Table of Contents
Introduction
Tirzepatide is a medicine that has changed the way doctors manage type 2 diabetes and obesity. It works by helping the body control blood sugar levels and support healthy weight loss. Many people have heard of tirzepatide by its brand names, such as Mounjaro® (used for type 2 diabetes) and Zepbound® (approved for weight management). These medications are given through a small, pre-filled injection pen that patients use once a week. While the medicine itself is highly effective, learning how to use the pen correctly is just as important. Proper technique helps you get the full benefit of the medication, avoid side effects, and prevent mistakes that could make the medicine less effective.
Tirzepatide belongs to a newer class of medications called GIP and GLP-1 receptor agonists. These are hormones that naturally exist in the body and help regulate how we process food and store energy. Tirzepatide acts on both of these hormone receptors. By doing so, it helps your pancreas release the right amount of insulin after meals, slows down how fast food leaves your stomach, and helps control your appetite. This combination supports lower blood sugar levels and promotes weight loss over time. Because tirzepatide acts in multiple ways, it offers a strong and balanced approach to managing type 2 diabetes and obesity.
The approval of tirzepatide by the U.S. Food and Drug Administration (FDA) was based on several major clinical trials that showed significant improvements in both blood sugar and body weight. People taking tirzepatide often lost more weight than those taking other diabetes medications, while also achieving better control of their glucose levels. For individuals living with type 2 diabetes, this dual effect is important because it reduces long-term risks such as heart disease, nerve damage, and kidney problems. For those using it for weight loss, it can help improve other related health issues like high blood pressure and cholesterol.
Because tirzepatide is given by injection, it is important for patients to feel confident about how to use the pen correctly. The pen is designed for simplicity, but using it properly still requires care and attention. You will need to know how to store it, how to prepare it, and exactly how to inject it into the right area of your body. Many people are nervous about giving themselves an injection, especially at first, but with proper instruction, it becomes a quick and easy weekly routine. This article will guide you step by step through how to use the tirzepatide pen safely and effectively.
Understanding how tirzepatide fits into your overall treatment plan is also essential. If you are taking it for type 2 diabetes, it will usually be part of a broader plan that includes diet, exercise, and sometimes other medications. If you are taking it for weight loss, it will be most effective when combined with a healthy eating plan and regular physical activity. Tirzepatide is not a quick fix, but rather a tool to help your body achieve better balance and long-term results.
Safety is another major part of using tirzepatide correctly. Like all medicines, tirzepatide can have side effects, and your healthcare provider will work with you to reduce your risks. Learning to use the pen properly helps avoid problems such as injecting into the wrong area, using a pen past its expiration date, or not storing it at the right temperature. It’s also important to understand how to handle missed doses, how to dispose of used pens safely, and when to call your healthcare provider if something doesn’t seem right.
This article was written to make the process of using the tirzepatide pen simple and clear for everyone. Whether you are new to injectable medication or switching from another diabetes drug, you will find straightforward instructions and explanations. Every section of this guide is based on up-to-date medical information and written in plain language so you can easily follow along. You will learn what tirzepatide is, who can use it, how it works, and exactly how to use the pen step by step. You will also find guidance on dosing schedules, side effects, and storage to help you use this medicine safely at home.
By the end of this article, you should feel more confident about using the tirzepatide pen on your own. You will understand how it supports your blood sugar control and weight goals, and why following each step carefully is so important. Learning to use your pen properly is a key part of taking charge of your health. This guide will help you develop the knowledge and confidence to do that safely and effectively. Tirzepatide has the potential to improve the lives of millions of people living with diabetes and obesity. With the right information and careful use, it can help you reach your treatment goals and improve your overall well-being.
What Is Tirzepatide and How Does It Work?
Tirzepatide is a medicine designed to help people manage type 2 diabetes and support weight loss. It belongs to a new group of medicines that act on two natural hormones in the body: GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1). These hormones play an important role in controlling blood sugar and appetite. Tirzepatide works by copying the effects of both, helping your body control glucose levels more effectively and making you feel full sooner after eating.
How Tirzepatide Works in the Body
When you eat, your stomach and intestines release hormones that help control how your body uses food for energy. Two of these hormones—GIP and GLP-1—help lower blood sugar by encouraging your pancreas to release insulin, the hormone that moves sugar from your blood into your cells. They also slow the release of another hormone called glucagon, which raises blood sugar levels.
People with type 2 diabetes often have a reduced ability to use insulin or may not make enough of it. This causes blood sugar levels to stay high. Tirzepatide helps correct this by working in two main ways:
- Improves insulin release: When blood sugar levels rise after eating, tirzepatide helps the pancreas release more insulin.
- Reduces glucagon levels: It tells the liver to release less glucose into the blood.
These effects help lower blood sugar without causing dangerous drops (hypoglycemia) when used alone.
Tirzepatide also slows stomach emptying, meaning food stays in the stomach longer. This helps reduce appetite and leads to smaller meals and gradual weight loss over time. Many people notice they feel full sooner and have fewer cravings, which can make it easier to stick to a healthy eating plan.
Dual Hormone Action: GIP and GLP-1
Older diabetes medications, such as semaglutide or liraglutide, act only on the GLP-1 receptor. Tirzepatide is different because it activates both GLP-1 and GIP receptors. This dual action helps improve how the body manages both sugar and fat.
- GLP-1 effects: Stimulates insulin, lowers glucagon, slows digestion, and reduces appetite.
- GIP effects: Improves insulin sensitivity and may increase the body’s ability to use stored fat for energy.
When these two effects are combined, the result is stronger control of blood sugar and more significant weight loss compared to using GLP-1 alone.
Clinical studies show that tirzepatide can help people lower their average blood sugar (HbA1c) by as much as 2% or more and support substantial weight loss, often greater than with older medicines.
Benefits for People with Type 2 Diabetes
For individuals living with type 2 diabetes, controlling blood sugar helps prevent long-term complications such as heart disease, nerve damage, kidney failure, and vision problems. Tirzepatide can help:
- Lower fasting and post-meal blood sugar levels
- Improve overall blood sugar control (measured by HbA1c)
- Support weight reduction, which further helps blood sugar management
- Reduce the need for other diabetes medications in some patients
In addition, clinical trials suggest tirzepatide may improve cholesterol levels and blood pressure, both of which are important for heart health.
Benefits for Weight Management
Even for people without diabetes, tirzepatide can help manage obesity when used with a healthy diet and regular physical activity. By reducing appetite, improving fullness, and changing how the body uses stored energy, tirzepatide can support a gradual and steady decrease in body weight.
Studies show that participants lost on average 15% to 22% of their body weight over 72 weeks, depending on the dose used. This level of weight reduction can lead to major health improvements, such as lower risk of diabetes, improved blood pressure, and better cholesterol control.
Differences Between Tirzepatide and Other Medications
While tirzepatide shares some similarities with other injectable drugs used for diabetes or weight loss, such as semaglutide (Ozempic®, Wegovy®) or liraglutide (Victoza®, Saxenda®), it stands out because of its dual-action mechanism.
Here’s how it differs:
- Broader hormone activity: It activates both GIP and GLP-1 receptors, whereas others act only on GLP-1.
- Greater effect on weight loss: Clinical trials show that tirzepatide can lead to more significant weight reduction compared to single-action GLP-1 drugs.
- Stronger blood sugar control: It may lower HbA1c further than other medications in the same class.
- Similar safety profile: The most common side effects—such as nausea and stomach upset—are similar to those seen with other GLP-1 drugs.
Tirzepatide is a dual-action injectable medication that mimics two natural hormones to help control blood sugar and support weight loss. It works by increasing insulin release, decreasing glucagon, slowing digestion, and reducing appetite. For people with type 2 diabetes, it improves both blood sugar control and body weight. For people with obesity, it helps achieve meaningful and sustained weight loss.
Because of its unique ability to act on both GIP and GLP-1 receptors, tirzepatide represents an important advancement in the treatment of diabetes and obesity. Understanding how it works helps patients use it correctly and recognize the benefits that come from following their treatment plan.
Who Can Use Tirzepatide?
Tirzepatide is a prescription medicine used to help people manage type 2 diabetes and chronic weight problems. It is not a general weight-loss drug for everyone, and it should only be used under the care of a healthcare provider. Understanding who can safely use tirzepatide is very important before starting treatment.
Approved Uses
Tirzepatide is approved by the U.S. Food and Drug Administration (FDA) for two main purposes:
- Type 2 Diabetes:
Tirzepatide helps adults with type 2 diabetes control blood sugar levels. It works by helping the body release insulin when needed and lowering the amount of sugar made by the liver. It also slows how fast food leaves the stomach, which can help prevent blood sugar spikes after meals. - Chronic Weight Management:
Tirzepatide is also approved to help adults with obesity or who are overweight and have at least one weight-related condition, such as high blood pressure, high cholesterol, or type 2 diabetes. It helps by reducing appetite, increasing feelings of fullness, and improving how the body uses insulin.
These approvals are based on large clinical studies that showed tirzepatide can lower blood sugar levels and lead to significant weight loss when combined with healthy eating and physical activity.
Who Is Eligible
Not everyone is a good candidate for tirzepatide. Your healthcare provider will review your health history, current medications, and medical conditions to decide if it is safe and appropriate for you.
You may be a candidate for tirzepatide if you:
- Have type 2 diabetes and have not been able to reach your blood sugar goals with diet, exercise, or other medicines.
- Have a body mass index (BMI) of 30 or higher, which means you are in the obesity range.
- Have a BMI of 27 or higher with at least one related condition, such as high blood pressure, high cholesterol, or sleep apnea.
Your provider may also consider factors such as your heart health, kidney function, and history of other metabolic disorders before prescribing tirzepatide.
Who Should Not Use Tirzepatide
Tirzepatide is not safe for everyone. There are certain medical conditions and risk factors that make its use unsafe or not recommended.
Do not use tirzepatide if you:
- Have a personal or family history of medullary thyroid carcinoma (MTC), a rare type of thyroid cancer.
- Have Multiple Endocrine Neoplasia syndrome type 2 (MEN 2), which increases the risk of thyroid tumors.
- Have had a serious allergic reaction to tirzepatide or any of its ingredients.
- Are younger than 18 years old, because it has not been studied for safety in children.
Use caution or discuss with your doctor if you:
- Have pancreatitis (inflammation of the pancreas) now or in the past. Tirzepatide can increase the risk of this condition.
- Have severe stomach or intestinal problems, such as gastroparesis (slow stomach emptying).
- Have kidney or liver disease, since dosage adjustments or closer monitoring may be needed.
- Are pregnant or planning to become pregnant, because tirzepatide is not recommended during pregnancy.
- Are breastfeeding, since it is not known if the drug passes into breast milk.
Your doctor will weigh the benefits and risks before deciding if tirzepatide is suitable for you.
Doctor’s Assessment Before Starting
Before prescribing tirzepatide, your healthcare provider will perform a full medical review. This may include:
- Measuring your blood sugar (A1C) and fasting glucose levels.
- Checking your weight and BMI.
- Reviewing any other medications you take, especially those for diabetes, high blood pressure, or cholesterol.
- Asking about your personal and family medical history, particularly related to thyroid disease or cancer.
- Assessing your heart, kidney, and liver health.
This information helps your provider decide on the right starting dose and make sure tirzepatide will not interact with your current treatments.
Prescription and Monitoring
Tirzepatide is only available with a doctor’s prescription. It should never be shared or used without medical advice. During treatment, regular follow-up visits are important. Your provider will monitor your:
- Blood sugar levels.
- Weight changes.
- Side effects or signs of intolerance.
- Blood pressure and cholesterol.
If needed, your dose may be adjusted gradually. This careful monitoring helps make sure you get the most benefit from tirzepatide while avoiding serious side effects.
Tirzepatide is designed for adults with type 2 diabetes or those struggling with obesity-related conditions, not for short-term or cosmetic weight loss. The decision to start this medication should always be made with your healthcare provider, based on your medical history and health goals.
Using tirzepatide safely means being honest about your health conditions, following medical instructions carefully, and keeping up with regular checkups. With proper supervision, tirzepatide can be a powerful tool to improve blood sugar control, support healthy weight loss, and reduce long-term health risks.

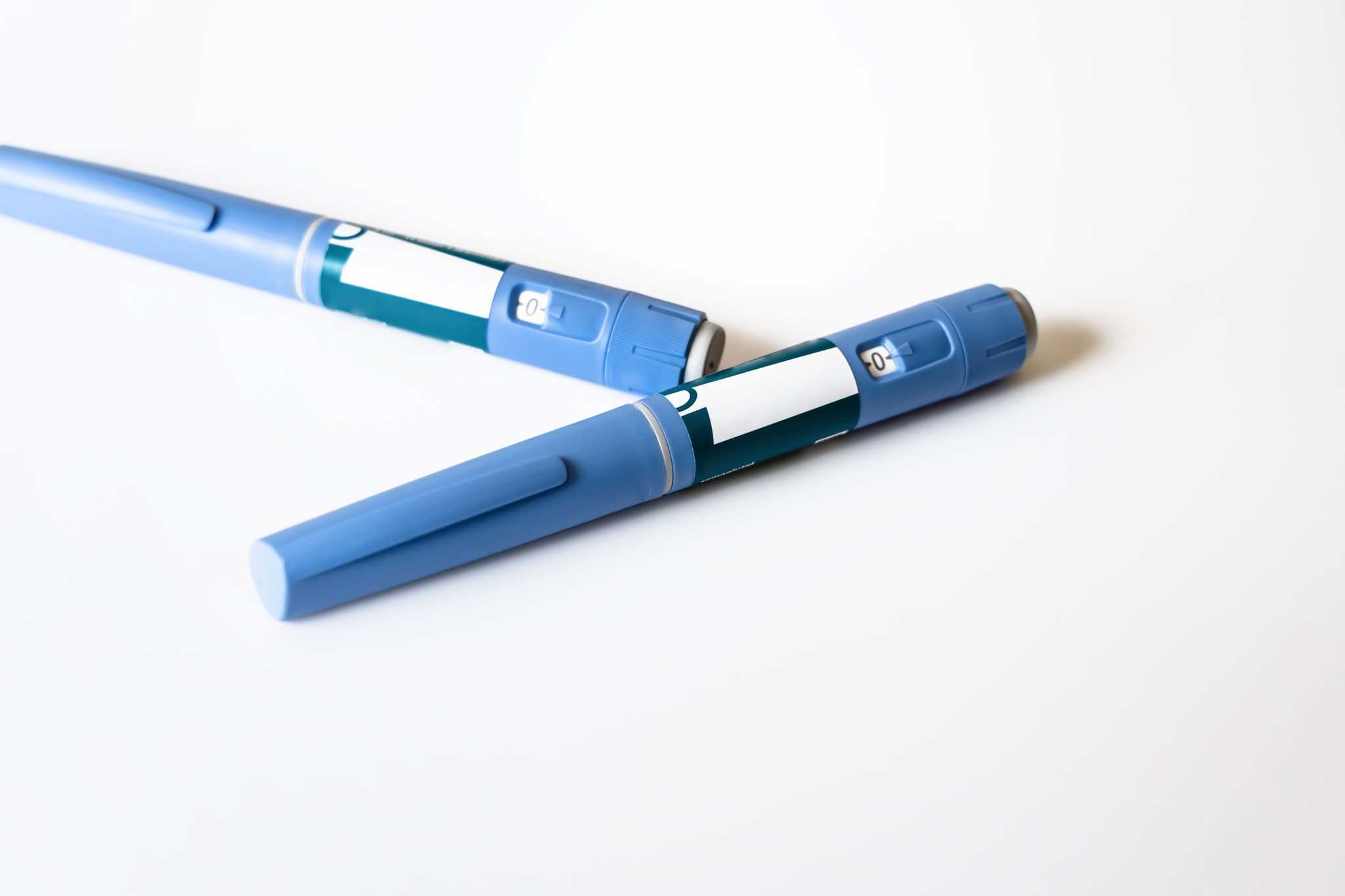
Understanding the Tirzepatide Pen
The tirzepatide injection pen is a pre-filled, single-use medical device designed to deliver a precise dose of tirzepatide safely and easily. It was created to make weekly injections simple for people managing type 2 diabetes or weight loss treatment. Learning how the pen works and how to handle it correctly helps ensure the medicine is both safe and effective.
What the Tirzepatide Pen Is
The tirzepatide pen comes ready to use. Each pen contains one complete dose of medication, meaning you use it once and then throw it away. You do not need to attach a needle, fill the pen, or measure the dose. The pen is pre-assembled and disposable, reducing the chance of dosing errors.
The medicine inside the pen is a clear, colorless liquid. It contains the active ingredient tirzepatide, a compound that helps the body control blood sugar and support weight loss. The pen is available by prescription only, so you should always use it under the direction of your healthcare provider.
Main Parts of the Tirzepatide Pen
Understanding each part of the pen will help you feel more confident when using it. Although the design may vary slightly depending on the brand (for example, Mounjaro® or Zepbound®), all tirzepatide pens include the following key components:
- Needle Cap:
This is the small cover at the tip of the pen that protects the needle before use. You remove the cap only when you are ready to inject. The needle is not visible until after use, which helps reduce anxiety for people who are uncomfortable with needles. - Dose Window or Indicator:
This small, clear section shows when the injection is complete. Some pens have a colored bar that moves or clicks when the full dose has been delivered. - Activation Button:
This is the button you press to start the injection. Once pressed, the medicine flows automatically into the skin. The button must be held down until the injection is finished. - Safety Lock or Cap:
A small lock or twist cap ensures that the pen is not activated by mistake. This feature prevents accidental injections during handling or transport.
Each part plays an important role in safe and accurate dosing. Before you use the pen, take a moment to identify these parts and read the instruction leaflet that comes in the package.
Available Strengths
Tirzepatide pens come in different dose strengths, allowing your healthcare provider to adjust your treatment gradually. Common strengths include:
- 2.5 mg – usually the starting dose
- 5 mg
- 7.5 mg
- 10 mg
- 12.5 mg
- 15 mg
Each pen is color-coded to help prevent confusion between doses. You should always check the label before injecting to make sure you are using the correct strength. Never try to combine doses or use two pens at once.
Your doctor will usually start you on a low dose and increase it slowly over several weeks. This gradual increase helps your body adjust and lowers the chance of stomach side effects like nausea.
Storage and Handling Guidelines
Proper storage keeps the medicine stable and effective. Tirzepatide pens should be:
- Stored in a refrigerator between 36°F and 46°F (2°C to 8°C).
- Protected from light by keeping them in the original box until use.
- Never frozen. If a pen has been frozen or left in extreme heat, it should be discarded.
- Kept out of reach of children and pets.
If you plan to use your pen soon, you can take it out of the refrigerator and let it reach room temperature (around 30 minutes) before injection. This helps reduce discomfort during the shot.
If needed, unopened pens can stay at room temperature (up to 86°F / 30°C) for a limited time—usually up to 21 days, depending on manufacturer guidelines. Always check the specific storage instructions provided in the package insert.
Checking Before Use
Before you inject, always do a quick safety check:
- Confirm your name and dose on the pen label.
- Check the expiration date. Do not use the pen if it has expired.
- Inspect the solution. It should be clear and colorless, without any cloudiness or particles.
- Make sure the pen has not been dropped or damaged. A cracked or broken pen should be replaced.
These steps take only a few seconds but are vital for ensuring safe and effective treatment.
Shelf Life and When to Discard
Each tirzepatide pen is single-use. After injection, dispose of the pen immediately in a FDA-approved sharps container. Do not attempt to reuse or recap the pen. Even though it may appear there is liquid left, the pen is designed to deliver one full, preset dose only.
Unused pens can typically be stored until the expiration date listed on the package, provided they have been stored correctly. If you are unsure whether a pen is still good, consult your pharmacist or healthcare provider before use.
The tirzepatide pen is designed for simple, once-weekly use with built-in safety and accuracy features. By learning how to identify each part, check your dose, and store the pen properly, you can use it confidently and safely. Correct handling and storage not only protect the medication’s effectiveness but also ensure that each injection delivers the exact dose your body needs for better blood sugar control and weight management.
Step-by-Step Instructions: How to Use the Tirzepatide Pen
Using your tirzepatide pen correctly is important for safety, comfort, and to make sure you get the full benefit of your medication. This step-by-step guide will walk you through everything you need to know — from preparation to injection and disposal — in simple, clear language.
Tirzepatide pens are single-use, prefilled devices that contain one full dose. You will use a new pen each week. Do not share your pen with anyone, even if the needle looks clean. Sharing can spread infections and is not safe.
Step 1: Wash your hands and prepare your injection site
Start by washing your hands with soap and warm water. Clean hands help prevent infection.
Next, choose an injection site. You can inject tirzepatide into:
- Your abdomen (stomach area) — at least 2 inches away from your belly button.
- Your thigh — either front or outer side.
- The back of your upper arm — if someone else can give you the injection.
Rotate your injection site each week to avoid irritation or bruising. Do not inject into the same exact spot two times in a row. Avoid areas with scars, stretch marks, or hard or tender skin.
If your healthcare provider recommends it, you may clean the injection area with an alcohol swab. Allow the skin to dry completely before injecting.
Step 2: Allow the pen to reach room temperature
Take your pen out of the refrigerator about 30 minutes before using it.
Letting it warm up to room temperature makes the injection more comfortable. Do not use external heat (like a microwave or hot water) to warm the pen.
Do not freeze the pen. If it has ever been frozen, throw it away and use a new one.
Step 3: Check the pen label, dose, and expiration date
Always confirm that you are using the correct dose prescribed by your doctor (for example, 2.5 mg, 5 mg, or 7.5 mg). Each pen is color-coded by dose, but reading the label is still essential.
Check the expiration date printed on the pen. Never use a pen that is expired.
Make sure the pen label matches your prescription (for example, “Mounjaro” or “Zepbound,” both contain tirzepatide). If the label looks damaged, faded, or unclear, or if the pen looks broken, do not use it.
Step 4: Remove the cap and inspect the solution
Hold the pen firmly and pull off the gray or colored cap straight — do not twist it.
You should now see the small needle end under the cap area. Never touch the needle.
Look through the pen window to check the liquid inside. The medicine should be clear and colorless. Do not use it if the liquid looks cloudy, thick, has particles, or is discolored. In that case, dispose of the pen safely and use a new one.
Once the cap is removed, use the pen right away. Do not put the cap back on.
Step 5: Place the pen at a 90° angle against your skin
Position the pen straight up and down (at a 90-degree angle) on your chosen injection site.
Hold the pen steady and make sure the tip is flat against your skin. Do not press the activation button yet.
This pen is designed for subcutaneous injection, meaning the medication is delivered just under the skin, not into the muscle. Keeping the pen flat and steady helps ensure proper delivery.
Step 6: Press and hold the activation button until the injection is complete
Press the injection button firmly. You should hear a click — this means the injection has started.
Keep the pen pressed firmly against your skin. After the first click, wait for about 10 seconds to make sure the full dose is delivered.
Some pens also make a second click when the injection is complete — follow the timing instructions on your brand’s package insert if you are unsure.
Do not move the pen until the injection is finished. Moving it early may prevent you from getting the full dose.
Afterward, lift the pen straight away from your skin. You can apply gentle pressure with a tissue or cotton ball if a small drop of blood appears — this is normal. Do not rub the area.
Step 7: Dispose of the pen safely
Each tirzepatide pen is made for one-time use only.
Once the injection is complete, immediately throw the pen away in a FDA-cleared sharps disposal container.
If you don’t have a medical sharps container, you can use a heavy-duty plastic container with a secure, puncture-resistant lid — such as an empty laundry detergent bottle. Label it clearly as “Do Not Recycle – Sharps.”
Never throw used pens in household trash or recycling bins. When your sharps container is full, follow local disposal rules or ask your pharmacy about drop-off sites.
Step 8: Wash your hands and record your injection
After disposal, wash your hands again with soap and water.
If you track your doses (especially for diabetes), write down the injection date, time, and site. Keeping a log helps your healthcare provider review your progress and ensure you are on schedule.
Tips for comfort and consistency
- Inject your dose on the same day each week at roughly the same time.
- Try to make injection day part of your weekly routine (for example, every Monday morning).
- Use a reminder on your phone or calendar to help you stay consistent.
- If you experience pain or redness, try using a different site the next time.
- Do not mix tirzepatide with insulin or other medications in the same injection.
Administering tirzepatide becomes simple once you understand the steps.
Always handle the pen with care, follow the same routine each week, and talk to your healthcare provider if anything feels confusing or uncomfortable. Proper technique not only helps your medicine work better but also keeps you safe and confident in your treatment routine.
Dosing Schedule and Titration
Getting the right dose of tirzepatide is important for both safety and success. Tirzepatide must be started slowly and increased over time. This slow, step-by-step approach is called titration. It helps your body adjust to the medicine while reducing side effects like nausea or stomach upset. This section explains how dosing works, what to do if you miss a dose, and why staying consistent matters.
Starting Dose: The First Step
Everyone who begins tirzepatide usually starts with the same low dose — 2.5 milligrams once a week. This small amount is used for the first four weeks. The purpose of this early stage is not to control blood sugar or cause major weight loss yet. Instead, it allows your body to get used to the medicine’s effects.
During this first month, your stomach may take longer to empty after meals, and you may feel full sooner. Some people notice mild nausea, constipation, or diarrhea. These effects are common at the start and usually improve within a few weeks. Drinking enough water, eating smaller portions, and avoiding high-fat or greasy foods can help you feel better as your body adjusts.
Increasing the Dose Step by Step
After four weeks at the starting dose, your doctor will usually increase your dose to 5 milligrams once a week. If your body handles this amount well, you may continue to increase the dose every four weeks as needed. The next doses typically move up by 2.5 milligrams each time — for example, 7.5 milligrams, then 10 milligrams, and possibly higher.
Your doctor will decide how far to go depending on your blood sugar control, weight loss progress, and how you feel. Some people stay at a middle dose such as 7.5 or 10 milligrams because it works well for them. Others may increase gradually to 12.5 or 15 milligrams for the best effect.
If you have strong nausea, vomiting, or stomach pain after increasing your dose, your doctor might keep you at your current level for longer before going higher. The goal is not to rush. It is more important to find a dose that works well for your body with the fewest side effects.
The Weekly Routine
Tirzepatide is taken once every week. You can inject it at any time of the day — morning or evening — and it does not need to be taken with food. What matters most is consistency. Choose a day that fits your schedule, such as Sunday, and stick to that same day each week.
Consistency keeps the amount of tirzepatide steady in your system, which helps it work properly. You may find it helpful to use a phone alarm or calendar reminder so you do not forget your injection. If you ever need to change your injection day, pick a new day that is at least three days (72 hours) after your last injection. After that, continue using the new day each week.
If You Miss a Dose
Missing a dose can happen to anyone, but you should know what to do to stay safe.
- If less than four days (96 hours) have passed since your missed injection, take the missed dose as soon as you remember. Then return to your regular schedule.
- If more than four days have passed, skip the missed dose. Just take your next dose on your usual injection day.
- Never inject two doses close together or double your dose to make up for a missed one. Taking doses too close together can increase the risk of nausea, vomiting, or other side effects.
If you often forget your doses, try linking the injection to something you always do weekly — for example, injecting every Sunday evening after dinner. This habit can make it easier to remember.
Why the Slow Increase Is Important
Tirzepatide affects the hormones that control appetite and digestion. It slows the emptying of food from your stomach and helps lower blood sugar after meals. Increasing the dose too quickly can cause uncomfortable side effects such as nausea, stomach cramps, or loss of appetite. That is why titration — the gradual increase — is key.
Each step gives your body time to adjust. This method not only improves comfort but also helps people stay on the medicine long term. Your doctor will monitor your progress, checking your blood sugar levels, body weight, and overall tolerance before moving to the next dose. The slow increase helps balance effectiveness with comfort.
Individualized Dosing
Not everyone will need the same dose. Your healthcare provider will personalize your plan based on your body’s response and medical history. People with diabetes might need adjustments to other medications, such as insulin or sulfonylureas, to avoid low blood sugar. Those using tirzepatide for weight management might focus on how appetite and eating patterns change instead.
Your provider will also consider factors such as your kidney or liver health and whether you are taking other prescription drugs. It is important not to change your dose on your own. Always follow medical advice and report any unusual symptoms, such as severe stomach pain or persistent nausea.
Staying Consistent for Best Results
Tirzepatide works best when taken regularly over time. Missing doses or stopping suddenly can reduce its benefits. For people with diabetes, this could mean higher blood sugar levels. For people using it for weight management, it may slow progress or cause weight regain.
Be patient and consistent. Tirzepatide is designed to work gradually, improving your health step by step. The slow dosing schedule helps your body adapt, lowers the risk of side effects, and increases the chances of long-term success.
Start low, go slow, and stay consistent. Tirzepatide’s weekly dosing plan is simple but must be followed carefully. The slow titration process gives your body time to adjust, ensures the medicine works safely, and helps you reach your blood sugar or weight goals more comfortably. Always keep in touch with your healthcare provider about how you are feeling as your dose changes.
Common Side Effects and How to Manage Them
Tirzepatide is a medication that helps people manage type 2 diabetes and lose weight by working on hormones that control blood sugar and appetite. Like most medicines, it can cause side effects. Most of these are mild and go away as your body gets used to the medication. However, it is important to understand what you might experience and how to manage it safely.
This section explains the most common side effects of tirzepatide, why they happen, what you can do to reduce them, and when to seek medical help.
Gastrointestinal Side Effects
The most common side effects of tirzepatide affect the digestive system. These include:
- Nausea (feeling sick to your stomach)
- Vomiting
- Diarrhea
- Constipation
- Loss of appetite or feeling full quickly
These side effects are usually mild to moderate and often occur when you first start taking the medication or when your dose increases. This happens because tirzepatide slows down how fast food leaves your stomach. It also affects the brain areas that control hunger, so you feel full sooner.
Tips to manage gastrointestinal symptoms:
- Start with the prescribed low dose. Tirzepatide treatment begins at a low dose (usually 2.5 mg weekly) to help your body adjust. Your doctor will gradually increase the dose every few weeks if you tolerate it well.
- Eat smaller meals more often. Large meals can make nausea or stomach pain worse. Choose smaller portions and chew food slowly.
- Avoid greasy, fried, or spicy foods. These can irritate your stomach and worsen nausea.
- Stay hydrated. If you experience vomiting or diarrhea, drink small sips of water or clear fluids throughout the day to prevent dehydration.
- Rest after eating. Avoid lying down right after meals, as this can increase discomfort.
- Tell your doctor if symptoms persist. If nausea or vomiting lasts more than a few days, or if you cannot keep fluids down, your healthcare provider may recommend temporary dose adjustments or supportive medication.
Most people find that these digestive symptoms improve after the first few weeks of treatment.
Injection Site Reactions
Mild redness, itching, or tenderness may occur where you inject the medication. This is not dangerous and usually goes away within a few hours to days.
How to reduce injection site reactions:
- Rotate injection sites each week (abdomen, thigh, or upper arm).
- Clean the skin with alcohol before injecting.
- Let the alcohol dry completely before injecting to reduce irritation.
- Do not inject into bruised, hard, or scarred skin.
- If redness or pain lasts more than a few days, talk to your doctor.
Low Blood Sugar (Hypoglycemia)
Tirzepatide alone rarely causes low blood sugar (hypoglycemia). However, the risk increases if you use it with insulin or sulfonylurea medications (such as glipizide or glyburide).
Symptoms of low blood sugar include:
- Shakiness or dizziness
- Sweating
- Fast heartbeat
- Hunger
- Blurred vision
- Confusion or irritability
How to prevent and manage hypoglycemia:
- Do not skip meals. Eat regular, balanced meals with carbohydrates and protein.
- Check your blood sugar as directed, especially if you also take insulin.
- Keep a quick source of sugar with you, such as glucose tablets or fruit juice.
- If you experience low blood sugar often, ask your doctor about adjusting your insulin or other diabetes medication doses.
Serious but Rare Side Effects
While uncommon, tirzepatide can cause serious side effects that require medical attention.
Pancreatitis (inflammation of the pancreas)
Pancreatitis is a rare but serious reaction. Symptoms may include:
- Severe, constant stomach pain (that may spread to your back)
- Nausea or vomiting that does not stop
- Fever or a fast heartbeat
If you experience these symptoms, stop taking tirzepatide and contact your healthcare provider immediately or go to the emergency room.
Gallbladder problems
Some people may develop gallstones or inflammation of the gallbladder. Signs include:
- Pain in the upper right side of the abdomen
- Nausea or vomiting
- Yellowing of the skin or eyes (jaundice)
Allergic reactions
Although very rare, allergic reactions can occur. Signs include:
- Rash or itching
- Swelling of the face, lips, or throat
- Trouble breathing
Seek emergency medical care if any of these occur.
Other Possible Side Effects
Other side effects that may occur include:
- Fatigue or tiredness
- Mild headache
- Dizziness (especially if blood sugar drops too low)
- Mild injection-site bruising
These symptoms are usually temporary and improve as your body adjusts to the medicine.
When to Call Your Doctor
Call your healthcare provider if you experience:
- Persistent or severe nausea, vomiting, or diarrhea
- Signs of dehydration (dry mouth, dizziness, little or no urine)
- Severe stomach or abdominal pain
- Symptoms of low blood sugar that do not improve after treatment
- Any sign of an allergic reaction
Your doctor may suggest slowing your dose increase or using additional medications to relieve symptoms. Never stop or change your dose without medical advice.
Most people taking tirzepatide experience mild side effects that go away on their own. Nausea and digestive issues are the most common, especially at the beginning of treatment. Staying hydrated, eating small meals, and allowing your body time to adjust can help. However, you should always watch for warning signs of more serious problems like pancreatitis or allergic reactions.
By learning how to manage side effects and communicating with your healthcare provider, you can continue tirzepatide treatment safely and achieve the best results for blood sugar control and weight management.
Storage, Handling, and Disposal
Proper storage, handling, and disposal of your tirzepatide pen are very important for keeping the medicine safe and effective. Tirzepatide (sold under brand names like Mounjaro® and Zepbound®) is a prescription injection that contains a sensitive biological medicine. Because of this, it can lose its strength or become unsafe if not stored or handled correctly. The following information will help you understand how to care for your tirzepatide pens from the day you bring them home until the day you dispose of them.
Storage Before Use
Tirzepatide pens should be stored in the refrigerator at a temperature between 36°F and 46°F (2°C to 8°C). This is the standard temperature for most biological medications.
Keep the pen in its original box until you are ready to use it. The box protects the pen from light, which can damage the medication over time.
Do not freeze the pen. If the pen has ever been frozen, you should throw it away — even if it looks fine. Freezing changes the structure of the medication, which can make it unsafe or ineffective.
Do not store the pen in a part of the refrigerator where the temperature often changes, such as the door or near the freezer section.
If you plan to travel, place the pen in an insulated bag with a cold pack, but make sure the pen does not touch the ice pack directly. Direct contact could cause freezing. Keep the pen away from extreme heat or sunlight.
Storage After Removing from the Refrigerator
Before you inject, it is a good idea to let the tirzepatide pen sit at room temperature for about 30 minutes. This makes the injection more comfortable and helps prevent stinging under the skin.
Once a pen has been taken out of the refrigerator, it can stay at room temperature (up to 86°F or 30°C) for a maximum of 21 days. After 21 days, if you have not used the pen, you must throw it away — even if it has been stored safely and looks normal.
Never put a pen back into the refrigerator once it has been left out for several days. Temperature changes can affect the medicine’s quality.
Always check the expiration date on the pen label before you use it. If the expiration date has passed, do not use the pen. Expired medication may not work properly and could cause harm.
Inspecting the Pen Before Use
Before each injection, carefully inspect your tirzepatide pen.
Look through the viewing window to check that the liquid inside is clear and colorless.
Do not use the pen if the liquid looks cloudy, discolored, or contains any particles.
Also, make sure the pen cap is firmly attached before removing it — this ensures it has not been used or damaged.
If the pen has been dropped or looks cracked, bent, or damaged, do not use it. Get a new pen from your pharmacy or contact your healthcare provider for guidance.
Traveling With Tirzepatide Pens
When traveling, keep your tirzepatide pens in a temperature-controlled container. Small insulated travel pouches with ice packs are ideal.
Always carry the pens with you in your hand luggage, not checked baggage, because cargo areas of planes can become too cold or too hot.
If you are traveling by car, do not leave the pen inside the vehicle for long periods. The temperature in a parked car can quickly rise above 100°F (37°C) or drop below freezing, both of which can spoil the medicine.
If you are staying in a hotel, store the pen in a mini-fridge or at least a cool, dry place out of direct sunlight.
Handling the Pen Safely
Tirzepatide pens are single-use devices. Each pen contains one pre-measured dose.
You should never try to reuse a pen or share it with someone else, even if you change the needle. Sharing can spread infections and is unsafe.
Once the pen has been used, it cannot be refilled or reactivated.
Always handle the pen gently. Avoid shaking or dropping it.
Keep it out of reach of children and pets. Store it in a secure area, ideally in its original box, until you are ready for your next injection.
Proper Disposal
After you inject your dose, you must safely dispose of the used pen. Tirzepatide pens contain a needle that is permanently attached, so it is important to handle them carefully.
- Immediately after injection, place the entire used pen in an FDA-cleared sharps disposal container. These containers are usually made of hard plastic and are puncture-resistant.
- If you do not have a sharps container, you can use a heavy-duty household container such as an empty laundry detergent bottle with a secure lid. Label it clearly as “Do Not Recycle: Contains Used Needles.”
- Never throw used pens into household trash, recycling bins, or public waste baskets.
- When the container is about three-quarters full, follow your local or pharmacy guidelines for safe disposal. Some communities or pharmacies offer drop-off programs or mail-back options for sharps.
Key Safety Tips
- Never reuse or share pens.
- Do not store pens in the bathroom, near stoves, or in hot cars.
- Keep all pens away from children.
- Always check the solution before each use.
- Dispose of pens properly to protect others and the environment.
Storing and handling your tirzepatide pens correctly helps ensure that each dose you take is safe, sterile, and effective.
Always follow the manufacturer’s instructions and your healthcare provider’s advice about temperature limits and disposal.
Taking these simple steps — refrigerating properly, avoiding extreme heat or cold, inspecting the medicine, and using safe disposal methods — protects your health and ensures you get the full benefit of your tirzepatide treatment.
Safety Precautions and Monitoring
Tirzepatide is a powerful medicine that can greatly help people with type 2 diabetes and those managing their weight. However, like any prescription medication, it needs to be used carefully. Understanding how to monitor your progress and stay alert for warning signs is key to safe and effective treatment. This section explains what safety steps to follow, what tests to expect, and when to contact your healthcare team.
Regular Blood Glucose Monitoring (for People with Diabetes)
If you are using tirzepatide to manage diabetes, you will need to check your blood sugar levels regularly. This helps you and your healthcare provider see how well the medication is working.
- Daily checks: Many people test fasting blood glucose in the morning and sometimes after meals.
- Record results: Keep a written or digital log of your readings. This helps your doctor adjust your dose if needed.
- Watch for patterns: If your readings are often too high or too low, share this information with your healthcare team.
Tirzepatide can lower blood glucose, especially when used with insulin or certain oral diabetes medicines like sulfonylureas. If your blood sugar drops too low, you may feel shaky, sweaty, dizzy, or confused. Always carry a quick source of sugar, such as glucose tablets or fruit juice, to treat low blood sugar quickly.
Weight and Lifestyle Monitoring
For people using tirzepatide for weight management, regular tracking helps measure progress.
- Weigh yourself weekly: Try to weigh yourself at the same time each week, preferably in the morning before eating.
- Track measurements: Some people also track waist size or body mass index (BMI).
- Maintain healthy habits: Tirzepatide works best when combined with a healthy diet and regular physical activity. It is not a substitute for lifestyle changes but a tool to support them.
Your healthcare provider might recommend a follow-up every few months to check your progress, review your food habits, and ensure you are losing weight safely.
Routine Laboratory Tests
Your doctor may order periodic blood tests to monitor how your body is responding to tirzepatide. These tests can include:
- HbA1c test: Measures your average blood glucose over the past three months.
- Kidney and liver function tests: Tirzepatide is processed through the body’s natural filtering systems, so checking organ function helps ensure safety.
- Lipid profile: Monitors cholesterol and triglyceride levels, which can change with weight loss and improved glucose control.
- Electrolytes: In cases of persistent vomiting or diarrhea, your doctor may test for dehydration or mineral imbalances.
These routine labs are usually done every 3 to 6 months, depending on your condition and treatment response.
Drug Interactions and Cautions
Tirzepatide may interact with other medicines. It is very important to inform your doctor or pharmacist about everything you take — including over-the-counter drugs, vitamins, and herbal supplements.
Some medicines that can interact include:
- Insulin and sulfonylureas: These can increase the risk of low blood sugar when used with tirzepatide.
- Other diabetes medications: Combining multiple GLP-1 receptor agonists is not recommended.
- Oral medications: Because tirzepatide slows stomach emptying, it may affect how quickly other pills are absorbed. Your doctor might suggest taking them at a different time of day.
Never change or stop your medicines without talking to your doctor first.
Special Situations: Pregnancy, Breastfeeding, and Medical Conditions
Tirzepatide is not recommended during pregnancy because its effects on unborn babies are not fully known. Women who plan to become pregnant should discuss stopping the medicine in advance. Healthcare providers may recommend waiting at least one month after the last dose before trying to conceive.
It is also not advised during breastfeeding, since it is unclear whether tirzepatide passes into breast milk.
People with certain medical conditions should use extra caution:
- Pancreatitis: Anyone with a history of pancreatitis should avoid tirzepatide unless cleared by a doctor.
- Severe stomach or intestinal problems: Because tirzepatide slows digestion, it can worsen certain gastrointestinal diseases.
- Kidney or liver disease: Dose adjustments or close monitoring may be needed.
- Thyroid C-cell tumors: Do not use tirzepatide if you or your family have a history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia type 2 (MEN 2).
Always discuss your full medical history before starting treatment.
Recognizing Warning Signs
While most people tolerate tirzepatide well, it is essential to recognize when something may be wrong.
Contact your healthcare provider immediately if you experience:
- Severe stomach pain that won’t go away
- Persistent vomiting
- Yellowing of the eyes or skin (sign of liver issues)
- Swelling of the neck or hoarseness (possible thyroid problem)
- Dizziness, fainting, or confusion
- Allergic reactions such as rash, itching, or swelling of the face and throat
These symptoms may indicate a serious side effect that needs urgent care.
Importance of Regular Medical Follow-Up
Ongoing medical supervision ensures that tirzepatide remains safe and effective for you. Most patients should schedule follow-up visits every 1 to 3 months at the beginning of therapy, then every 3 to 6 months once the dose is stable. During these visits, your provider will:
- Review blood test results
- Check for side effects
- Adjust your dose if needed
- Discuss diet, physical activity, and other medications
Do not skip appointments even if you feel well — monitoring helps prevent complications and keeps your treatment on track.
Safety and monitoring are essential parts of using tirzepatide. Always take it as prescribed, track your results, and stay in contact with your healthcare team. Watch for side effects and never ignore warning signs. With proper care, regular monitoring, and professional guidance, tirzepatide can be a safe and effective treatment for improving blood sugar control and supporting healthy weight loss.

When to Contact a Healthcare Provider
Even though tirzepatide is a safe and effective medicine when used correctly, there are times when you should contact your healthcare provider right away. Knowing when to reach out can help prevent serious health problems and ensure your treatment stays safe and effective. This section explains the main reasons to contact your doctor or nurse, what to do if you miss a dose or make a mistake, and the warning signs you should never ignore.
When You Have Ongoing or Severe Side Effects
Some side effects are common when starting tirzepatide, such as mild nausea, diarrhea, or a reduced appetite. These often improve after a few weeks as your body adjusts.
However, if these symptoms become severe, constant, or worsen over time, it’s important to contact your healthcare provider. You should especially call if you:
- Cannot keep food or fluids down due to vomiting.
- Have severe or persistent abdominal (stomach) pain.
- Feel dizzy, lightheaded, or weak for several hours.
- Have diarrhea lasting longer than two days.
- Notice dehydration (dry mouth, reduced urination, dark urine).
These symptoms can lead to dehydration or signal a more serious reaction that needs medical attention.
If You Feel Sudden or Severe Abdominal Pain
Severe stomach or upper abdominal pain that does not go away or radiates to your back could be a sign of pancreatitis, a rare but serious inflammation of the pancreas.
Other warning signs include:
- Nausea and vomiting that start suddenly and don’t improve.
- Fever or a rapid heartbeat.
- Tenderness or swelling around your upper abdomen.
If you suspect pancreatitis, stop using tirzepatide immediately and call your healthcare provider or go to the emergency room. Your doctor may run blood tests or imaging scans to check your pancreas before restarting the medicine.
When You Notice Allergic Reactions
Although uncommon, allergic reactions can happen after using tirzepatide. These can range from mild to severe (anaphylaxis).
Seek immediate medical care if you experience:
- Swelling of your face, lips, tongue, or throat.
- Difficulty breathing or swallowing.
- Hives, rash, or itching after injection.
- Rapid heartbeat or chest tightness.
For mild skin redness or itching at the injection site, contact your healthcare provider if it does not go away within a few days or gets worse. You may need a different injection site or another treatment.
If You Have Signs of Low Blood Sugar (Hypoglycemia)
Tirzepatide by itself rarely causes low blood sugar. However, if you take it with insulin or other diabetes medicines like sulfonylureas, your risk increases.
Call your healthcare provider if you frequently notice symptoms such as:
- Sweating, shakiness, or a fast heartbeat.
- Dizziness, confusion, or headache.
- Blurred vision or trouble concentrating.
If you experience severe low blood sugar (where you can’t eat or drink safely), seek emergency help right away. You may need a dose adjustment of your other diabetes medications.
When You Miss a Dose or Inject Incorrectly
If you miss a dose, inject it as soon as possible within four days (96 hours) after your scheduled time. If more than four days have passed, skip that dose and inject the next one at your regular time.
Do not inject two doses at once or within three days of each other.
Contact your healthcare provider if you:
- Are unsure when to take your next dose.
- Injected too much by mistake.
- Are not sure the injection worked (for example, if the pen malfunctioned).
Your provider can advise you on the safest next step and prevent possible side effects.
Signs of Overdose or Serious Complications
Too much tirzepatide can cause strong nausea, vomiting, or dangerously low blood sugar.
If you think you took too much, call your local poison control center or go to the emergency room immediately. Bring the pen or packaging with you if possible to help the medical team identify the medication and dose.
Other serious symptoms that require urgent care include:
- Fainting or loss of consciousness.
- Fast or irregular heartbeat.
- Trouble breathing or swallowing.
- Swelling or severe pain at the injection site.
When You Experience Sudden Weight Loss or Appetite Changes
Tirzepatide is designed to help with gradual weight loss. However, very fast or extreme weight loss may signal a problem.
Contact your doctor if:
- You lose more than 5 pounds per week.
- You stop feeling hungry altogether.
- You experience fatigue, dizziness, or weakness.
Your provider may check your dosage or rule out dehydration, nutritional deficiencies, or other underlying issues.
Importance of Regular Follow-Up Visits
Even if you feel fine, regular checkups are an important part of your treatment. These visits allow your healthcare provider to:
- Monitor your blood sugar, HbA1c, and weight progress.
- Check your kidney and liver function if needed.
- Adjust your dose to match your goals and tolerance.
- Review other medicines to prevent drug interactions.
Do not stop or change your dose without talking to your doctor first. Every adjustment should be guided by professional advice.
Contact your healthcare provider any time you notice new, severe, or unusual symptoms while using tirzepatide. It’s always safer to ask questions early rather than wait until problems become serious.
If you experience trouble breathing, swelling, severe stomach pain, or confusion, seek emergency medical help immediately.
Conclusion
Using the tirzepatide pen correctly is one of the most important parts of getting the best results from this medicine. Tirzepatide can help control blood sugar for people with type 2 diabetes, and it can also help reduce body weight for those living with obesity. But how well it works depends not only on the medicine itself, but also on how carefully and consistently it is used. Understanding every step—from preparing the pen to injecting the dose and storing it safely—makes a big difference in safety and results.
The tirzepatide pen is made to be as simple as possible for weekly use, but it still needs attention and care. Each pen contains a single, pre-filled dose that should only be used once. Before every injection, always check the pen label to make sure the dose is correct and that the medicine has not expired. The solution inside should look clear and colorless, never cloudy or with particles floating in it. If anything looks unusual, do not use that pen. Instead, dispose of it properly and use a new one.
Consistency matters. Tirzepatide works best when taken on the same day every week. Choose a day that is easy to remember, such as Sunday evening or Monday morning, and try to stick to it. Keeping the timing regular helps your body adjust to the medicine and reduces the chance of side effects. If you ever miss a dose, take it as soon as you remember—as long as it has been less than four days (96 hours) since your missed injection. If more time has passed, skip that dose and continue with your next scheduled one. Never take two doses at once to make up for a missed week.
Safe injection technique is key. Always wash your hands and clean the injection site before using the pen. The most common injection areas are the abdomen, thigh, or upper arm. Rotate injection sites each week to avoid skin irritation or soreness. Hold the pen straight against the skin and press the button firmly until you hear a click. Keep it in place for a few seconds after the injection to ensure the full dose goes in. Once finished, the entire pen should be disposed of in a proper sharps container. Never reuse a pen or try to take it apart.
Side effects can happen, especially when first starting tirzepatide or when the dose is increased. Nausea, stomach discomfort, and reduced appetite are common but often improve as your body gets used to the medicine. Eating smaller meals, staying hydrated, and avoiding greasy or spicy foods can help. However, if you experience severe abdominal pain, vomiting, or dizziness, contact your healthcare provider right away. These could be signs of more serious conditions such as pancreatitis or gallbladder problems, which need medical attention.
Monitoring is another key part of safe use. For people with type 2 diabetes, regular blood sugar checks help track how well the medicine is working. Your doctor may also order blood tests for HbA1c, liver function, or kidney function during treatment. For those using tirzepatide mainly for weight management, keeping a weekly weight record can help you see progress over time. It is also important to note any unusual symptoms or patterns, such as fatigue, lightheadedness, or significant changes in appetite. Always share these with your healthcare provider during follow-up visits.
Storage plays a big role in keeping the medicine effective. Tirzepatide pens should be stored in the refrigerator between 36°F and 46°F (2°C–8°C) until ready to use. If needed, a pen can be kept at room temperature for up to 21 days, but it should be protected from direct sunlight and never frozen. Once the pen is used, it should be disposed of safely and not reused or recycled. Following these handling rules helps maintain the quality of the medication and prevents contamination.
Tirzepatide is a powerful treatment, but it is not a cure by itself. It works best when combined with healthy habits, such as balanced eating, physical activity, and regular medical check-ups. Even small improvements in diet and daily movement can greatly enhance the benefits of the medication. For diabetes, it can help lower blood sugar levels and reduce the risk of long-term complications. For weight management, it can support meaningful and sustained weight loss, which can improve heart health and reduce strain on joints and organs.
Finally, never make changes to your tirzepatide dose on your own. Your healthcare provider will guide you on when and how to increase or maintain your dose safely. They will also watch for potential interactions with other medicines, especially if you take insulin, sulfonylureas, or other drugs that lower blood sugar. Always tell your doctor about all medicines and supplements you use, even over-the-counter ones. If you plan to become pregnant, are breastfeeding, or have major health changes, consult your doctor before continuing treatment.
In summary, using the tirzepatide pen safely means paying attention to the details—proper handling, correct injection technique, timely dosing, and open communication with your healthcare team. Each of these steps helps ensure that the medicine can do its job effectively, improving both blood sugar control and weight outcomes. With consistent use, medical monitoring, and healthy lifestyle choices, tirzepatide can be a valuable tool in supporting better long-term health.
Research Citations
European Medicines Agency. (2022). Mounjaro: EPAR—Public assessment report. EMA.
U.S. Food and Drug Administration, Center for Drug Evaluation and Research. (2021). Clinical pharmacology review: NDA 215866 (Mounjaro, tirzepatide). FDA.
U.S. Food and Drug Administration, Center for Drug Evaluation and Research. (2022). Medical review: NDA 215866 (tirzepatide injection). FDA.
European Medicines Agency. (2025). Mounjaro, INN: tirzepatide—Product information (includes multi-dose pre-filled pen details). EMA.
Eli Lilly and Company. (2019). A study to compare the pharmacokinetics of tirzepatide administered subcutaneously by an autoinjector versus prefilled syringe in healthy subjects (Protocol I8F-MC-GPGS). ClinicalTrials.gov document.
Eli Lilly and Company. (2019–present). A study of tirzepatide administered by two different devices (autoinjector vs prefilled syringe) in healthy subjects (NCT04004988) [Clinical trial registry record]. ClinicalTrials.gov.
Medicines and Healthcare products Regulatory Agency (UK). (2024). Module 2.7.2: Summary of clinical pharmacology studies—Mounjaro KwikPen (FOI_24_252). MHRA/UK Gov.
Medicines and Healthcare products Regulatory Agency (UK). (2024). Module 2.7.6: Synopses of individual studies—Mounjaro KwikPen (FOI_24_252). MHRA/UK Gov.
Eli Lilly and Company. (2022). Protocol I8F-MC-GPIP (a): A bioequivalence study to compare the PK of tirzepatide administered by fixed-dose multi-use prefilled pen versus single-dose pen in healthy participants. ClinicalTrials.gov document.
Eli Lilly and Company. (2023). Statistical Analysis Plan—Study I8F-MC-GPIP: Bioequivalence between multi-use prefilled pen and single-dose pen. ClinicalTrials.gov document.
Questions and Answers: Tirzepatide Pen
Tirzepatide pens are prefilled injection devices used to deliver tirzepatide, a medication that helps control blood sugar in adults with type 2 diabetes and support weight loss. Brand names include Mounjaro and Zepbound.
Tirzepatide is a dual GIP and GLP-1 receptor agonist. It mimics natural hormones that regulate blood sugar and appetite, improving insulin sensitivity, lowering glucose, and reducing hunger.
The pen is injected under the skin (subcutaneously) once weekly. It can be injected in the stomach, thigh, or upper arm, rotating sites each time.
No. Tirzepatide pens come prefilled and pre-assembled for single use. You do not need to mix, prime, or attach a separate needle.
If it’s been 4 days (96 hours) or less since the missed dose, take it as soon as possible. If more than 4 days have passed, skip the missed dose and take your next dose on the regular day.
Store unused pens in the refrigerator (36°F–46°F / 2°C–8°C). You may keep a pen at room temperature (below 86°F / 30°C) for up to 21 days. Do not freeze the pens.
Common side effects include nausea, vomiting, diarrhea, decreased appetite, and constipation. These are usually mild and lessen over time.
No. Each tirzepatide pen is single-use only and pre-measured for one injection. Dispose of it in a sharps container after use.
Yes. The FDA approved tirzepatide under the brand Zepbound for chronic weight management in adults with obesity or overweight plus a weight-related condition.
Many people notice reduced appetite within the first few weeks. Blood sugar improvements often occur within weeks, while significant weight loss usually develops over several months.

Dr. Judith Germaine
Dr. Jude (Germaine-Munoz) Germaine, MD is a family physician in Springfield, New Jersey. She is currently licensed to practice medicine in New Jersey, New York, and Florida. She is affiliated with Saint Josephs Wayne Hospital.
