Table of Contents
Introduction
Diabetes is one of the most common chronic diseases in the world today. Millions of people are affected, and the numbers continue to rise every year. Diabetes does not only affect blood sugar levels. Over time, it can damage many parts of the body, including the heart, eyes, nerves, and especially the kidneys. Because of this, doctors and scientists are always looking for new treatments that not only control blood sugar but also protect the organs that diabetes often harms.
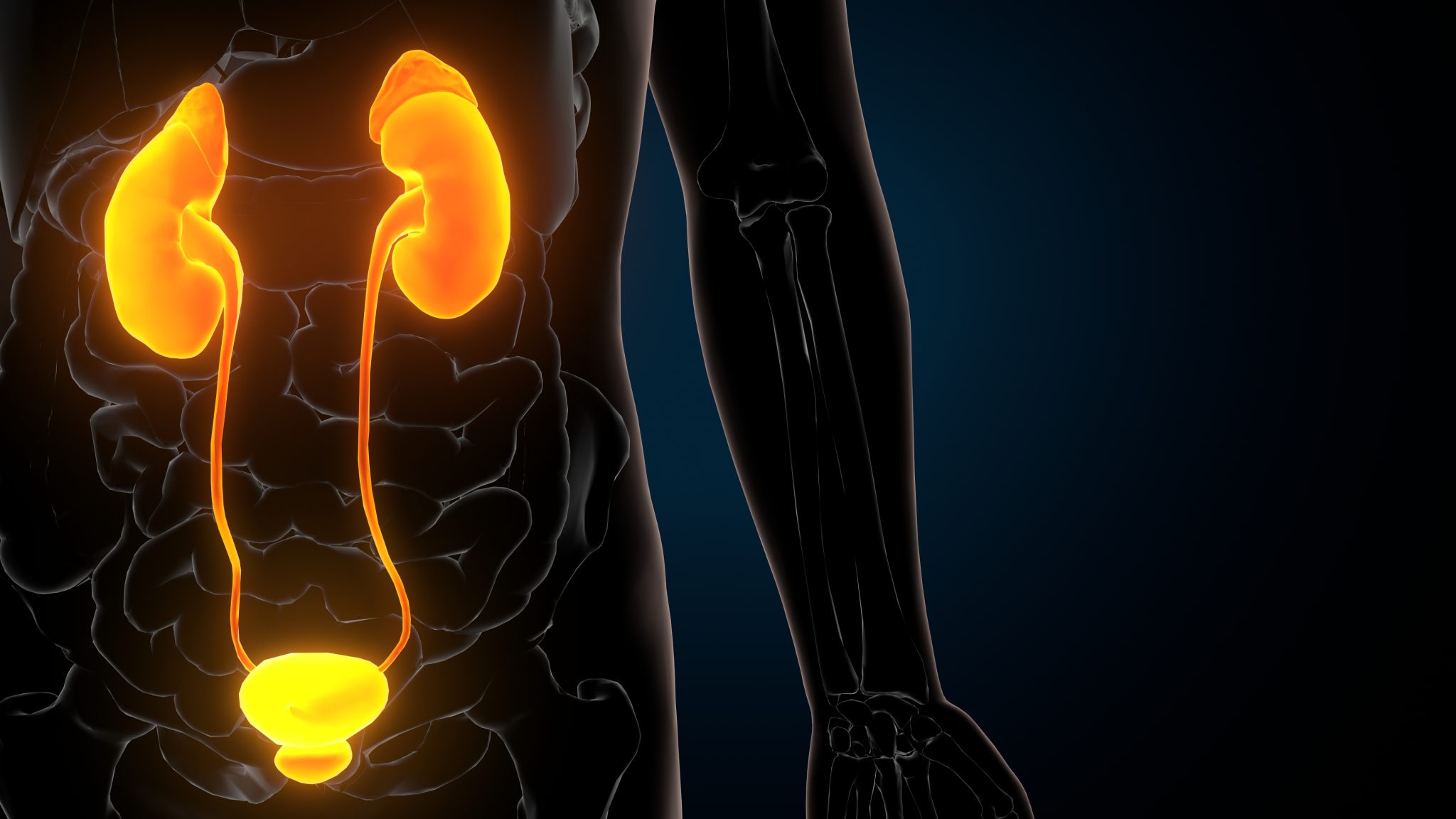
The kidneys play a central role in overall health. These small bean-shaped organs act like filters. They clean the blood by removing waste and extra fluids, and they help keep blood pressure and electrolytes balanced. In people with diabetes, high blood sugar levels can damage the delicate blood vessels in the kidneys. This damage builds up slowly over the years and can lead to a serious condition known as diabetic kidney disease, or DKD. Diabetic kidney disease is one of the leading causes of kidney failure worldwide. For patients, this often means dialysis or a kidney transplant later in life. Preventing or slowing kidney damage is therefore a top priority in diabetes care.
One of the newest medications to treat type 2 diabetes is called tirzepatide. Tirzepatide is different from many older drugs because it does more than lower blood sugar. It belongs to a group of medicines that work on hormones in the gut, called incretins. These hormones, which include GLP-1 (glucagon-like peptide-1) and GIP (glucose-dependent insulinotropic polypeptide), help the body manage food intake, insulin release, and blood sugar levels after meals. Tirzepatide is unique because it works on both GLP-1 and GIP receptors, not just one. For this reason, it is sometimes called a “dual incretin” or “twincretin.”
In clinical trials, tirzepatide has shown very strong effects on lowering blood sugar and promoting weight loss. In fact, the weight reduction it produces has been greater than most other diabetes drugs studied to date. Both blood sugar control and weight management are important for protecting the kidneys in people with diabetes. Because of these results, scientists have started to ask: can tirzepatide also help protect kidney health?
This is an important question, because while some diabetes medications improve blood sugar, they do not always have lasting benefits for the kidneys. Others, like SGLT2 inhibitors, have been proven to protect the kidneys and are now widely used for this reason. Tirzepatide is newer, so the medical community is still learning how it affects long-term kidney outcomes. Patients and doctors alike want to know whether this drug is safe for people who already have kidney problems, whether it can prevent kidney damage in those who do not, and if there are any risks that need careful monitoring.
The connection between diabetes, kidney health, and tirzepatide is also important for another reason. Diabetes and kidney disease often go hand in hand with heart disease. Doctors call this the “cardio-renal-metabolic” connection. When one system in the body is damaged, the others are affected too. Medications that can address blood sugar, weight, heart risk, and kidney health together are especially valuable, because they reduce the overall burden of disease and improve long-term health. Early signs suggest tirzepatide may play such a role, but much more research is needed to be sure.
This article will look closely at the evidence we have so far on tirzepatide and kidney health. It will answer some of the most common questions people search for, such as: Does tirzepatide damage the kidneys, or can it protect them? Is it safe for patients with chronic kidney disease? What about those on dialysis? Does it increase the risk of dehydration or acute kidney injury? And most importantly, what do the long-term studies suggest about the future of tirzepatide in protecting kidney health?
We will begin by reviewing how tirzepatide works and why kidneys are especially vulnerable in diabetes. Then we will move step by step through the latest research findings on how tirzepatide affects kidney function, what risks exist, and how it fits with other kidney-protective therapies. We will also explore what ongoing clinical trials may tell us about its long-term safety and effectiveness. Finally, we will look ahead to the future of diabetes care and how tirzepatide might change treatment strategies.
By the end of this article, the goal is to give readers a clear, evidence-based understanding of where tirzepatide fits in the larger picture of diabetes and kidney health. The topic is complex, but explained simply, it becomes easier to see why researchers are so interested in this medication, what patients and doctors should consider when using it, and how it may shape treatment options in the years to come.
What Is Tirzepatide and How Does It Work?
Tirzepatide is a new type of medicine developed for people with type 2 diabetes. It is different from older treatments because it acts on two natural hormones in the body instead of just one. These hormones are called GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1). Both hormones are part of a group known as incretins. Incretins help the body control blood sugar after eating.
Understanding Incretins
When you eat, your stomach and small intestine release incretin hormones. These signals travel in the blood to the pancreas. The pancreas then produces more insulin, which helps lower blood sugar. At the same time, incretins reduce the release of glucagon, a hormone that normally raises blood sugar. They also slow down how quickly food leaves the stomach, which makes you feel full longer.
Most diabetes drugs work by improving insulin release or by lowering sugar made in the liver. Incretin-based drugs, such as GLP-1 receptor agonists, mimic the body’s natural system. Tirzepatide takes this idea further by targeting two incretin receptors at once.
GLP-1 Receptor Activation
GLP-1 is the incretin that scientists have studied the most. GLP-1 receptor agonist drugs, such as semaglutide or liraglutide, are already widely used to manage type 2 diabetes. These drugs:
- Increase insulin production after meals.
- Decrease glucagon, lowering sugar released by the liver.
- Slow down stomach emptying, which helps reduce appetite.
- Support weight loss in many patients.
Tirzepatide also acts on the GLP-1 receptor, so it shares these benefits.
GIP Receptor Activation
The second part of tirzepatide’s action is unique. It activates the receptor for GIP. In the past, researchers thought GIP was less useful because its effect seemed weaker in people with type 2 diabetes. However, new studies showed that combining GIP with GLP-1 could have a stronger effect than GLP-1 alone.
By stimulating the GIP receptor, tirzepatide may:
- Further boost insulin release in a blood sugar–dependent way.
- Work together with GLP-1 to improve blood sugar control.
- Add extra support for weight loss and metabolism.
This dual action is sometimes described as a “twincretin” effect—a combination of two incretin pathways.
Why This Matters for Diabetes
Type 2 diabetes is a complex disease. It is not only about high blood sugar, but also about problems with weight, appetite, and how the body uses energy. Because tirzepatide works in more than one way, it addresses several of these problems at once:
- Better blood sugar control – lowers fasting glucose and after-meal spikes.
- Weight reduction – helps patients lose more weight than GLP-1 drugs alone.
- Metabolic improvements – may improve blood pressure, cholesterol, and fatty liver disease.
This makes tirzepatide an important step forward compared to medicines that act on a single pathway.
How Tirzepatide Might Affect the Kidneys
The kidneys are very sensitive to blood sugar, blood pressure, and body weight. Over time, high sugar levels damage small blood vessels in the kidneys, leading to diabetic kidney disease. Weight gain, high cholesterol, and high blood pressure can make this worse.
Tirzepatide may protect kidney health indirectly because:
- It lowers blood sugar, reducing stress on the kidneys.
- It helps people lose weight, which can lower blood pressure.
- It improves cardiovascular health, and the heart and kidneys are closely linked.
- It may reduce albuminuria (protein in the urine), which is an early sign of kidney damage.
Scientists are still studying these effects in long-term clinical trials, but the results so far suggest potential benefits beyond blood sugar control.
Comparison to GLP-1 Only Drugs
To understand tirzepatide better, it helps to compare it with older GLP-1 receptor agonists. Both drug types lower blood sugar and support weight loss. However, studies show tirzepatide may cause greater weight loss and stronger blood sugar improvements than GLP-1 drugs alone. This is likely due to the added action of GIP.
In trials, patients taking tirzepatide lost up to 20% of their body weight in some cases. This is more than what is usually seen with GLP-1–only therapies. For people with diabetes and kidney risk, this weight reduction could be very important.
Tirzepatide is a new kind of diabetes medicine that acts on two incretin hormones, GIP and GLP-1. By combining these actions, it improves blood sugar control, reduces appetite, and supports weight loss. Because diabetes and obesity are closely tied to kidney disease, these effects may also help protect the kidneys.
Why Are Kidneys a Key Concern in Diabetes?
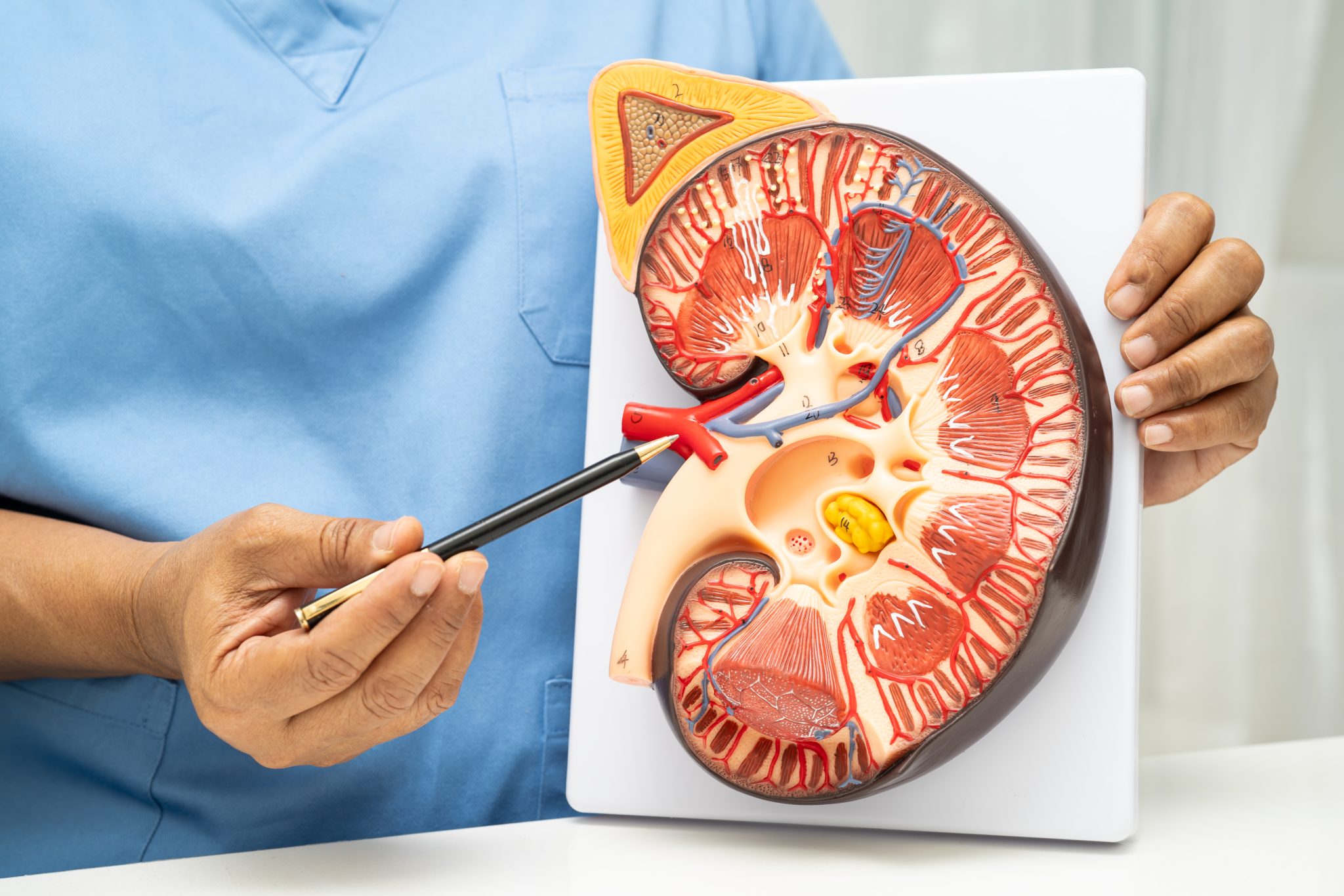
Diabetes is one of the leading causes of kidney disease worldwide. To understand why, it is helpful to know what the kidneys do and how diabetes changes their normal function. The kidneys are small, bean-shaped organs that act as the body’s natural filters. They remove waste products, balance fluids, and help control blood pressure. When diabetes is not well managed, the kidneys can slowly become damaged. This type of damage is called diabetic kidney disease (DKD) or sometimes diabetic nephropathy.
How Diabetes Damages the Kidneys
High blood sugar levels over many years harm the tiny blood vessels in the kidneys. These blood vessels are called glomeruli. They act like sieves, allowing waste to pass into the urine while keeping useful proteins and other important substances in the blood. When the glomeruli are injured, they start to “leak.” Proteins such as albumin escape into the urine. This is one of the first signs of diabetic kidney disease.
The damage does not happen overnight. In the early stages, kidney disease may have no symptoms. Many people feel fine even while their kidneys are being harmed. As the damage continues, the kidneys lose their ability to filter properly. Waste products build up in the blood, and symptoms like swelling in the legs, fatigue, or changes in urination may appear. If the process continues unchecked, it can eventually lead to chronic kidney disease (CKD) and even kidney failure, which may require dialysis or a kidney transplant.
The Role of High Blood Pressure and Obesity
Kidney health in diabetes is influenced not only by blood sugar but also by blood pressure and body weight. High blood pressure is very common in people with type 2 diabetes. Extra pressure inside the blood vessels of the kidneys speeds up injury to the glomeruli. Over time, this worsens kidney disease. Doctors often prescribe blood pressure–lowering medications like ACE inhibitors or ARBs to help protect the kidneys.
Obesity adds another layer of strain. Extra body fat causes inflammation and hormone changes that stress the kidneys. It can also make blood sugar and blood pressure harder to control. Together, these factors create a cycle that increases the risk of kidney damage.
Why Kidney Disease in Diabetes Matters
Kidney disease is more than just a complication of diabetes. It is also a powerful predictor of poor health outcomes. People with diabetic kidney disease are much more likely to develop heart disease and strokes. In fact, most patients with kidney disease do not die from kidney failure itself, but from cardiovascular complications linked to it. This is why doctors often talk about “cardio-renal” health — meaning the heart and kidneys are closely connected.
Kidney disease also greatly affects quality of life. As kidney function drops, patients may need frequent doctor visits, more medications, and sometimes dialysis. Dialysis can take many hours each week and can cause fatigue, infections, and other complications. Preventing or delaying kidney disease is therefore one of the most important goals in diabetes care.
The Hidden Nature of Early Kidney Damage
One of the challenges is that early kidney damage is silent. Unlike chest pain in heart disease or vision changes in eye disease, kidney disease can advance for years without symptoms. By the time patients feel sick, the kidneys are often already severely impaired. Because of this, doctors recommend regular screening for urine albumin and blood creatinine levels in people with diabetes. These tests help catch kidney injury early, when it may still be slowed or reversed.
The Need for Protective Treatments
Given the high risks, treatments that can protect kidney health are urgently needed. Traditional strategies include tight control of blood sugar, lowering blood pressure, and using kidney-protective medications. In recent years, new classes of diabetes drugs, like SGLT2 inhibitors and GLP-1 receptor agonists, have shown benefits for kidney function. Tirzepatide, as a newer therapy that targets both GIP and GLP-1 receptors, is being studied to see if it can provide similar or even stronger kidney protection. This is why researchers and patients alike are interested in how tirzepatide affects kidney health.
The kidneys are a major concern in diabetes because they are highly sensitive to long-term injury from high blood sugar, high blood pressure, and obesity. Diabetic kidney disease is common, dangerous, and often silent until advanced. It increases the risk of heart disease, dialysis, and early death. For these reasons, protecting the kidneys is a key goal in diabetes management. New treatments like tirzepatide are being studied not only for their effects on blood sugar and weight, but also for their potential to safeguard kidney health.

Does Tirzepatide Affect Kidney Function?
When people with type 2 diabetes think about starting a new medicine, one of the first questions they often ask is: Will this drug hurt my kidneys, or will it help them? This is a very important question because diabetes is the leading cause of kidney disease worldwide. Many people with diabetes already have reduced kidney function, so doctors need to know if a new treatment like tirzepatide is safe for the kidneys.
Understanding Kidney Function in Diabetes
The kidneys are small organs, but they do a big job. They filter waste, balance water and electrolytes, and help regulate blood pressure. Diabetes, especially when blood sugar is high over time, can damage these filters. The result can be chronic kidney disease (CKD). Doctors track kidney function with tests such as:
- eGFR (estimated glomerular filtration rate): shows how well kidneys filter blood. A lower number means weaker kidney function.
- Albuminuria (protein in urine): shows if kidneys are leaking protein, an early sign of kidney damage.
These markers help researchers measure how a medicine affects the kidneys.
Evidence From Clinical Trials
Tirzepatide has been studied in large clinical trials called the SURPASS studies, which tested its effect on blood sugar, weight, and safety. In these trials, kidney health was not always the main focus, but researchers did track kidney-related results.
So far, results suggest that tirzepatide may not cause harm to kidney function. In fact, early data shows possible benefits:
- Slowing decline in eGFR: In some patients, tirzepatide appeared to slow down the drop in kidney function compared with other diabetes medicines.
- Reducing albuminuria: Some studies showed fewer patients developed protein in the urine while on tirzepatide.
These effects are important because keeping kidneys healthy means lower chances of dialysis or kidney transplant in the future.
Comparison to Other Medicines
Tirzepatide works differently from older diabetes drugs. For example:
- Metformin is safe for the kidneys but cannot be used in advanced kidney disease.
- SGLT2 inhibitors (like empagliflozin) have strong kidney-protective effects and are now recommended for many people with diabetes and CKD.
- GLP-1 receptor agonists (like semaglutide) have shown kidney benefits as well.
Tirzepatide combines GIP and GLP-1 activity, and early results suggest it may give similar or even stronger protection than GLP-1–only drugs. Still, long-term studies are ongoing to confirm this.
Mechanisms: Why Tirzepatide May Help Kidneys
There are several reasons why tirzepatide might protect kidney function:
- Lowering blood sugar: High blood sugar directly damages kidney filters. Tirzepatide helps keep glucose under control.
- Weight loss: Extra weight puts strain on kidneys. Tirzepatide often leads to significant weight loss, which can ease this burden.
- Blood pressure improvement: High blood pressure is another major cause of kidney damage. Weight loss and improved metabolic health with tirzepatide can lower blood pressure.
- Reduced inflammation: Research suggests incretin-based drugs may reduce harmful inflammation in the body, including in the kidneys.
Together, these effects may explain why kidney outcomes appear better with tirzepatide than with some other medicines.
Addressing Safety Concerns
The question many patients ask is: Can tirzepatide cause kidney damage? Based on current research, the answer is no. There is no evidence that tirzepatide directly injures the kidneys. However, there are two points to keep in mind:
- Dehydration risk: Tirzepatide can cause nausea, vomiting, or diarrhea in some people. If these symptoms are severe and lead to dehydration, kidney function can temporarily get worse. This is not because the drug harms the kidneys directly, but because dehydration lowers blood flow to the kidneys.
- Monitoring needed: For people with kidney problems, doctors usually check kidney blood tests (eGFR) and urine tests regularly to be safe.
What This Means for Patients
For now, the data is encouraging. Tirzepatide seems safe for most people with diabetes, including those with mild to moderate kidney disease. It may even slow the progression of diabetic kidney disease. However, more evidence is needed from long-term studies before we can be certain about its protective effects.
Patients should:
- Stay hydrated while on tirzepatide, especially if they experience stomach side effects.
- Tell their doctor about any history of kidney disease.
- Have regular kidney blood and urine tests while taking the medication.
Tirzepatide does not appear to damage the kidneys. On the contrary, early studies show it might protect them by lowering blood sugar, reducing weight, and improving overall metabolic health. While it is not yet proven to be a “kidney drug” like SGLT2 inhibitors, it holds promise as part of a treatment plan to protect long-term kidney function in people with diabetes.
Can Tirzepatide Help Prevent or Slow Diabetic Kidney Disease?
Diabetic kidney disease, also called diabetic nephropathy, is one of the most serious long-term complications of type 2 diabetes. Over time, high blood sugar damages the small blood vessels in the kidneys. This makes it harder for the kidneys to filter waste products and keep the right balance of fluid and minerals in the body. If not managed, the damage can progress to chronic kidney disease (CKD) or even kidney failure. Because diabetes is the leading cause of kidney failure worldwide, any treatment that may slow or prevent kidney disease is extremely important.
Tirzepatide, a new medicine for type 2 diabetes, is being studied for its possible benefits beyond lowering blood sugar. Researchers are especially interested in whether it can protect the kidneys. While we do not yet have final answers from long-term studies, early evidence gives reasons to be hopeful.
Evidence From Clinical Trials
The SURPASS clinical trial program tested tirzepatide in thousands of people with type 2 diabetes. These studies mainly focused on blood sugar control and weight loss, but researchers also collected information about kidney health.
In these trials, people taking tirzepatide showed lower levels of albumin in the urine (albuminuria). Albumin is a protein that leaks into the urine when the kidneys are damaged. Reducing albuminuria is seen as a positive sign because it often predicts slower kidney decline.
Another encouraging finding was that tirzepatide users had slower declines in estimated glomerular filtration rate (eGFR) compared to those taking other diabetes medicines. eGFR is a measure of kidney function, and keeping this number stable is key to avoiding kidney failure.
While these results are early and based on shorter-term data, they suggest that tirzepatide may indeed help preserve kidney health.
How Tirzepatide Might Protect the Kidneys
There are several reasons why tirzepatide could reduce the risk or slow the progression of diabetic kidney disease:
- Better Blood Sugar Control
High blood sugar is the main driver of diabetic kidney damage. Tirzepatide has been shown to lower blood sugar more than many other medications, including some GLP-1 receptor agonists. By keeping glucose closer to normal, the kidneys are exposed to less harm over time. - Weight Loss
Extra body weight increases the workload on the kidneys. Tirzepatide often leads to significant weight loss—sometimes more than 20% of body weight in certain patients. This reduces pressure on the kidneys, lowers inflammation, and may slow disease progression. - Lower Blood Pressure
High blood pressure is another major cause of kidney damage. Some studies show that tirzepatide modestly lowers blood pressure. Even small reductions can add up to meaningful benefits for kidney health. - Reduced Inflammation and Oxidative Stress
In diabetes, inflammation and stress from unstable molecules called free radicals can damage kidney cells. Animal studies suggest incretin-based therapies like tirzepatide may calm inflammation and reduce oxidative stress, giving kidneys further protection.
How It Compares With Other Treatments
Other medicines, such as SGLT2 inhibitors and GLP-1 receptor agonists, have already shown kidney-protective effects in large outcome trials. Since tirzepatide works on both GIP and GLP-1 receptors, researchers believe it could provide equal or possibly greater benefits.
However, unlike SGLT2 inhibitors, tirzepatide does not directly act on the kidneys to increase urine glucose excretion. Its benefits are more indirect—through lowering blood sugar, body weight, and blood pressure. This means it may be best used together with other kidney-protective drugs rather than as a replacement.
Need for Long-Term Studies
Even though the early data is promising, it is important to remember that most of the tirzepatide kidney findings so far come from secondary outcomes—meaning the trials were not designed to focus mainly on kidney health.
Large, long-term trials that specifically look at kidney failure, dialysis, and transplant outcomes are still underway. Until those are complete, doctors cannot say for certain that tirzepatide prevents kidney disease progression.
Still, the signs point in the right direction: better glucose control, lower albuminuria, slower eGFR decline, and added benefits from weight loss and blood pressure reduction.
So, can tirzepatide help prevent or slow diabetic kidney disease? The answer is: likely yes, but more proof is needed.
The combination of improved blood sugar, reduced body weight, lower blood pressure, and possible anti-inflammatory effects all support a kidney-protective role. Early clinical trial data shows positive signals, but larger and longer studies are required to confirm how strong and lasting these benefits will be.
What Are the Risks of Tirzepatide for Patients With Kidney Impairment?
Kidney disease is very common in people who have type 2 diabetes. Many patients who could benefit from new medicines, like tirzepatide, also have some level of kidney damage. Because of this, it is important to ask if tirzepatide is safe for people whose kidneys do not work at full strength. This section explains what the research shows about the risks, how dosing works, and what doctors should watch for when prescribing tirzepatide to patients with kidney problems.
Understanding Kidney Impairment
Kidney impairment is usually described in stages based on how well the kidneys filter the blood. Doctors measure this using a number called estimated glomerular filtration rate (eGFR):
- Stage 1–2 CKD: Mild impairment. Kidneys still work fairly well.
- Stage 3 CKD: Moderate impairment. eGFR falls between 30–59 mL/min.
- Stage 4 CKD: Severe impairment. eGFR between 15–29 mL/min.
- Stage 5 CKD or ESRD: End-stage kidney disease. eGFR below 15 mL/min or on dialysis.
The more advanced the stage, the harder it is for the body to remove waste and drugs. Some medicines build up in the blood when the kidneys are weak, leading to harmful side effects. That is why researchers carefully test new diabetes drugs like tirzepatide in people with different kidney function levels.
Dosing of Tirzepatide in Kidney Disease
One of the first safety questions is whether people with kidney problems need a lower dose of tirzepatide. According to clinical trial data and the prescribing information, no dose adjustment is needed for people with mild, moderate, or even severe kidney impairment. This means that the same dose used in patients with normal kidney function can also be given to those with reduced function, at least down to stage 4 CKD.
The reason is that tirzepatide is not cleared mainly by the kidneys. Instead, the body breaks it down in a different way, and only a small part passes through the kidneys. Because of this, the drug does not build up to dangerous levels when kidney function is reduced.
Safety Data From Clinical Trials
Several studies have looked at tirzepatide in people with kidney impairment:
- SURPASS clinical trials: These large studies of people with type 2 diabetes included many patients who also had early or moderate CKD. The results showed that tirzepatide was effective at lowering blood sugar and body weight across all groups, including those with impaired kidney function. Importantly, no major increase in kidney-related side effects was seen.
- Dedicated pharmacology studies: Research testing tirzepatide in people with mild, moderate, and severe kidney impairment found that drug levels in the blood were similar to those in people with normal kidney function. This confirmed that dosing changes are not needed.
Together, these findings suggest that tirzepatide is safe to use in people with kidney problems up to severe CKD.
Risks and Monitoring in Kidney Disease Patients
Even though tirzepatide itself does not directly harm the kidneys, there are still risks to consider. Most of these risks are related to side effects that could indirectly stress the kidneys:
- Dehydration and Acute Kidney Injury (AKI): Tirzepatide can cause nausea, vomiting, or diarrhea in some patients. If these symptoms are severe, patients may lose too much fluid, leading to dehydration. Dehydration can temporarily reduce kidney function and, in some cases, trigger AKI.
- Risk management: Patients should be told to stay well hydrated, especially during the first weeks of treatment. If vomiting or diarrhea is severe, patients should contact their healthcare team right away. Doctors may pause tirzepatide until the patient recovers.
- Risk management: Patients should be told to stay well hydrated, especially during the first weeks of treatment. If vomiting or diarrhea is severe, patients should contact their healthcare team right away. Doctors may pause tirzepatide until the patient recovers.
- Changes in Lab Tests: Kidney patients already have regular bloodwork to monitor eGFR and electrolytes. With tirzepatide, doctors may want to continue close monitoring, especially in those with stage 3 or 4 CKD, to watch for changes in kidney function after starting the drug.
- Drug Combinations: Many patients with diabetes and kidney disease are also prescribed ACE inhibitors, ARBs, or diuretics. These drugs protect the kidneys and heart but can sometimes affect hydration and blood pressure. When combined with tirzepatide, the risk of dehydration or low blood pressure may increase. Careful monitoring reduces these risks.
Is Tirzepatide Safe for Stage 3 CKD?
Stage 3 CKD (moderate impairment) is one of the most common scenarios doctors see. Patients at this stage are at high risk for both worsening kidney disease and cardiovascular events. Current evidence suggests that tirzepatide is safe and effective in stage 3 CKD. Clinical trials have shown strong improvements in blood sugar and weight loss without added kidney toxicity in these patients.
Doctors do not need to adjust the dose, but they should watch for dehydration, check labs regularly, and adjust other medications if needed.
Is Tirzepatide Safe in People on Dialysis or With Advanced CKD?
Chronic kidney disease (CKD) is a long-term condition where the kidneys slowly lose their ability to filter blood. When CKD reaches advanced stages (stage 4 or 5), kidney function is severely reduced. In stage 5, often called end-stage kidney disease, many patients require dialysis to survive. Dialysis is a medical process that removes waste, salt, and extra water from the blood when the kidneys can no longer do this on their own.
People with advanced CKD or on dialysis have complex health needs. They often also live with type 2 diabetes, high blood pressure, and heart problems. Because of this, any new treatment—like tirzepatide—must be studied carefully in this group to make sure it is both safe and effective.
What Clinical Trials Tell Us So Far
Tirzepatide has been studied in large groups of people with type 2 diabetes, including some with reduced kidney function. However, most clinical trials excluded patients with the most advanced stages of kidney disease or those already on dialysis. This means the available evidence is limited.
In the SURPASS trials, tirzepatide was tested in people with type 2 diabetes and different levels of kidney function. The results showed that tirzepatide worked well in lowering blood sugar and helping with weight loss, even in people with mild to moderate CKD. Importantly, there was no strong signal that the medicine harmed kidney function in these groups.
But when it comes to patients on dialysis, the data is much more scarce. Only small numbers of patients with severe kidney disease or dialysis have been exposed to tirzepatide in research so far. This leaves doctors and patients without clear guidance from large-scale, long-term studies.
Why Evidence Is Limited in Dialysis Patients
There are a few reasons why studies often exclude people on dialysis:
- Medical complexity – People on dialysis usually take many other medicines and often have other health conditions, making results harder to interpret.
- Safety concerns – Researchers are cautious about testing new drugs in very fragile patients until more is known.
- Drug handling in the body – Some medicines are filtered by the kidneys. For these drugs, impaired kidney function can cause buildup in the blood. With tirzepatide, this concern appears to be less severe, but more research is needed.
How Tirzepatide Behaves in Severe CKD
One important question is whether tirzepatide levels build up in the blood of people with kidney failure. Early pharmacology studies suggest that tirzepatide is not heavily removed by the kidneys. Instead, it is broken down by proteins in the body and cleared in other ways. Because of this, tirzepatide does not appear to require dose adjustment in people with mild, moderate, or even severe CKD.
For dialysis patients, it is still not clear if dialysis itself removes tirzepatide from the bloodstream. Current knowledge suggests it is unlikely to be cleared significantly by dialysis, but more studies are needed to be certain.
Practical Considerations for Advanced CKD and Dialysis
Even though the available evidence looks reassuring, there are still practical issues that doctors must consider when prescribing tirzepatide for people with advanced CKD or on dialysis:
- Gastrointestinal side effects: Tirzepatide can cause nausea, vomiting, and diarrhea, especially during the first months of treatment. In dialysis patients, these symptoms may increase the risk of dehydration, which can make kidney and heart problems worse.
- Nutritional needs: Many dialysis patients already struggle to maintain proper nutrition. Rapid weight loss or poor appetite caused by tirzepatide may be risky for some individuals.
- Blood sugar control: Tirzepatide is effective at lowering blood sugar, but dialysis patients often have fluctuating glucose levels. This requires close monitoring to avoid hypoglycemia.
- Medication interactions: Dialysis patients are usually on multiple medications, including phosphate binders, blood pressure drugs, and heart medicines. While tirzepatide has no major known drug–drug interactions, doctors must remain cautious.
Current Guidance for Patients and Clinicians
Because there is not enough strong evidence yet, most guidelines say tirzepatide can be used with caution in people with advanced CKD but should be prescribed carefully. For those on dialysis, it is not formally contraindicated, but doctors must weigh risks and benefits on an individual basis.
This usually means:
- Starting at the lowest available dose and adjusting slowly.
- Careful monitoring for dehydration and gastrointestinal problems.
- Checking weight and nutrition status regularly.
- Frequent blood sugar testing to prevent severe lows.
At present, tirzepatide looks safe for people with diabetes and moderate kidney disease, and it does not appear to need dose adjustment in most cases. However, for people on dialysis or with advanced CKD, the evidence is limited. Clinical trials so far do not provide clear answers.
Until larger studies are done, doctors should use tirzepatide with caution in these patients. Close monitoring, specialist input from nephrologists (kidney doctors), and open discussions with patients about risks and benefits are essential.
Tirzepatide may become an important option for managing diabetes and protecting kidney health, but for now, patients on dialysis or with very advanced CKD remain a group where more evidence is urgently needed.
Does Tirzepatide Interact With Other Kidney-Related Medications?
When doctors treat people with diabetes who also have kidney disease, it is common for patients to take more than one medicine. These medicines often work together to lower blood sugar, protect the kidneys, and reduce the risk of heart problems. Because tirzepatide is a newer medicine, many people ask if it interacts with other common drugs used for kidney health. Let’s look closely at how tirzepatide fits into the bigger picture of diabetes and kidney care.
Common Kidney-Related Medications in Diabetes
Many people with diabetes and kidney disease take medicines that directly protect kidney function. The most common groups are:
- ACE inhibitors (angiotensin-converting enzyme inhibitors) – Examples include lisinopril and enalapril. They help lower blood pressure and reduce the strain on the kidneys.
- ARBs (angiotensin receptor blockers) – Examples include losartan and valsartan. These are often used if a patient cannot take ACE inhibitors. Like ACE inhibitors, they reduce protein loss in the urine and slow kidney disease.
- SGLT2 inhibitors (sodium-glucose cotransporter-2 inhibitors) – Examples include empagliflozin and dapagliflozin. These medicines lower blood sugar by helping the body pass glucose in the urine. They also reduce kidney disease progression and lower the risk of hospitalization for heart failure.
- Diuretics (water pills) – These help control blood pressure and swelling by removing extra fluid.
It is important to know whether tirzepatide affects how these medicines work.
Evidence for Interactions Between Tirzepatide and ACE Inhibitors or ARBs
So far, studies show no major drug–drug interaction between tirzepatide and either ACE inhibitors or ARBs. This means tirzepatide does not change how these medicines are absorbed, broken down, or cleared from the body. Both groups of drugs can be used safely together. In fact, because tirzepatide helps with weight loss and blood sugar control, it may indirectly make ACE inhibitors and ARBs even more effective at protecting kidney health.
For example, high blood pressure and uncontrolled diabetes are two main causes of kidney decline. By lowering blood sugar and supporting weight loss, tirzepatide reduces stress on the kidneys. ACE inhibitors and ARBs reduce blood pressure inside the kidney’s small blood vessels. Together, they may provide stronger protection against kidney damage.
Tirzepatide and SGLT2 Inhibitors: Are They Synergistic?
SGLT2 inhibitors are now a standard part of care for people with diabetes and chronic kidney disease. One common question is whether patients can take tirzepatide and an SGLT2 inhibitor at the same time. The answer is yes, and research suggests that this combination may be especially powerful.
Both medicines lower blood sugar but in different ways. Tirzepatide works by increasing insulin release and reducing appetite, while SGLT2 inhibitors remove glucose through the urine. Because they use different pathways, the combination has an additive effect without creating harmful overlap.
More importantly, both medicines have shown benefits beyond blood sugar control. SGLT2 inhibitors have strong evidence for protecting kidney function and reducing heart failure risk. Tirzepatide has shown early promise in reducing albuminuria (protein in urine) and slowing kidney decline. Using both together could mean broader kidney and heart protection. Large clinical trials are ongoing to confirm these combined benefits.
Diuretics and Dehydration Risk
Another group of medicines often used in people with kidney disease is diuretics. Since tirzepatide can sometimes cause nausea, vomiting, or diarrhea, there is a small risk of dehydration. Diuretics also increase fluid loss. When combined, these effects could raise the chance of dehydration or low blood pressure. This does not mean they cannot be used together, but doctors usually watch patients closely for signs of dehydration. Drinking enough fluids and checking kidney function with blood tests are important steps.
No Major Pharmacological Interactions
So far, research shows that tirzepatide does not directly interfere with how other kidney medicines are processed in the body. It does not speed up or slow down the liver enzymes or kidney pathways that handle most drugs. This is important, because it means the chance of harmful drug–drug interactions is low.
Still, the way medicines affect each other in real life can be more complex. For example, if tirzepatide causes a patient to eat less or lose weight quickly, the body may respond differently to blood pressure medicines. This is why ongoing monitoring is needed.
Clinical Monitoring and Physician Oversight
Even though no major interactions are known, doctors usually recommend close monitoring when starting tirzepatide in patients who already take ACE inhibitors, ARBs, SGLT2 inhibitors, or diuretics. Monitoring may include:
- Checking kidney function with blood tests (creatinine and eGFR).
- Measuring blood pressure regularly.
- Watching for dehydration, especially if stomach side effects occur.
- Adjusting doses of other medicines if needed.
This careful follow-up helps ensure that the benefits of tirzepatide are maximized without unexpected side effects.
Tirzepatide can be safely combined with the main kidney-protective medicines used in diabetes. There are no major drug–drug interactions with ACE inhibitors, ARBs, or SGLT2 inhibitors. In fact, combining tirzepatide with these medicines may improve outcomes by addressing different causes of kidney damage. The main caution is when tirzepatide is used alongside diuretics, since both can increase the risk of dehydration. For this reason, regular monitoring and guidance from a healthcare team are essential.
Tirzepatide fits well into the standard treatment plan for people with diabetes and kidney disease. It appears safe to use with other kidney medications and may even provide stronger protection when used together. The future looks promising as researchers continue to study the combined benefits of tirzepatide with other therapies.
Does Tirzepatide Increase the Risk of Acute Kidney Injury (AKI)?
When people hear about new medicines like tirzepatide, one of the first questions they ask is whether it is safe for the kidneys. This is especially important for patients with diabetes, because kidney disease is already a common complication. In this section, we will carefully explain what doctors know about tirzepatide and the risk of acute kidney injury (AKI). We will look at why side effects of tirzepatide could sometimes stress the kidneys, what the research shows so far, and how doctors reduce risks for patients.
What Is Acute Kidney Injury (AKI)?
Acute kidney injury means that the kidneys suddenly stop working as well as they should. This problem often develops over hours or days. AKI can be mild and temporary, or it can become very serious and require hospital treatment.
Common causes of AKI include:
- Dehydration (not enough fluid in the body)
- Low blood pressure
- Certain medications that strain the kidneys
- Severe illness or infection
For people with diabetes or kidney disease, the risk of AKI is already higher than in the general population. That is why any new diabetes medicine must be studied for its kidney safety.
Why Might Tirzepatide Be Linked to Kidney Problems?
Tirzepatide is not directly toxic to the kidneys. Instead, the concern about AKI mostly comes from side effects that can affect body fluids. Like other medicines in its class, tirzepatide often causes:
- Nausea
- Vomiting
- Diarrhea
These side effects are usually mild and improve with time. But if they are severe or last too long, they can lead to dehydration. When dehydration happens, the kidneys may not receive enough blood flow, which can trigger AKI.
In medical safety reports, cases of AKI linked to GLP-1 medicines often involved patients who became very dehydrated because of stomach problems. Doctors believe the same risk applies to tirzepatide.
What Do Studies Show About Tirzepatide and AKI?
Large clinical trials of tirzepatide, such as the SURPASS studies, did not show high rates of acute kidney injury. Most participants did not experience serious kidney problems. However, a few reports of AKI have appeared in post-marketing safety data and real-world use. These reports usually happened in patients who:
- Already had chronic kidney disease
- Were taking other medicines that affect fluid balance (like diuretics)
- Had severe vomiting or diarrhea and did not replace lost fluids
So far, there is no evidence that tirzepatide itself damages the kidneys. Instead, the connection to AKI seems to be indirect, related to dehydration or other health conditions.
Risk Mitigation: How Doctors Reduce the Chance of AKI
Doctors take several steps to protect patients’ kidneys while they are on tirzepatide:
- Start with a low dose
- Tirzepatide is introduced at a small dose and increased slowly. This helps the body adjust and lowers the risk of nausea, vomiting, or diarrhea.
- Tirzepatide is introduced at a small dose and increased slowly. This helps the body adjust and lowers the risk of nausea, vomiting, or diarrhea.
- Encourage hydration
- Patients are advised to drink enough fluids every day. Staying hydrated keeps blood flow to the kidneys stable.
- Patients are advised to drink enough fluids every day. Staying hydrated keeps blood flow to the kidneys stable.
- Monitor kidney function
- In patients with chronic kidney disease or those at higher risk, doctors check kidney blood tests (such as eGFR and creatinine) regularly.
- In patients with chronic kidney disease or those at higher risk, doctors check kidney blood tests (such as eGFR and creatinine) regularly.
- Pause tirzepatide during acute illness
- If a patient develops a stomach virus, food poisoning, or another illness that causes dehydration, doctors may temporarily stop tirzepatide until the patient is better.
- If a patient develops a stomach virus, food poisoning, or another illness that causes dehydration, doctors may temporarily stop tirzepatide until the patient is better.
- Review other medications
- Some drugs, like diuretics or nonsteroidal anti-inflammatory drugs (NSAIDs), also increase AKI risk. Doctors may adjust these when a patient is on tirzepatide.
- Some drugs, like diuretics or nonsteroidal anti-inflammatory drugs (NSAIDs), also increase AKI risk. Doctors may adjust these when a patient is on tirzepatide.
Who Is Most at Risk?
Not all patients face the same level of risk. Those at highest risk of tirzepatide-related AKI include:
- People with advanced chronic kidney disease
- Elderly patients, who are more prone to dehydration
- Patients taking diuretics for high blood pressure or heart failure
- Patients who experience persistent vomiting or diarrhea on tirzepatide
For these groups, doctors will be extra cautious and monitor more closely.
At this stage, the evidence suggests tirzepatide is not a major cause of acute kidney injury, but it can indirectly increase the risk if patients become dehydrated. The good news is that most cases can be prevented by careful monitoring, patient education, and early action if stomach side effects become severe. As longer-term studies continue, researchers will gain more detailed information about tirzepatide’s safety profile for the kidneys.
What Do Long-Term Studies Suggest About Kidney Health and Tirzepatide?
Tirzepatide is still a fairly new medicine, so most of the studies we have today are short- or medium-term. These studies usually last one to two years and focus on blood sugar, weight loss, and heart health. But because diabetes often damages the kidneys over many years, researchers are now watching closely to see if tirzepatide has long-term effects—either positive or negative—on kidney health.
This section explains what we know so far, what ongoing research is looking at, and what people with diabetes and kidney concerns should understand about tirzepatide’s future outlook.
Early Signs From Clinical Trials
The main studies that tested tirzepatide are called the SURPASS trials. These were large studies that included thousands of people with type 2 diabetes. While the main goals were to check how well tirzepatide lowered blood sugar and body weight, the researchers also looked at markers of kidney health.
One key measure was eGFR (estimated glomerular filtration rate), which shows how well the kidneys are filtering waste. Another important measure was albuminuria, which is the leakage of protein into the urine—a common sign of early kidney damage.
In these studies, people taking tirzepatide often showed:
- Less protein in the urine compared with those on insulin or other medicines.
- Stable kidney function over the study period, with some signs that decline in eGFR slowed down.
These early signals suggest tirzepatide might protect the kidneys in the long run. However, because the trials were not designed specifically for kidney outcomes, the data are still considered early and not final.
Why Might Tirzepatide Help the Kidneys?
Researchers believe tirzepatide may protect the kidneys in several ways:
- Better blood sugar control – High blood sugar damages the small blood vessels in the kidneys. Tirzepatide lowers blood sugar more than many older diabetes medicines.
- Weight loss – Extra weight increases kidney strain. People on tirzepatide often lose 15–20% of their body weight, which can reduce kidney stress.
- Lower blood pressure – High blood pressure is another major driver of kidney damage. Weight loss and metabolic changes from tirzepatide may reduce blood pressure, giving the kidneys a break.
- Direct effects on kidney tissue – GLP-1 receptor drugs (like semaglutide) have shown anti-inflammatory and protective effects on kidney cells. Since tirzepatide also activates GLP-1 receptors, it may share these benefits.
These combined effects explain why researchers are hopeful about tirzepatide’s role in long-term kidney protection.
Ongoing Studies Looking at Kidney Outcomes
Right now, several large studies are being planned or are already underway to give clearer answers:
- SURPASS-CVOT (Cardiovascular Outcomes Trial): This trial is mainly designed to test if tirzepatide reduces the risk of heart attack, stroke, and death. However, it also includes a kidney health substudy. This means researchers will track how kidney function changes over years, not just months.
- Real-world studies: Doctors are also collecting information from patients who are taking tirzepatide outside of clinical trials. These studies are important because they show how the drug works in everyday life, including in people with kidney disease at different stages.
It may take several more years before we have full results, but these studies will tell us if tirzepatide can truly slow or prevent diabetic kidney disease in the long term.
Should People With CKD Be Cautious?
So far, tirzepatide appears safe for people with mild to moderate kidney disease. The drug does not need dose adjustments in kidney impairment, unlike some other medicines.
However, people with advanced kidney disease, especially those on dialysis, should be cautious. There is not enough long-term research yet in these groups. Doctors usually recommend close monitoring with blood and urine tests when patients with CKD start tirzepatide.
For now, the key questions that ongoing studies aim to answer include:
- Can tirzepatide slow down the progression of kidney disease?
- Will it prevent dialysis or kidney failure in the long run?
- Is it safe to use in people with very low kidney function?
Long-Term Outlook
At this time, the long-term outlook for tirzepatide and kidney health is promising but not proven. Early evidence shows:
- Lower rates of protein leakage in urine.
- Slower decline in kidney function in trial participants.
- Added benefits from weight loss, blood sugar control, and blood pressure reduction.
Still, until the large outcome trials are completed, doctors and patients will need to rely on close monitoring and the growing body of real-world data.
Tirzepatide has shown encouraging early signs that it may help protect the kidneys in people with type 2 diabetes. Long-term studies are underway and will give clearer answers in the next few years. For now, people with diabetes and kidney concerns should discuss with their doctors whether tirzepatide may be a good choice for them, while understanding that more data is still coming.
Future Directions in Research and Clinical Practice
Tirzepatide is a new medicine that has already changed how doctors think about treating type 2 diabetes and obesity. The early research shows benefits not only for blood sugar and weight but also for heart and kidney health. Even so, doctors and scientists agree that more research is needed before we can fully understand its long-term effects, especially for people living with kidney disease. In this section, we will look at what the future may hold for tirzepatide in research and daily medical practice.
Large-Scale Outcome Trials Focusing on Kidney Health
One of the biggest needs right now is more data from large and long-term studies. The clinical trials we have so far, such as the SURPASS program, suggest that tirzepatide may slow kidney damage. For example, patients using tirzepatide had less albumin in their urine, which is an early sign of kidney strain. They also showed slower loss of estimated glomerular filtration rate (eGFR), a key measure of kidney function.
However, these studies were not designed to test kidney outcomes as their main goal. The focus was more on blood sugar and body weight. Future trials are being planned and some are already underway that will study tirzepatide with kidney outcomes as the main target. These trials will track patients for several years and look at whether tirzepatide can actually reduce the number of people who develop serious kidney disease or need dialysis.
Such trials are important because they can give stronger answers than smaller studies. Doctors and patients will want to know if tirzepatide not only manages diabetes but also protects kidneys in the same way that other medicines, such as SGLT2 inhibitors, have been proven to do.
Combining Tirzepatide With Other Kidney-Protective Drugs
Another area of future practice is how tirzepatide may work when combined with other medications. Right now, SGLT2 inhibitors and ACE inhibitors or ARBs are widely used to protect the kidneys in people with diabetes. These drugs have strong evidence for reducing kidney failure and heart problems.
Since tirzepatide works in a different way, doctors are interested in whether using it together with SGLT2 inhibitors or ACE inhibitors will give extra protection. Early research suggests that the effects might add up, giving better results than either drug alone. For example, tirzepatide lowers weight, blood sugar, and blood pressure, while SGLT2 inhibitors reduce stress on the kidney filters and lower risk of heart failure.
Future studies will need to test these combinations directly. If the results are positive, then using tirzepatide alongside these medicines could become standard care for people at high risk of kidney disease. This would represent a new level of protection, especially for patients with diabetes who often face kidney, heart, and blood vessel problems at the same time.
Personalized Medicine Approaches
Medicine is moving toward a more personalized approach, and tirzepatide may become part of that shift. Not all patients with diabetes are the same. Some have faster progression of kidney disease. Some are more likely to have heart problems. Others may respond better to one drug than another.
Future research may help doctors identify which patients benefit most from tirzepatide. This could involve studying genetic markers, lifestyle factors, or patterns in lab tests. For example, patients who struggle with weight loss might gain more from tirzepatide’s strong effects on body weight. Others with higher levels of protein in their urine might respond better if tirzepatide truly protects the kidneys.
If doctors can predict who will get the most benefit, they can tailor treatment plans. This reduces the risk of side effects and makes the most of what the medicine can offer. Personalized care will likely become more common as more data is collected from real-world patients outside of clinical trials.
Expanding Research Beyond Diabetes
Another direction for future research is to see if tirzepatide could help people who do not have diabetes but are still at risk for kidney disease. Obesity, high blood pressure, and heart disease all increase the risk of kidney failure. Since tirzepatide lowers weight and blood pressure, it may also help these groups.
Some early studies are already testing tirzepatide in patients with obesity but without diabetes. If kidney benefits are also found in these groups, it could expand the use of tirzepatide and give doctors another tool to slow the rise of kidney disease in the general population.
Improving Patient Access and Monitoring
While research continues, doctors will also need to think about how to use tirzepatide safely in practice. One concern is cost and access. New medicines are often expensive, and patients may not have full insurance coverage. This can limit who gets the drug, even if it could help them. Over time, as more evidence builds and guidelines are updated, insurance systems may expand coverage.
Another important step is patient monitoring. Future practice will likely include clear guidelines on how to follow patients taking tirzepatide. This may involve checking kidney function tests at regular intervals, watching for signs of dehydration, and adjusting other medications as needed. With good monitoring, doctors can maximize benefits while reducing risks.
The future of tirzepatide in kidney health looks promising but still uncertain. Large outcome trials will show whether it can truly prevent or slow kidney disease. Combining tirzepatide with other proven kidney drugs may offer even greater protection. Personalized medicine may help doctors decide who benefits most. Research may expand beyond diabetes to obesity and other groups at risk for kidney problems. Finally, practical issues like cost, access, and monitoring will shape how tirzepatide is used in everyday care.
Conclusion
Tirzepatide is one of the newest medicines for people with type 2 diabetes, and its effects go beyond lowering blood sugar. As more people use this medicine, one of the most important questions is how it affects the kidneys. Diabetes is the leading cause of chronic kidney disease (CKD) worldwide. Protecting kidney health is critical because once kidneys are damaged, the condition is usually permanent, and people may need dialysis or a transplant. This makes it very important to look at whether tirzepatide can protect the kidneys, whether it carries risks, and what the future may hold.
From the evidence we have so far, tirzepatide shows promise in protecting kidney function in people with diabetes. Clinical studies, especially the SURPASS program, show improvements in markers that are linked with kidney health. These include reductions in albuminuria, which means less protein leaking into the urine, and slower declines in estimated glomerular filtration rate (eGFR), which is the main measure of how well the kidneys filter waste. Both of these findings suggest that tirzepatide may help delay the development or progression of diabetic kidney disease. This protective effect seems to come from several factors: strong blood sugar control, significant weight loss, lower blood pressure, and improvements in inflammation. All of these are important for reducing stress on the kidneys.
At the same time, safety remains a key question. People with diabetes often have some level of kidney impairment already, and medicines need to be used carefully in this group. Based on current evidence, tirzepatide does not require dose changes in people with mild, moderate, or even severe kidney disease who are not yet on dialysis. This is an important advantage, since many diabetes medicines are limited or restricted once kidney function starts to decline. For people with advanced kidney disease or those on dialysis, the data are not as strong. There are fewer patients in this group in the clinical trials, so doctors have to use extra caution. More research is needed to understand how safe and effective tirzepatide is in patients with stage 4 CKD, stage 5 CKD, or those already on dialysis.
Another question is whether tirzepatide can cause harm to the kidneys. Like other medicines in its class, tirzepatide may cause side effects such as nausea, vomiting, or diarrhea. If these symptoms are severe, they can lead to dehydration. Dehydration can, in turn, cause acute kidney injury, which is a sudden drop in kidney function. The risk of this is not high, but it is something doctors and patients need to watch closely. Staying hydrated, monitoring lab tests, and pausing the medicine during episodes of severe illness can help reduce this risk. Importantly, there is no strong evidence at this time that tirzepatide directly damages the kidneys.
In the long run, the biggest question is whether tirzepatide can change the course of kidney disease in people with diabetes. Current evidence is encouraging, but large outcome trials are still ongoing. For example, trials that focus on cardiovascular and kidney outcomes will tell us more about how well tirzepatide protects the kidneys over years of use, not just months. These trials are also important because diabetes, kidney disease, and heart disease are all linked. Medicines that improve blood sugar, weight, blood pressure, and cholesterol at the same time may provide combined protection for both the heart and the kidneys.
Looking at the big picture, tirzepatide appears to be a strong option for people with type 2 diabetes who need better blood sugar control and who may also benefit from weight loss and possible kidney protection. The safety profile so far is favorable, and it seems usable across most stages of kidney disease, with extra care needed in advanced stages. At the same time, long-term answers are not here yet. Doctors and researchers need to keep studying how tirzepatide works in different kidney groups and how it interacts with other proven kidney-protective medicines, such as SGLT2 inhibitors and ACE inhibitors.
In summary, tirzepatide offers hope for a future where people with type 2 diabetes may have not only better blood sugar and weight control but also stronger kidney protection. For now, the medicine should be used with careful monitoring, especially in those who already have reduced kidney function. Patients should talk with their doctors about risks, benefits, and follow-up care. With ongoing research, the long-term outlook may confirm that tirzepatide is not only safe for the kidneys but also an important tool in slowing or preventing diabetic kidney disease.
Research Citations
Heerspink, H. J. L., Sattar, N., Pavo, I., Haupt, A., Duffin, K. L., Yang, Z., Wiese, R. J., Tuttle, K. R., & Cherney, D. Z. I. (2022). Effects of tirzepatide versus insulin glargine on kidney outcomes in type 2 diabetes in the SURPASS-4 trial: Post-hoc analysis of an open-label, randomised, phase 3 trial. The Lancet Diabetes & Endocrinology, 10(11), 774–785.
Heerspink, H. J. L., Sattar, N., Pavo, I., Haupt, A., Duffin, K. L., Yang, Z., Wiese, R. J., Wilson, J. M., Hemmingway, A., Cherney, D. Z. I., & Tuttle, K. R. (2023). Effects of tirzepatide versus insulin glargine on cystatin C–based kidney function: A SURPASS-4 post hoc analysis. Diabetes Care, 46(8), 1501–1506.
Apperloo, E. M., Tuttle, K. R., Pavo, I., Haupt, A., Taylor, R., Wiese, R. J., Hemmingway, A., Cherney, D. Z. I., Sattar, N., & Heerspink, H. J. L. (2025). Tirzepatide associated with reduced albuminuria in participants with type 2 diabetes: Pooled post hoc analysis from the randomized active- and placebo-controlled SURPASS-1–5 clinical trials. Diabetes Care, 48(3), 430–436.
Caruso, I., & Giorgino, F. (2024). Renal effects of GLP-1 receptor agonists and tirzepatide in individuals with type 2 diabetes: Seeds of a promising future. Endocrine, 84(3), 822–835.
Kamrul-Hasan, A., Patra, S., Dutta, D., Nagendra, L., Muntahi-Reza, A., Borozan, S., & Pappachan, J. M. (2025). Renal effects and safety of tirzepatide in subjects with and without diabetes: A systematic review and meta-analysis. World Journal of Diabetes, 16(2), 101282.
Karakasis, P., Stavridis, G., Kalaitzidis, R., Papatheodorou, K., & Karagiannis, T. (2024). Effect of tirzepatide on albuminuria levels and renal function in patients with type 2 diabetes mellitus: A systematic review and multilevel meta-analysis. Diabetes, Obesity and Metabolism, 26(3), 1090–1104.
Urva, S., Quinlan, T., Landry, J., Martin, J., & Loghin, C. (2021). Effects of renal impairment on the pharmacokinetics of the dual GIP and GLP-1 receptor agonist tirzepatide. Clinical Pharmacokinetics, 60(8), 1049–1059.
Bosch, C., Carriazo, S., Soler, M. J., Ortiz, A., & Fernandez-Fernandez, B. (2023). Tirzepatide and prevention of chronic kidney disease. Clinical Kidney Journal, 16(5), 797–808.
Chuang, M.-H., Chen, Y.-Y., Jiang, P., Wang, S.-H., & Wu, V.-C. (2024). Clinical outcomes of tirzepatide or GLP-1 receptor agonists in individuals with type 2 diabetes. JAMA Network Open, 7(8), e2427258.
Borlaug, B. A., et al. (2025). Effects of tirzepatide on circulatory overload and end-organ damage in heart failure with preserved ejection fraction and obesity: A secondary analysis of the SUMMIT trial. Nature Medicine, 31, advance online publication.
Questions and Answers: Tirzepatide Kidney
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. It is approved for type 2 diabetes and is being studied for obesity, cardiovascular, and kidney outcomes.
Yes. Clinical trials suggest tirzepatide slows the decline in estimated glomerular filtration rate (eGFR) and reduces albuminuria (protein in the urine), both of which are markers of kidney health.
Evidence indicates tirzepatide may reduce progression of CKD by improving blood sugar, lowering weight, and decreasing albuminuria. Ongoing outcome studies are evaluating its long-term kidney protection.
Tirzepatide improves glycemic control, reduces body weight, lowers blood pressure, and decreases albuminuria. These combined effects are believed to reduce kidney stress and damage.
Yes. Pharmacokinetic studies show tirzepatide can be used in patients with mild, moderate, or severe CKD, and even in end-stage renal disease, without dose adjustment. However, monitoring is still important.
Yes. Clinical data show tirzepatide reduces urinary albumin-to-creatinine ratio (UACR), a key measure of protein leakage in the urine, suggesting a kidney-protective effect.
In the SURPASS program, tirzepatide slowed eGFR decline and reduced progression to higher levels of albuminuria compared to insulin or placebo in patients with type 2 diabetes.
It is not yet proven, but ongoing cardiovascular and kidney outcome trials (such as SURPASS-CVOT) are evaluating whether tirzepatide reduces the risk of kidney failure, dialysis, or transplantation.
Like other GLP-1 RAs (e.g., semaglutide, liraglutide), tirzepatide shows kidney benefits, but early data suggest its dual GIP/GLP-1 mechanism may provide even stronger kidney protection.
Yes. Although no dose adjustment is required, clinicians should monitor kidney function (eGFR) and urine protein regularly, especially in patients with advanced CKD or those on diuretics, since dehydration can worsen kidney function.