around 18% of body weight.
- 15 mg dose: Patients lost about 20% to 21% of body weight.
While higher doses bring greater benefits, they can also cause more side effects, especially nausea and stomach discomfort. Doctors usually start patients on the lowest dose and slowly increase it, so the body can adjust.
Why This Level of Weight Loss Matters
Weight loss is not just about physical appearance. Even a modest reduction in weight, around 5% to 10% of body weight, can greatly improve health markers. For example, it can lower blood pressure, improve cholesterol, and reduce the risk of developing type 2 diabetes.
Tirzepatide’s level of weight loss goes well beyond that. Losing 15% to 20% of body weight has the potential to change the course of obesity-related conditions. Research shows that this amount of weight reduction can:
- Improve blood sugar control in people with type 2 diabetes.
- Lower the need for certain medications, including insulin.
- Reduce fat in the liver, which can help treat fatty liver disease.
- Decrease the risk of heart disease.
- Improve mobility, joint pain, and overall energy.
For many patients, these improvements can lead to a better quality of life and may even extend life expectancy.
Real-World Impact of Clinical Results
It is important to remember that clinical trials are done in controlled conditions. Patients are closely followed by healthcare teams, and lifestyle changes such as diet and exercise are encouraged. Even so, the results with tirzepatide are much stronger than what has been seen before with other medications.
In everyday practice, some patients may lose less weight than in the trials, while others may lose more, depending on factors like diet, activity level, and consistency with taking the medication. But the data clearly show that tirzepatide has the potential to help many people who have struggled for years to achieve and maintain significant weight loss.
Tirzepatide is one of the most effective medications for weight loss studied so far. Clinical trials such as SURMOUNT-1 and SURMOUNT-2 show average reductions of 12% to 21% of body weight, which is far greater than most other medications currently available. The results are dose-dependent, with higher doses leading to more weight loss but also more side effects.
This level of weight reduction has major health benefits, including better blood sugar control, improved heart health, and reduced risk of obesity-related diseases. Tirzepatide may represent a new standard in weight management treatment for people with obesity, both with and without diabetes.
How Effective is Tirzepatide for Blood Sugar Control?
Tirzepatide has been studied in large clinical trials to see how well it helps people with type 2 diabetes manage their blood sugar. These trials are known as the SURPASS program, and they tested thousands of patients across different groups. Researchers compared tirzepatide to other common diabetes treatments, including insulin, semaglutide, and placebo. The results showed that tirzepatide is one of the most effective medicines available today for lowering blood sugar.
This section explains the key findings in detail, looking at HbA1c reduction, how many people reached safe blood sugar targets, how long the effects last, and what this means for patients who may otherwise need insulin.
HbA1c Reduction Compared to Other Treatments
The main way doctors measure blood sugar control is through the HbA1c test. This test shows a person’s average blood sugar levels over the past two to three months. For most people with type 2 diabetes, the goal is to bring HbA1c below 7%.
In the SURPASS trials, tirzepatide consistently reduced HbA1c more than other medicines:
- Patients on tirzepatide 10 mg or 15 mg saw average HbA1c reductions of about 2.0% to 2.4% from their starting point.
- In comparison, semaglutide 1 mg reduced HbA1c by about 1.9%.
- Insulin glargine, a common long-acting insulin, reduced HbA1c by only about 1.3%.
This shows that tirzepatide lowered blood sugar more strongly than either a leading GLP-1 drug or basal insulin.
For patients starting with an HbA1c above 8% or 9%, the improvements were even greater. Some participants reached near-normal HbA1c levels, which is uncommon with most other diabetes medicines.
Proportion of Patients Reaching HbA1c Targets
Another way to look at effectiveness is the percentage of patients who actually reached healthy blood sugar targets.
- Over 80% of people treated with tirzepatide reached an HbA1c below 7%.
- Up to 50% of patients on the highest doses of tirzepatide lowered their HbA1c to below 5.7%. This level is considered the range for people without diabetes.
This is remarkable because very few medicines help so many people reach near-normal blood sugar.
By contrast:
- About 60–70% of patients using semaglutide reached HbA1c below 7%.
- Around 50% of patients using basal insulin reached the same target.
These results suggest that tirzepatide may help more patients gain strong control of their diabetes, even those who struggled with other medications.
Long-Term Glycemic Durability
Many diabetes medicines work well at first but lose effectiveness over time as the disease progresses. Researchers looked at whether tirzepatide’s blood sugar benefits lasted over one to two years.
The data showed that patients using tirzepatide maintained low HbA1c levels with little loss of effect. In fact, the benefits lasted longer compared to people taking basal insulin. This suggests that tirzepatide may help delay the need for stronger therapies, such as full insulin replacement, in many patients.
Durability is important because type 2 diabetes often gets worse over time, and patients usually need more than one medicine. Having a treatment that keeps working longer reduces complications and may help protect the pancreas.
Implications for Insulin-Requiring Patients
A major question for doctors is whether tirzepatide can reduce the need for insulin in people with advanced diabetes.
In studies where tirzepatide was compared directly with insulin:
- Patients on tirzepatide had greater reductions in HbA1c than those using insulin alone.
- Many patients who would normally need insulin injections were able to avoid starting insulin when treated with tirzepatide.
- In some trials, people already using insulin were able to lower their insulin doses while keeping their blood sugar under control.
This shows that tirzepatide is not only effective but may also change the treatment path for many patients, giving them an option that avoids high daily insulin use.
Why These Results Matter
Strong blood sugar control lowers the risk of complications from type 2 diabetes. High blood sugar damages blood vessels and nerves over time, leading to heart disease, kidney failure, vision loss, and amputations. By helping patients achieve large reductions in HbA1c, tirzepatide may play an important role in preventing these long-term problems.
Another key point is the combination of benefits. Most diabetes medicines either lower blood sugar or help with weight loss, but not both. Tirzepatide lowers HbA1c dramatically while also leading to significant weight reduction, which improves insulin sensitivity and further supports healthy blood sugar levels.

What Are the Common Side Effects of Tirzepatide?
Tirzepatide, like most medicines that affect hormones in the gut, can cause side effects. While it has shown strong results in lowering blood sugar and helping with weight loss, some people may find it difficult to take because of how it affects the digestive system. It is important to understand these possible side effects, how often they happen, and how doctors usually manage them.
Gastrointestinal Side Effects
The most common side effects of tirzepatide are related to the stomach and intestines. These include nausea, vomiting, and diarrhea. In clinical studies, a large number of people experienced these problems, especially when they first started taking the drug or when the dose was increased.
- Nausea: This is the most common issue. People may feel queasy or lose their appetite. For many, nausea improves after a few weeks as the body gets used to the medicine.
- Vomiting: Some patients may vomit, especially during the first few doses. Doctors often recommend starting tirzepatide at a low dose and slowly increasing it to reduce this risk.
- Diarrhea: Loose stools and frequent bowel movements may occur. This can sometimes lead to dehydration if it continues for many days.
Other digestive complaints include constipation, stomach pain, or a feeling of being full very quickly. These side effects usually happen because tirzepatide slows down how fast food leaves the stomach. While this effect helps control blood sugar and reduce hunger, it can also cause discomfort.
Dose-Dependent Tolerability
The chance of side effects often depends on the dose of tirzepatide. Lower doses (such as 5 mg once weekly) are less likely to cause stomach problems than higher doses (such as 15 mg). That is why treatment usually begins at a small dose and increases gradually.
Doctors call this a titration schedule. By raising the dose slowly, the body has more time to adapt, and many patients can tolerate the medicine better. Still, even at lower doses, some people may stop taking tirzepatide if the side effects feel too strong.
Rare but Serious Risks
Although most side effects are mild to moderate, there are some rare but more serious risks that patients and doctors must be aware of.
- Pancreatitis: This is inflammation of the pancreas, an organ that makes digestive enzymes and insulin. Symptoms include severe stomach pain that may spread to the back, along with nausea and vomiting. While uncommon, pancreatitis can be dangerous and requires immediate medical attention.
- Gallbladder Disease: Some patients may develop gallstones or inflammation of the gallbladder while on tirzepatide. This may be linked to the weight loss caused by the drug. Symptoms include pain in the upper right side of the belly, fever, or yellowing of the skin and eyes.
- Thyroid C-Cell Tumors (in animal studies): In long-term studies on rats, tirzepatide caused a type of thyroid tumor. It is not yet clear if this risk applies to humans, but because of this finding, tirzepatide should not be used by people with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN2).
These risks are uncommon, but they highlight the need for careful monitoring and medical guidance when using tirzepatide.
Comparison of Tolerability vs. Semaglutide
Semaglutide, another well-known drug in the same general class, is often compared to tirzepatide. Both medicines cause similar gastrointestinal side effects, especially during the first few weeks. However, some studies suggest that tirzepatide may cause slightly more nausea and vomiting at higher doses compared to semaglutide.
On the other hand, tirzepatide tends to produce greater weight loss and blood sugar improvements, which may balance the tolerability issues for many patients. Doctors often weigh the benefits against the side effects when deciding which drug may be more suitable for a patient.
Managing Side Effects
Doctors often give patients guidance on how to handle common side effects:
- Start low and go slow: Begin with the lowest dose and only increase after the body adjusts.
- Eat smaller meals: Large meals may make nausea worse. Eating smaller, more frequent meals can help.
- Avoid fatty, greasy, or spicy foods: These foods can worsen stomach upset.
- Stay hydrated: Drinking water or clear fluids helps prevent dehydration from vomiting or diarrhea.
- Report warning signs: Severe abdominal pain, yellowing skin, or trouble breathing should be reported immediately.
Most people who continue tirzepatide past the first few weeks find that side effects decrease over time. In many cases, patients can remain on the drug long term without ongoing discomfort.
Tirzepatide is generally safe, but side effects are common, especially in the digestive system. The most frequent problems are nausea, vomiting, and diarrhea, which often improve as the body adjusts. Higher doses bring greater results but also a higher chance of stomach upset. Rare but serious risks, such as pancreatitis, gallbladder disease, and possible thyroid tumors, require caution and monitoring. Compared with other medicines like semaglutide, tirzepatide’s side effect profile is similar, though sometimes more intense at high doses. With careful dosing and lifestyle adjustments, most patients can tolerate the drug and benefit from its strong effects on blood sugar and weight.
Who Can and Cannot Use Tirzepatide
Tirzepatide is a powerful medicine that helps people lower blood sugar and lose weight. Like all medicines, it is not right for everyone. Doctors decide who can use tirzepatide based on a person’s health, age, medical history, and safety factors. This section explains in detail who may benefit from tirzepatide, and who should not use it because of possible risks.
Adults Who May Benefit
- People with Type 2 Diabetes
Tirzepatide is approved by the U.S. Food and Drug Administration (FDA) for the treatment of type 2 diabetes. This means adults with this condition may be prescribed tirzepatide to help:
- Lower their blood sugar (HbA1c levels).
- Improve insulin response.
- Reduce the risk of long-term complications such as kidney disease, nerve damage, or heart disease.
It is especially useful for patients who have not reached their blood sugar goals with other diabetes medicines like metformin, sulfonylureas, or basal insulin.
- Adults with Obesity or Overweight with Health Problems
Tirzepatide has also been studied in people with obesity. Many of these patients do not have diabetes but struggle with extra weight that affects their health. Adults who are obese (body mass index, or BMI, of 30 or more) or overweight (BMI of 27 or more) with weight-related conditions may qualify. These conditions include:
- High blood pressure.
- High cholesterol.
- Sleep apnea.
- Heart disease.
- Joint pain from carrying extra weight.
By reducing weight and improving metabolic health, tirzepatide may lower risks for serious long-term illnesses.
People Who Should Not Use Tirzepatide
Even though tirzepatide can help many adults, there are groups of people who should not take it because it may be unsafe.
- People with a Personal or Family History of Certain Thyroid Cancers
Tirzepatide carries a warning for medullary thyroid carcinoma (MTC), a rare form of thyroid cancer. In animal studies, drugs like tirzepatide caused thyroid C-cell tumors. Because of this, people with a personal or family history of MTC should not use tirzepatide.
Another related condition is called Multiple Endocrine Neoplasia syndrome type 2 (MEN2). This genetic disorder increases the risk of thyroid tumors. Patients with MEN2 must also avoid tirzepatide.
- Pregnant and Breastfeeding Women
Tirzepatide is not recommended during pregnancy. Weight loss medicines and certain diabetes drugs may harm an unborn baby, especially in the second and third trimesters. Women who are planning to become pregnant should stop tirzepatide before trying to conceive.
It is also not known if tirzepatide passes into breast milk. Because of possible risks to a newborn, breastfeeding women are advised not to use tirzepatide.
- Children and Teenagers
Tirzepatide has not been studied in children. At this time, it is only approved for adults. Safety and effectiveness in people younger than 18 are unknown.
- People with Certain Medical Conditions
Some medical conditions may make tirzepatide unsafe or less effective. Doctors usually avoid prescribing it in these cases:
- Severe gastrointestinal disease: People with serious digestive problems such as gastroparesis (slow stomach emptying) may not tolerate tirzepatide well, because it slows digestion even more.
- History of pancreatitis: Tirzepatide and similar drugs may increase the risk of inflammation of the pancreas, so patients with past pancreatitis are advised not to use it.
- Advanced kidney disease: Nausea and vomiting caused by tirzepatide can worsen dehydration, which may put stress on the kidneys. People with end-stage kidney disease may need extra caution or should avoid the drug.
Special Considerations
Combination with Other Medicines
Some patients may take tirzepatide along with other diabetes medicines. Doctors need to carefully adjust doses, especially if patients are also using insulin or sulfonylureas, since the risk of low blood sugar (hypoglycemia) can increase.
Careful Monitoring
Even if a patient qualifies for tirzepatide, regular monitoring is important. Doctors may order lab tests, check blood pressure, monitor weight, and ask about side effects to ensure treatment is safe.
Individualized Decisions
Each patient’s case is unique. A doctor will weigh the benefits of improved blood sugar and weight loss against any possible risks. For example, someone with mild kidney problems might still use tirzepatide under close supervision, while someone with severe kidney failure might not.
Tirzepatide is best suited for adults with type 2 diabetes or obesity who need extra help controlling blood sugar or reducing weight. It should not be used by people with certain thyroid conditions, pregnant or breastfeeding women, children, or those with specific medical problems like severe stomach disease, pancreatitis, or advanced kidney failure. Doctors make decisions about prescribing tirzepatide based on safety, individual health history, and potential benefits.
What Do Long-Term Outcomes Show?
When new medicines are studied, doctors want to know not only how they work in the short term, but also what happens when people use them for months or years. Tirzepatide has shown strong early results for weight loss and blood sugar control, but the bigger question is whether these results last, and whether they lead to improvements in long-term health. Below, we look at what research has found so far about tirzepatide’s effects over time.
Cardiovascular Safety Studies (Ongoing and Preliminary Data)
One of the most important goals in diabetes and obesity treatment is lowering the risk of heart disease and stroke. People with type 2 diabetes and obesity are at a higher risk of cardiovascular problems. That is why every new diabetes drug is tested in large studies to confirm that it does not raise the risk of serious heart events, and ideally, that it reduces them.
For tirzepatide, a large ongoing trial called SURPASS-CVOT (Cardiovascular Outcomes Trial) is studying whether the medication reduces the chances of heart attack, stroke, or cardiovascular death compared to insulin. While full results are still being collected, early analyses suggest tirzepatide is at least safe for the heart. In fact, many researchers believe it may provide protective benefits similar to GLP-1 medications, which have already been shown to reduce heart risk.
Preliminary findings have shown improvements in blood pressure, cholesterol levels, and body fat distribution. These changes are linked to lower cardiovascular risk, which makes experts optimistic that the final results will confirm benefits beyond blood sugar control.
Long-Term Metabolic Improvements
Tirzepatide’s effects go beyond lowering blood sugar and weight. Research has shown that people taking tirzepatide also experience improvements in other markers of metabolic health:
- Lipids (cholesterol and triglycerides): Tirzepatide has been shown to lower triglyceride levels and improve cholesterol balance, particularly by raising HDL (“good cholesterol”) and lowering LDL (“bad cholesterol”). This shift supports better heart health over time.
- Blood pressure: Weight loss from tirzepatide is often accompanied by a drop in both systolic and diastolic blood pressure. Even small improvements in blood pressure can significantly reduce the risk of stroke and heart disease.
- Liver fat: Non-alcoholic fatty liver disease (NAFLD) is common in people with obesity and type 2 diabetes. Studies using imaging scans have shown that tirzepatide can reduce fat buildup in the liver. This may help prevent progression to more serious liver problems like cirrhosis.
By improving several aspects of metabolic health at the same time, tirzepatide may help protect against complications linked to diabetes and obesity.
Impact on Quality of Life and Adherence Trends
Another important question is whether patients can continue using tirzepatide for long periods. In clinical trials, many participants stayed on the medication for more than a year, and most reported improvements in quality of life.
People who lose weight with tirzepatide often report:
- More energy for daily activities
- Better mobility and less joint pain
- Improvements in sleep quality
- Higher self-confidence
Adherence, or sticking with the medication, is also a key factor. Because tirzepatide is given only once a week by injection, many patients find it more convenient than daily medicines or insulin regimens. However, side effects like nausea can still make some people stop treatment. Research shows that slow dose increases and supportive care can improve tolerability and help patients continue therapy long-term.
Durability of Weight Loss After Discontinuation
One of the biggest questions is what happens when patients stop taking tirzepatide. Current data show that most people regain some weight after discontinuation. This is not unique to tirzepatide — it is common with all weight loss medications because the underlying biology of appetite and metabolism tends to return to its previous state once treatment ends.
In clinical studies, people who stopped tirzepatide gained back part of the weight they had lost, often within months. However, some patients were able to maintain lower body weight compared to their starting point, especially if they continued lifestyle measures such as diet and exercise.
This means tirzepatide may need to be viewed as a long-term or even lifelong treatment for many individuals, similar to how blood pressure or cholesterol medicines are used. Doctors will need to discuss with patients what realistic expectations are, and whether ongoing therapy is appropriate.
The current evidence shows that tirzepatide provides more than just short-term improvements. It helps lower blood sugar, reduces weight, and improves many other metabolic health markers. Early signs suggest it may also protect the heart, though more data are needed from ongoing cardiovascular trials. Quality of life tends to improve for many patients, and weekly dosing supports adherence. However, weight regain after stopping therapy highlights the need for careful planning and long-term strategies.

How is Tirzepatide Administered?
Tirzepatide is not taken by mouth like many traditional diabetes medicines. Instead, it is given as an injection under the skin. This is called a subcutaneous injection. Many patients give these injections to themselves at home, after learning the correct technique from a doctor, nurse, or pharmacist. Understanding how tirzepatide is given is important because it affects both safety and effectiveness.
Subcutaneous Injection Method and Frequency
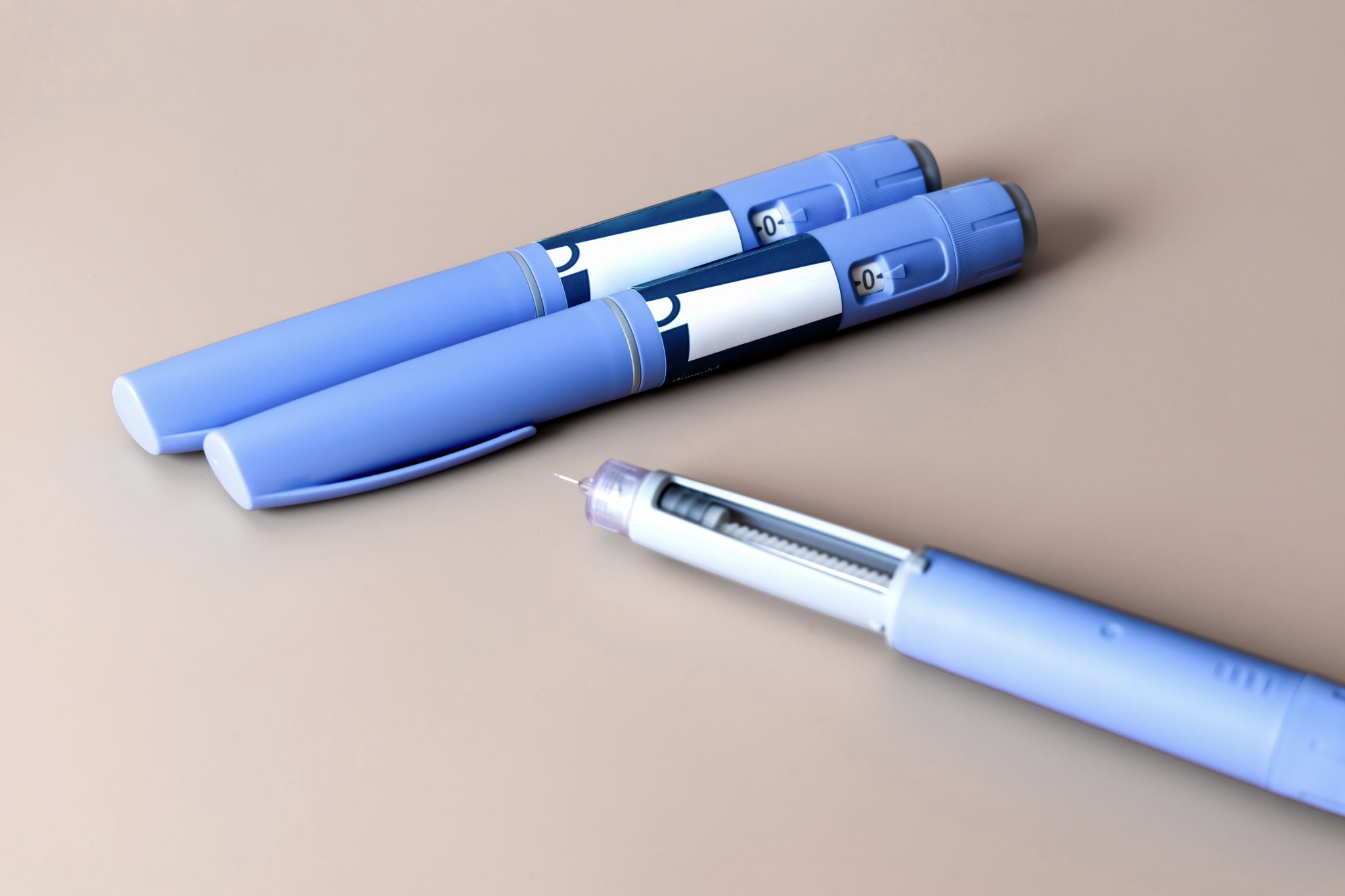
Tirzepatide is injected just under the skin using a prefilled pen device. This is similar to other modern injectable medicines for diabetes and weight management.
- Injection sites: The most common areas are the stomach (abdomen), the front of the thighs, or the back of the upper arms. These sites have enough fatty tissue to absorb the medicine slowly and evenly.
- Rotation: Patients are taught to rotate injection sites with each dose. This means not always injecting in the exact same spot, because repeated injections in one area can cause skin irritation or thickening.
- Frequency: Tirzepatide is taken once a week. This weekly schedule is one of the reasons many patients prefer it compared to older medications that require daily injections.
The prefilled pen is designed to be simple. Patients usually do not need to measure the medicine or handle a needle directly. Instead, they click and press the device against the skin until it delivers the full dose.
Titration Schedule for Tolerability
When starting tirzepatide, patients do not immediately begin at the highest dose. Instead, doctors use a titration schedule. Titration means gradually increasing the dose over time.
- The first dose is usually 2.5 mg once weekly, which allows the body to adjust.
- After four weeks, the dose is increased to 5 mg once weekly.
- Depending on how the patient tolerates the medicine and how well it controls blood sugar or supports weight loss, the dose may then be raised to 10 mg or even 15 mg.
This step-by-step increase is important because tirzepatide can cause side effects, especially nausea, vomiting, or diarrhea, when the dose is raised too quickly. By moving up slowly, patients are more likely to continue treatment comfortably.
Doctors decide the best dose based on the patient’s needs. For example:
- A person with type 2 diabetes who mainly needs blood sugar control might do well on 5 or 10 mg.
- A person focused on weight loss may need a higher dose, like 15 mg, to get the strongest effect.
Storage, Handling, and Self-Injection Education
Tirzepatide pens need to be handled carefully so that the medicine stays effective.
- Storage: The pens are stored in the refrigerator until use. However, once taken out, most pens can stay at room temperature for a limited time (usually up to 21 days, depending on manufacturer instructions). Patients must always check the guidance that comes with their prescription.
- Light and heat: Pens should not be exposed to direct sunlight or extreme heat, since this can damage the medication.
- Needle safety: Each pen is single-use. After injection, it should be safely discarded in a sharps container.
Doctors and nurses usually provide training sessions to help patients feel comfortable giving injections. In these sessions, patients learn:
- How to prepare the pen
- How to select and clean the injection site
- How to inject slowly and correctly
- What to do if the dose is missed
With practice, most patients find self-injection simple and fast.
Difference Between Compounded Tirzepatide and FDA-Approved Formulations
Not all tirzepatide available on the market is the same. There are two main types:
- FDA-approved versions: These include the branded medication (for example, Mounjaro). These pens are made under strict quality controls, ensuring each dose is consistent and safe. They come in specific strengths and are supplied with full instructions.
- Compounded tirzepatide: Some compounding pharmacies prepare tirzepatide in different forms, such as multi-dose vials. While these can be less expensive or more accessible in areas with shortages, compounded versions do not always go through the same strict FDA testing process. This may raise concerns about consistency, sterility, and safety.
The method of administration can differ slightly:
- FDA-approved pens are single-use and designed for ease of use.
- Compounded vials often require drawing up the medicine into a syringe, which can be harder for patients without training.
Because of these differences, patients should only use compounded tirzepatide under close medical supervision and should discuss potential risks with their healthcare provider.
Missed Doses and Practical Considerations
Sometimes, a patient might forget a dose. The guidance is:
- If less than 4 days have passed since the missed dose, the patient can take it as soon as remembered.
- If more than 4 days have passed, they should skip that dose and take the next dose at the regular weekly time.
This flexibility is helpful since the medication is designed to last for a full week in the body.
Other practical considerations include:
- Taking the dose on the same day each week helps patients remember.
- Setting reminders on phones or calendars can reduce the chance of missed doses.
- Some patients prefer taking the injection in the morning, while others choose evenings — both are acceptable, as long as it is consistent.
Tirzepatide is given once a week by subcutaneous injection. It is started at a low dose and gradually increased to help reduce side effects. The pens are easy to use, but patients must learn the proper injection technique and how to store and handle the medicine. While FDA-approved versions come in ready-to-use pens, compounded tirzepatide may require syringes and carry extra risks. Following proper guidance on injection sites, rotation, and what to do when a dose is missed helps patients get the most benefit from treatment.
How Does Compounded Tirzepatide Differ from Branded Versions?
Tirzepatide is now widely used for type 2 diabetes and obesity management. The version that most people hear about is the branded, FDA-approved form sold under the name Mounjaro® (for diabetes) and Zepbound™ (for obesity). These versions are produced by the pharmaceutical company Eli Lilly. However, in recent years, some patients have also received compounded tirzepatide from certain pharmacies. While both contain the same active drug, there are very important differences between branded tirzepatide and compounded versions. Understanding these differences is key for both safety and effectiveness.
Regulatory Differences: FDA-Approved vs Compounded
The branded versions of tirzepatide, such as Mounjaro and Zepbound, go through a strict approval process by the U.S. Food and Drug Administration (FDA). This means that the drug has been tested in large clinical trials with thousands of people. The FDA reviews all data on safety, effectiveness, side effects, and manufacturing quality before approving the medication. Once approved, every batch must meet the same high standards of purity, strength, and stability.
By contrast, compounded tirzepatide is not FDA-approved. Compounding pharmacies prepare medications in smaller batches, often mixing or altering ingredients for individual patients. In some cases, compounding is important, for example when patients need a different dose or cannot take a medication in its standard form. However, compounded tirzepatide does not go through the same level of testing or quality control as branded tirzepatide. This means there can be more variability between batches and less assurance that every dose works exactly the same way.
Safety and Quality Considerations
One of the main differences between branded and compounded tirzepatide is quality assurance. With FDA-approved tirzepatide, patients know that the medication is manufactured under Good Manufacturing Practices (GMP). These are strict rules designed to prevent contamination, ensure proper dosage, and confirm that the drug is stable during shipping and storage.
Compounded tirzepatide may not always follow the same strict standards. The quality of compounded medications depends heavily on the specific pharmacy that prepares them. Some compounding pharmacies may maintain very high standards, but others may not. As a result, there is a greater risk of:
- Inaccurate dosing – patients may receive more or less tirzepatide than expected.
- Contamination – if sterile procedures are not followed, bacteria or other harmful substances could enter the medication.
- Instability – compounded versions may not last as long or may degrade faster.
The FDA has issued warnings about compounded versions of tirzepatide because of these concerns. Patients need to understand that compounded medications are not reviewed for safety and effectiveness before use.
Clinical Effectiveness and Variability
Another key difference is in how reliable the results are. With branded tirzepatide, doctors can expect a certain level of blood sugar reduction or weight loss based on the published clinical studies. For example, patients on FDA-approved tirzepatide have been shown to lower HbA1c by up to 2% and lose up to 20% of body weight, depending on the dose and duration of treatment.
Compounded tirzepatide may not always give the same results. This is because the formulation could vary in purity, absorption, or strength. If the dose is slightly weaker or stronger than intended, the patient’s response may be very different. This makes it harder for doctors to predict how effective the treatment will be. In some cases, patients may not achieve the same level of blood sugar control or weight loss as with the branded product.
Patient Access and Affordability Issues
Why do some patients turn to compounded tirzepatide? A main reason is access and cost. FDA-approved tirzepatide can be very expensive without insurance, often costing more than $1,000 per month. Even with insurance, coverage may be limited depending on the patient’s diagnosis and the insurance company’s rules.
Because of high demand and supply shortages, some patients have struggled to obtain branded tirzepatide from pharmacies. Compounding pharmacies have sometimes stepped in to fill this gap, offering versions that may cost less and be easier to access. While this can improve availability, it also raises the safety and quality issues mentioned earlier.
It is important to note that not all compounded tirzepatide is legal. The FDA allows compounding only when there is a true shortage of the FDA-approved drug or when a patient requires a unique formulation that cannot be met by the standard product. Using compounded tirzepatide outside of these conditions can put patients at risk.
Branded tirzepatide is FDA-approved, studied in large trials, and manufactured under strict quality controls. This provides strong evidence that it is both safe and effective. Compounded tirzepatide, on the other hand, is not FDA-approved, and its safety and effectiveness may vary.
Patients should always discuss these differences with their healthcare provider. While compounded versions may sometimes seem more affordable or easier to obtain, the potential risks must be weighed carefully. For long-term use, the branded, FDA-approved product remains the gold standard for safety, consistency, and predictable results.
Conclusion
Tirzepatide is a new medicine that has quickly become one of the most important advances in the treatment of type 2 diabetes and obesity. Over the past several years, it has drawn worldwide attention not only because of its ability to lower blood sugar, but also because of the impressive weight loss seen in patients during clinical studies. It works in a unique way by targeting two different hormone systems in the body, GLP-1 and GIP, which together improve how the body controls blood sugar, appetite, and energy balance. This dual action makes tirzepatide different from older medicines that only act on one pathway.
The strength of tirzepatide is not only in its design but also in the large amount of clinical evidence that supports its use. The SURPASS trials, which focused on type 2 diabetes, showed that tirzepatide helped patients reach lower HbA1c levels than many of the current standard medicines, including insulin and other GLP-1 receptor agonists. Some patients even achieved blood sugar levels in the range that is considered normal, which has not been common with most diabetes treatments. In the SURMOUNT studies, which looked at people with obesity, tirzepatide led to an average weight loss of more than 20% of body weight in many participants. This is a result that approaches what can be seen with bariatric surgery, but through medication alone. Such findings show how powerful this therapy can be when used properly.
Tirzepatide is also changing the way doctors and patients think about long-term health. Managing type 2 diabetes and obesity is not only about lowering numbers on a chart. It is about reducing the risk of heart disease, improving liver health, protecting kidney function, and increasing quality of life. Early data suggest that tirzepatide can help improve cholesterol, blood pressure, and markers of liver fat. Ongoing cardiovascular outcome trials will show whether these changes translate into fewer heart attacks, strokes, and deaths. If confirmed, tirzepatide may become not just a treatment for diabetes and obesity, but a medicine that reduces the burden of major chronic diseases.
Another reason tirzepatide is important is because of its role in giving patients more options. For many years, insulin was the main treatment when oral medicines could no longer control blood sugar. While effective, insulin is often linked with weight gain and can cause low blood sugar episodes. GLP-1 drugs improved this picture by supporting weight loss and lowering risk of hypoglycemia, but they did not always provide enough blood sugar control for everyone. Tirzepatide brings together stronger blood sugar lowering with greater weight loss, which addresses both sides of the problem in type 2 diabetes and obesity.
However, like all medicines, tirzepatide also has limits and risks. Gastrointestinal side effects such as nausea, diarrhea, and vomiting are common, especially when starting the drug or increasing the dose. Careful dose titration helps many patients adjust, but not all people tolerate it well. There are also warnings based on animal studies about the risk of thyroid C-cell tumors, and it should not be used in people with certain rare genetic conditions like multiple endocrine neoplasia type 2. Doctors and patients must weigh these risks against the benefits.
Compounded tirzepatide has also become a topic of discussion. Some patients turn to compounding pharmacies because of cost or limited access to brand-name medications. But compounded products may not always have the same quality or reliability as FDA-approved versions. This raises safety concerns, and patients are encouraged to speak with their healthcare providers before considering compounded formulations. The future of tirzepatide depends not only on its clinical results but also on how regulators, manufacturers, and healthcare systems make it available and safe for the people who need it.
The future outlook for dual incretin therapies like tirzepatide is very promising. Researchers are already studying whether similar medicines may help other conditions such as fatty liver disease, heart failure, or even Alzheimer’s disease, since metabolic health affects so many systems in the body. As more data comes in, doctors will have a clearer picture of how broad the benefits may be.
In summary, tirzepatide represents a major step forward in modern medicine for diabetes and obesity. Its ability to combine strong blood sugar control with significant and lasting weight loss makes it different from most other drugs available today. The evidence from clinical trials shows both its power and its safety profile, though ongoing studies will continue to provide important answers about long-term risks and benefits. For patients and clinicians, tirzepatide offers hope for better outcomes and a tool that can reshape the way we think about managing two of the most common and challenging health problems of our time.
Research Citations
Rosenstock, J., Wysham, C., Frías, J. P., Kaneko, S., Lee, C. J., Fernández Landó, L., Mao, H., Cui, X., Karanikas, C. A., & Thieu, V. T. (2021). Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): A double-blind, randomised, phase 3 trial. The Lancet, 398(10295), 143–155.
Ludvik, B., Giorgino, F., Jódar, E., Frías, J. P., Fernández Landó, L., Brown, K., Bray, R., & Rodríguez, Á. (2021). Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in type 2 diabetes (SURPASS-3): A randomised, open-label, phase 3 trial. The Lancet, 398(10300), 583–598.
Del Prato, S., Kahn, S. E., Pavo, I., Weerakkody, G. J., Yang, Z., Doupis, J., Aizenberg, D., Wynne, A. G., Riesmeyer, J. S., Heine, R. J., & Wiese, R. J. (2021). Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): A randomised, open-label, multicentre, phase 3 trial. The Lancet, 398(10313), 1811–1824.
Frías, J. P., Davies, M. J., Rosenstock, J., Pérez Manghi, F. C., Fernández Landó, L., Bergman, B. K., Liu, B., Cui, X., & Brown, K.; SURPASS-2 Investigators. (2021). Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. The New England Journal of Medicine, 385(6), 503–515.
Jastreboff, A. M., Aronne, L. J., Ahmad, N. N., Wharton, S., Connery, L., Alves, B., Kiyosue, A., Zhang, S., Liu, B., Bunck, M. C., Stefanski, A., & SURMOUNT-1 Investigators. (2022). Tirzepatide once weekly for the treatment of obesity. The New England Journal of Medicine, 387(3), 205–216.
Gastaldelli, A., Cusi, K., Fernández Landó, L., Bray, R., Brouwers, B., & Rodríguez, Á. (2022). Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): A substudy of the randomised, open-label, phase 3 SURPASS-3 trial. The Lancet Diabetes & Endocrinology, 10(6), 393–406.
Heerspink, H. J. L., Sattar, N., Pavo, I., Haupt, A., Duffin, K. L., Yang, Z., Wiese, R. J., Tuttle, K. R., & Cherney, D. Z. I. (2022). Effects of tirzepatide versus insulin glargine on kidney outcomes in type 2 diabetes in the SURPASS-4 trial: Post-hoc analysis of a randomised, phase 3 trial. The Lancet Diabetes & Endocrinology, 10(11), 774–785.
Inagaki, N., Takeuchi, M., Oura, T., Imaoka, T., & Seino, Y. (2022). Efficacy and safety of tirzepatide monotherapy compared with dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): A double-blind, multicentre, randomised, phase 3 trial. The Lancet Diabetes & Endocrinology, 10(9), 623–633.
Aronne, L. J., Jastreboff, A. M., et al. (2025). Tirzepatide as compared with semaglutide for the treatment of obesity (SURMOUNT-5). The New England Journal of Medicine, 392, ePub ahead of print.
Battelino, T., Bergenstal, R. M., Giorgino, F., et al. (2022). Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): A substudy of a randomised, open-label, phase 3 trial. The Lancet Diabetes & Endocrinology, 10(6), 407–417.
Questions and Answers: Tirzepatide Compound
Tirzepatide is a novel injectable medication that acts as a dual agonist of the glucose-dependent insulinotropic polypeptide (GIP) receptor and the glucagon-like peptide-1 (GLP-1) receptor. It is primarily used for the treatment of type 2 diabetes and obesity.
Tirzepatide mimics the effects of two incretin hormones, GIP and GLP-1. These hormones enhance insulin secretion, suppress glucagon release, slow gastric emptying, and reduce appetite, leading to improved blood sugar control and weight loss.
Tirzepatide is FDA-approved for type 2 diabetes management. It is also under review and increasingly prescribed for chronic weight management in adults with obesity or overweight and at least one weight-related condition.
Tirzepatide is given as a once-weekly subcutaneous injection. Patients usually self-administer the dose into the thigh, abdomen, or upper arm.
The most common side effects include nausea, vomiting, diarrhea, decreased appetite, and constipation. These gastrointestinal effects are usually mild to moderate and tend to lessen over time.
In clinical trials, tirzepatide demonstrated significant weight loss effects, with many patients losing 15–20% of their body weight, making it one of the most effective medications currently available for obesity management.
Tirzepatide itself rarely causes hypoglycemia. However, when combined with insulin or sulfonylureas, the risk increases, and careful monitoring is recommended.
Tirzepatide is not recommended for people with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN2). It should also be avoided in those with severe hypersensitivity to the drug.
While both target GLP-1 receptors, tirzepatide also activates GIP receptors, potentially providing enhanced effects on glucose control and weight reduction compared to GLP-1 agonists alone.
Tirzepatide is marketed under the brand name Mounjaro for type 2 diabetes and is also being commercialized as Zepbound for obesity treatment.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.
